What is Thyroid Cancer?
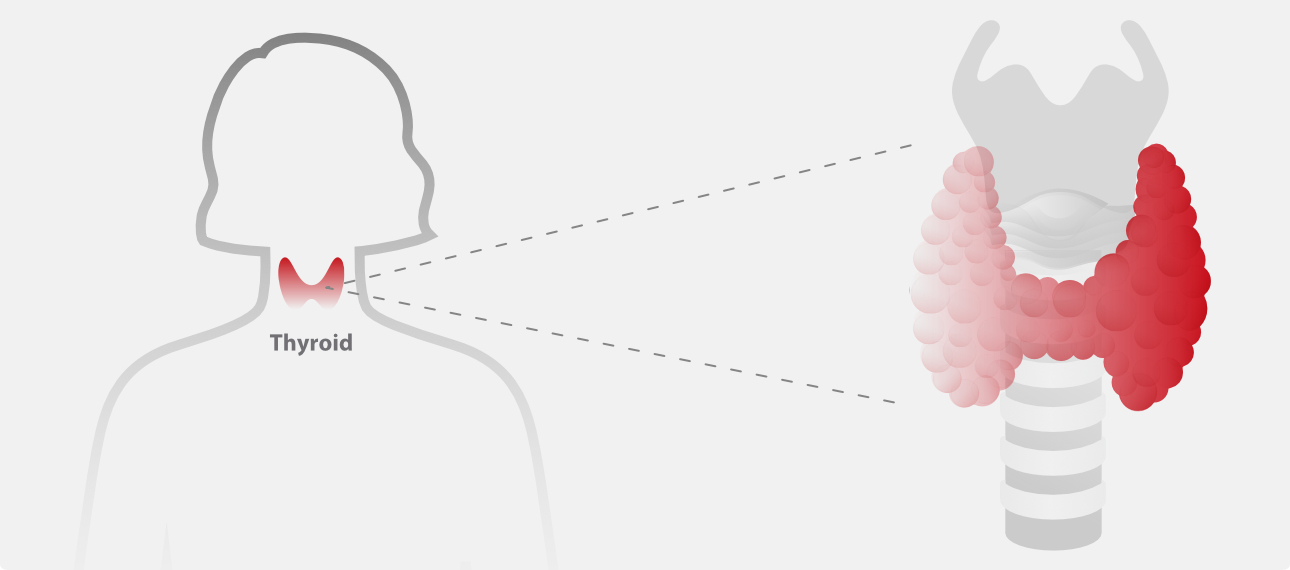
Thyroid cancer is a growth of cells that starts in the thyroid. The thyroid is a butterfly-shaped gland located at the base of the neck, just below the Adam's apple. The thyroid produces hormones that regulate heart rate, blood pressure, body temperature and weight.
Thyroid cancer might not cause any symptoms at first. But as it grows, it can cause signs and symptoms, such as swelling in your neck, voice changes and difficulty swallowing.
Several types of thyroid cancer exist. Most types grow slowly, though some types can be very aggressive. Most thyroid cancers can be cured with treatment.
Symptoms of Thyroid Cancer
In the early stages, thyroid cancer usually shows no signs or symptoms.
As a thyroid tumor grows, it may produce the following symptoms [1]:
- Neck mass or node: This is the most common symptom of thyroid cancer. A hard, fixed mass with an uneven surface is found in the thyroid gland. The glands are less mobile up and down during swallowing.
- Persistent hoarseness or changes in voice, and frequent coughs unrelated to a cold may occur.
- Difficulty swallowing or breathing. Swollen lymph nodes in the neck.
- Pain in ears, occiput, shoulders, and other parts. may occur in the late stage.

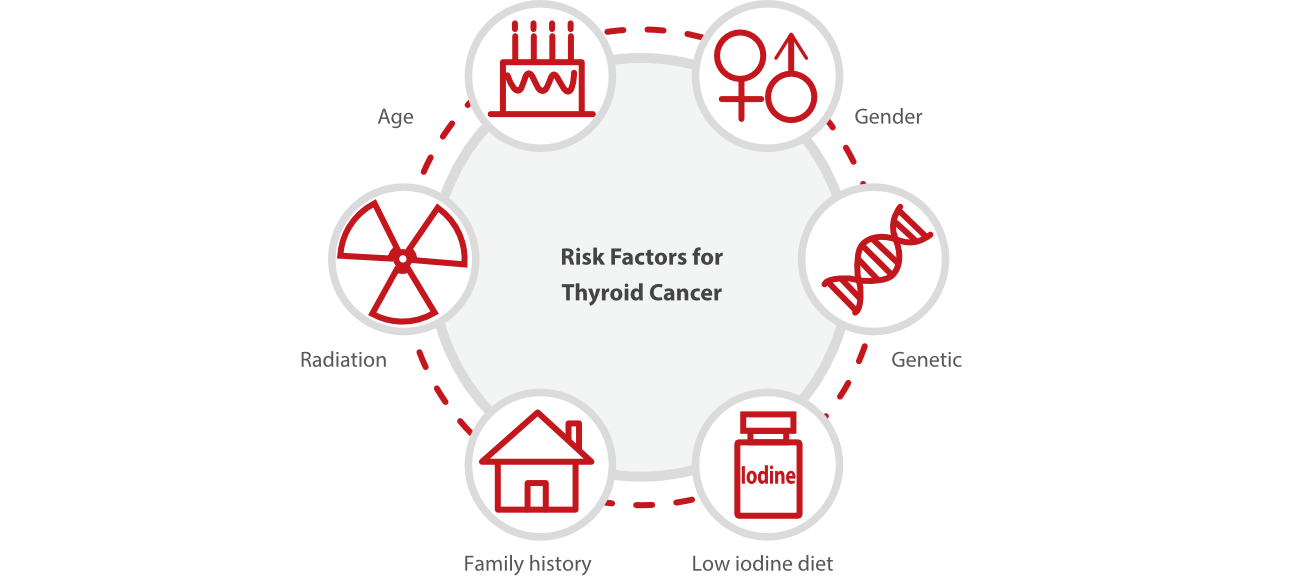
Risk Factors for Thyroid Cancer
Risk factors for thyroid cancer include ionizing radiation, family history, gender, obesity, alcohol consumption, and smoking. Recent studies have also demonstrated the relationship between exposure to flame retardants and PTC[2].
1. Gender and Race
Thyroid cancer is more common in women than men. White or Asian people are more likely to develop thyroid cancer.
2. Age
Most thyroid cancer patients are between 20 and 55 years old.
3. Radiation Exposure
Exposure to high levels of radiation may increase the risk of thyroid cancer.
4. Genetic Factors
Most thyroid cancer cases are sporadic, only 5% of DTC is characterized as familial (mainly PTC), and about 25% of MTC is inherited as an autosomal trait.
Certain genetic syndromes increase the risk of thyroid cancer. These include familial myeloid thyroid cancers and multiple endocrine neoplasms (type 2A and type 2B).
Mutations in certain genes are also important causes of thyroid cancer. Mutations in BRAF and RAS family also occur frequently in thyroid cancer. Chromosomal translocations also occur in thyroid cancer, such as peroxisome proliferation-activated receptor (PPAR gamma) translocations in about 30% of follicular thyroid cancer cases[3-4].
Diagnosis of Thyroid Cancer [5]
Comprehensive and thorough diagnosis of thyroid cancer involves a number of procedures and tests that your healthcare provider may use to diagnose thyroid cancer and rule out other thyroