Autoimmune thyroid disease (AITD), which includes Graves' disease (GD) and Hashimoto's thyroiditis (HT), affects an estimated 5% of the general population, making it one of the most prevalent autoimmune diseases[1].
Graves’ disease
What is Graves' disease?
Graves‘ disease is an immune system disorder that is the most common cause of hyperthyroidism.

Who is more likely to have Graves’ disease?
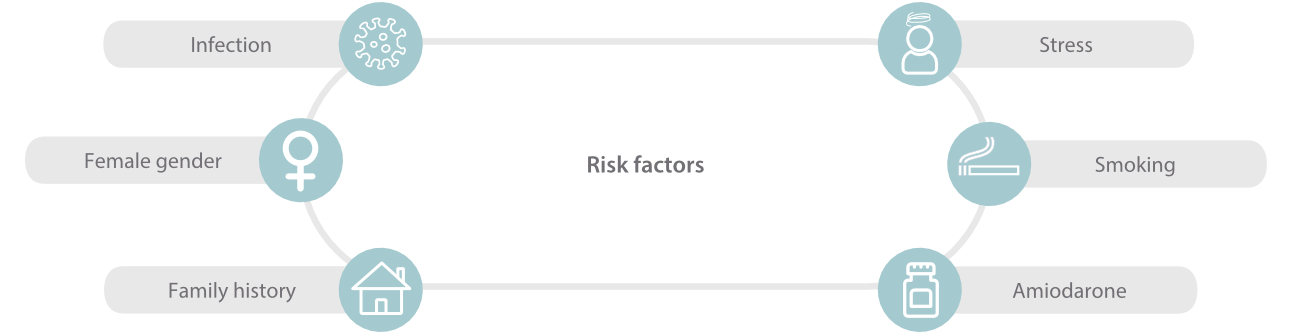
AITD is much more common in women than in men, with a female: male ratio ranging from 5:1 to 10:1[2]. Graves’ disease is more common in women, those older than age 30[3], and those with a family history of Graves’ or Hashimoto’s disease. Other autoimmune disorders, such as vitiligo, autoimmune gastritis, type 1 diabetes and rheumatoid arthritis, are associated with the use of nicotine products[4,5].
What are the symptoms and complications of Graves’ disease?
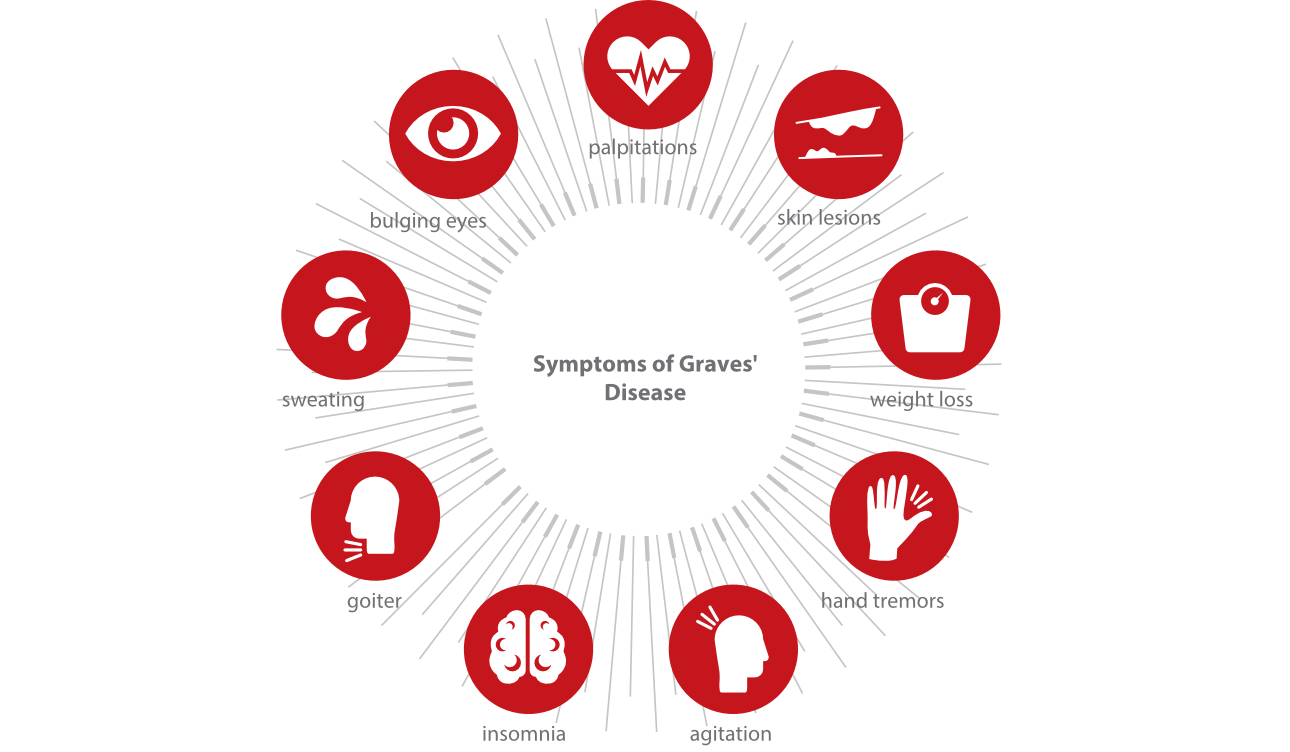
Graves' disease can cause hyperthyroidism and is characterized by increase in metabolic rate and increase in sympathetic activity[6.7].
How do doctors diagnose Graves’ disease?
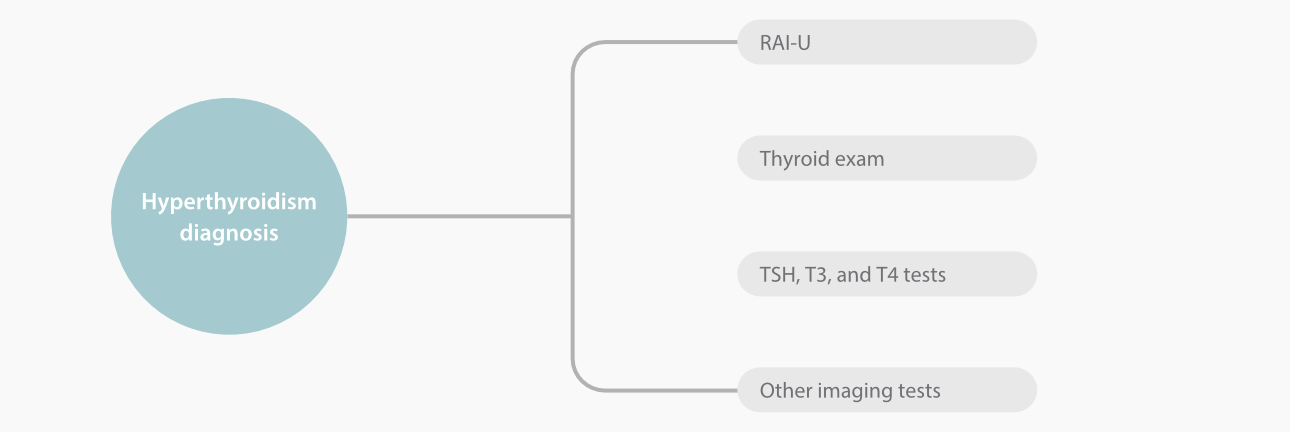
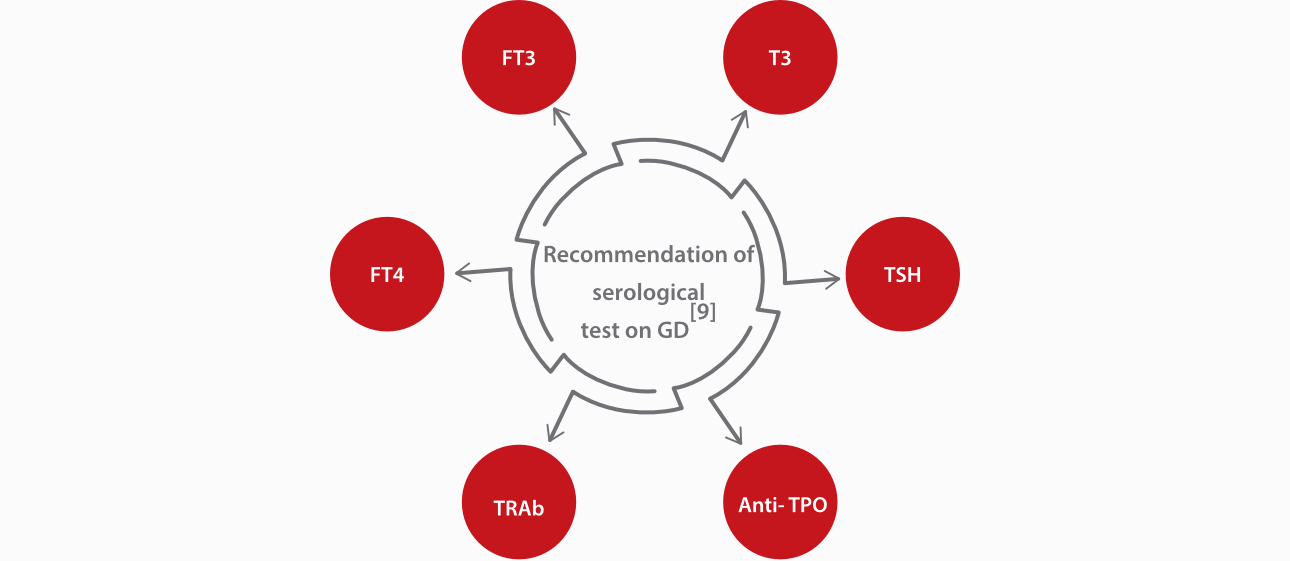
The diagnosis of hyperthyroidism is performed based on symptoms and physical signs and confirmed by a laboratory test. First, the levels of thyroid hormones (thyroxine/T4, and triiodothyronine/T3) and thyroid-stimulating hormone (TSH) in blood are measured, and then the levels of thyrotropin receptor antibodies (TRAbs) are measured, the elevation of which confirms the diagnosis of Graves’ disease.
A TRAb test helps to diagnose Graves' disease, but may confirm the diagnosis of toxic multinodular goiter. The test is also performed during the last three months of pregnancy to check a baby's risk of being born with Graves' disease or an overactive thyroid.
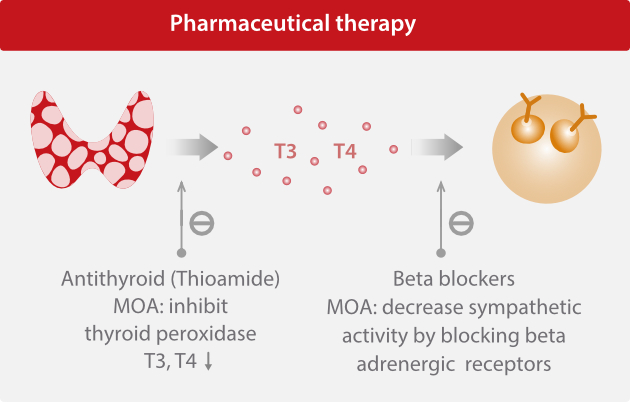
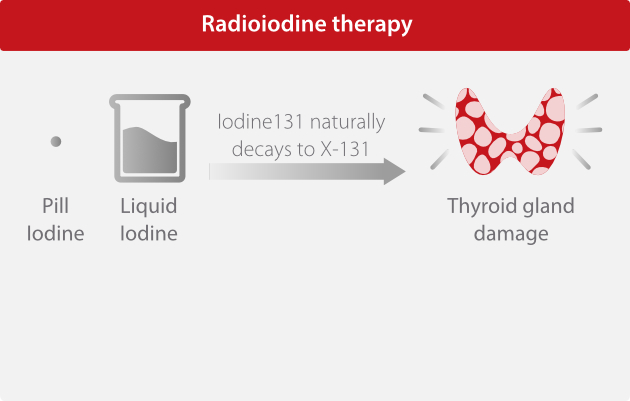
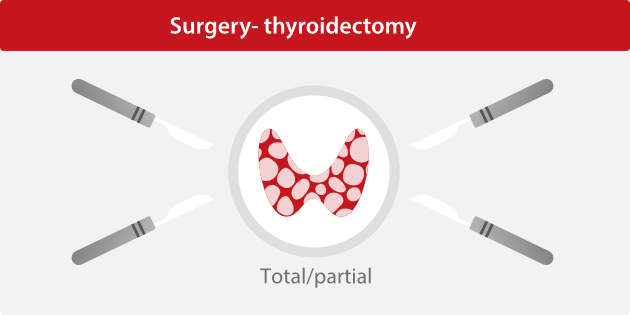
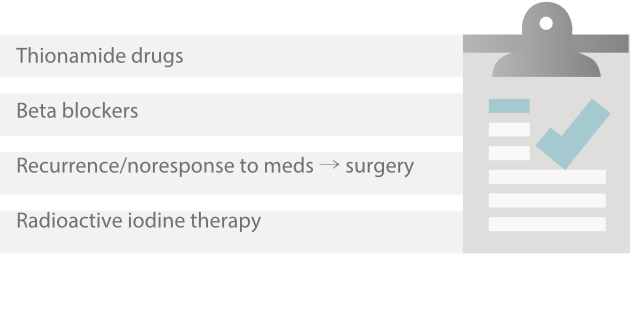
Graves' disease management
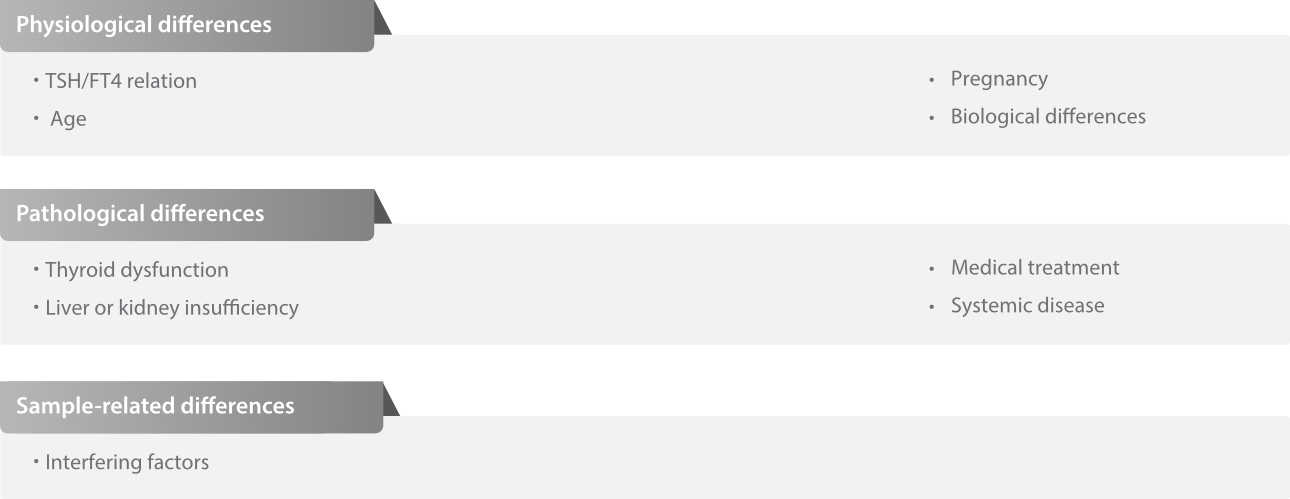
Some preanalytical factors should be considered when interpreting thyroid function results as they might be influenced by these factors[8].
Hashimoto’s thyroiditis
What is Hashimoto’s thyroiditis?[10-13]
Hashimoto’s thyroiditis, named after the Japanese physician Hakaru Hashimoto who first described it, belongs to a group of disorders where there is some form of inflammation “-itis” of the thyroid gland. It is basically an autoimmune destruction of the thyroid gland, which typically progresses gradually to hypothyroidism, or state of too low “hypo-“ thyroid hormones. In fact, Hashimoto’s thyroiditis is the most common cause of hypothyroidism in areas of the world where dietary iodine, the basic structural element of thyroid hormones, is sufficient.
Symptoms of Hashimoto’s Disease[14]
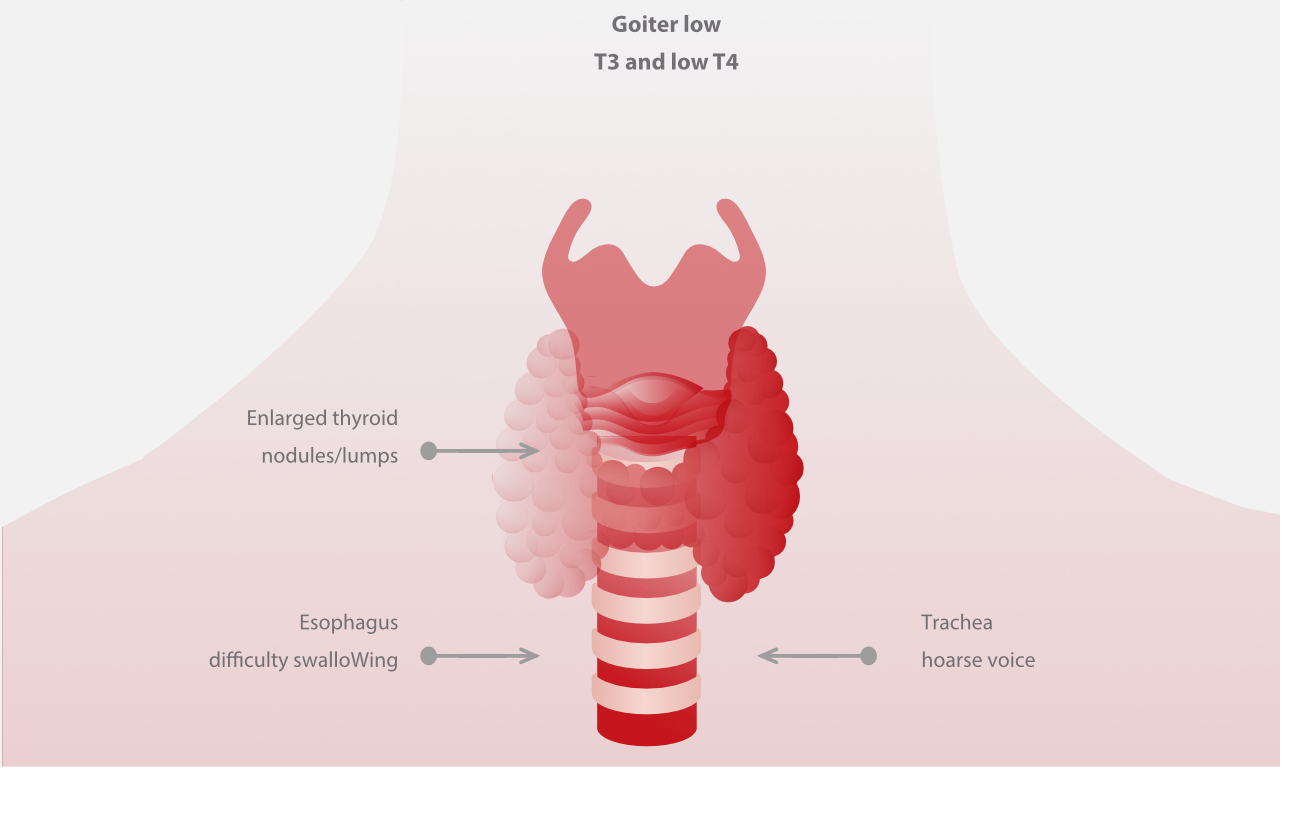
Symptoms of Hashimoto’s thyroiditis usually start in the hypothyroid phase and are directly related to the low T3 and T4 levels. Individuals often have a goiter, meaning that their thyroid is enlarged and sometimes has nodules, or lumps, which can sometimes press on the trachea, causing voice hoarseness, or on the esophagus, causing difficulty swallowing. The decreased metabolic rate could cause individuals to get tired easily, feel weak and cold, have constipation, and experience rapid weight gain even without any change in diet or exercise. Typically the heart rate and respiratory rate slow down as well.
Symptoms of Hashimoto’s Disease
The skin can become dry and rough due to decreased sweat secretion, and the hair and nails can become brittle and sometimes fall off. Ε levated prolactin levels from the increased thyrotropin-releasing hormone could also cause problems like menstrual abnormalities, galactorrhea, which is a milky nipple discharge, and infertility. In severe cases, myxedema develops, meaning that there is increased deposition of various proteins and mucopolysaccharides in the upper skin layers, leading to edema or swelling, in particular around the eyes, hands and feet.

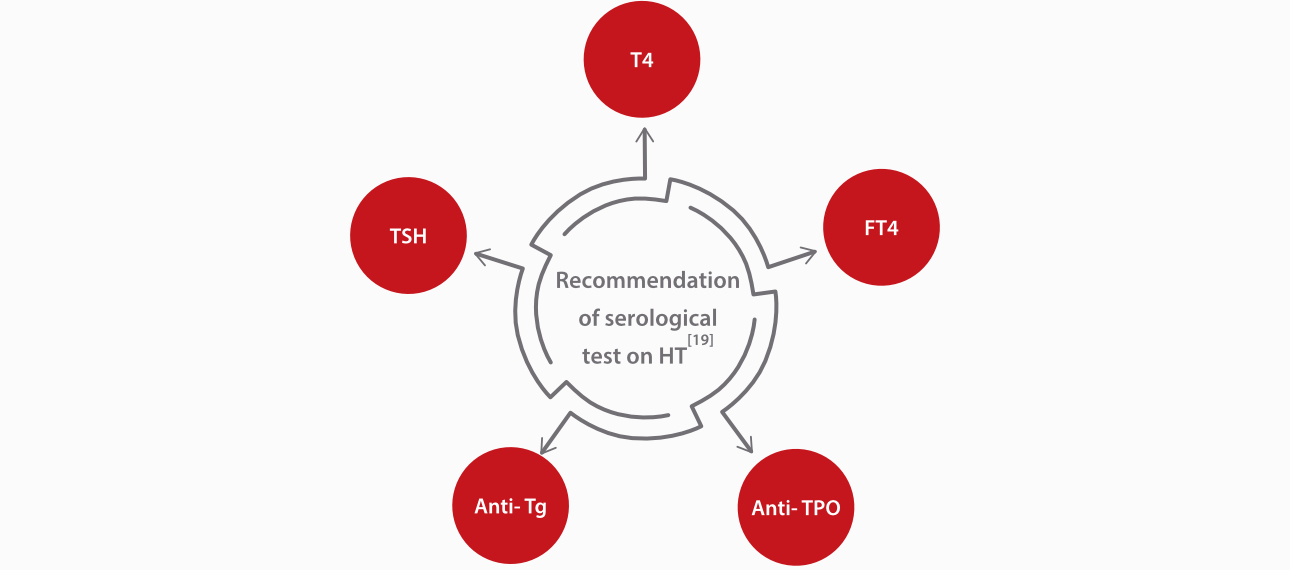
Diagnosis of Hashimoto’s Disease[15-17]
Diagnosis of Hashimoto’s thyroiditis is usually based on a combination of low serum levels of free thyroid hormones and increased TSH levels with high levels of the associated autoantibodies, mainly anti-thyroid peroxidase and antithyroglobulin antibodies. Fine- needle aspiration should be used to get a biopsy, when thyroid lymphoma is suspected.
Treatment of Hashimoto’s Disease[18]
Treatment of Hashimoto’s thyroiditis typically requires lifelong thyroid hormone replacement, mainly with levothyroxine. If there is a very large goiter compressing the airways or the esophagus, or if there is suspicion of a lymphoma, then surgical removal may be needed.

Mindray provides a comprehensive solution for thyroid-related disease diagnosis and management, especially for autoimmune thyroid disease, helping doctors to deliver reliable diagnosis and treatment options with accurate serum tests.
References
1. Lee NJ, Li CW, Hammerstad SS, Stefan M, Tomer Y. Immunogenetics of autoimmune thyroid diseases: a comprehensive review. J Autoimmun. 2015 November ; 64: 82–90.
2. Dong YH, Fu DG. Autoimmune thyroid disease: mechanism, genetics and current knowledge. Eur Rev Med Pharamcol Sci. 2014;18:3611-3618.
3. Kahaly GJ, Bartalena L, Hegedus L, Leenhardt L, Poppe K, Pearce SH. 2018 European Thyroid Association guideline for the management of Graves’ hyperthyroidism. European Thyroid Journal. 2018;7 (4):167–186. doi: 10.1159/000490384;
4. Ferrari SM, Fallahi P, Ruffilli I, et al. The association of other autoimmune diseases in patients with Graves’ disease (with or without ophthalmopathy): review of the literature and report of a large series. Autoimmunity Reviews. 2019;18(3):287–292. doi: 10.1016/j.autrev.2018.10.001
5. Rotondi M, Virili C, Pinto S, et al. The clinical phenotype of Graves’ disease occurring as an isolated condition or in association with other autoimmune diseases. Journal of Endocrinological Investigation. 2020;43(2):157–162. doi: 10.1007/s40618-019-01094-7
6. Mathew P, Rawla P. Hyperthyroidism. In: StatPearls [Internet]. StatPearls Publishing. Updated November 21, 2020. Accessed July 14, 2021.
7. Antonelli A, Fallahi P, Elia G, et al. Graves’ disease: clinical manifestations, immune pathogenesis (cytokines and chemokines), and therapy. Best Practice & Research Clinical Endocrinology & Metabolism.
2020;34(1):101388. doi: 10.1016/j.beem.2020.101388
8. The National Academy of Clinical Biochemistry (NACB): laboratory medicine practice guidelines: laboratory supporting for the diagnosis and monitoring of thyroid disease.
9. https://www.testing.com/graves-disease-testing/
10. https://www.thyroid.org/hashimotos-thyroiditis/
11. https://www.webmd.com/women/hashimotos- thyroiditis-symptoms-causes-treatments
12. Hashimoto‘s thyroiditis (lymphocytic thyroiditis). American Thyroid Association.
13. https://www.thyroid.org/hashimotos-thyroiditis/. Accessed Oct. 19, 2021.
14. Journal of Clinical Endocrinology & Metabolism. 2021; doi:10.1210/clinem/dgaa945.
15. Thyroid function tests. American Thyroid Association.
https://www.thyroid.org/thyroid-function-tests/. Accessed Sept. 28, 2021.
16. Thyroid hormone treatment. American Thyroid Association. http://www.thyroid.org/thyroid-hormone- treatment/ Accessed Oct. 19, 2021.
17. Goldman L, et al., eds. Thyroid. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Oct. 27, 2021.
18. https://www.wikihow.com/Treat-Hashimoto%27s- Disease#aiinfo
19. 2008 Guidelines for Diagnosis and Treatment of Thyroid Diseases in China-Hypothyroidism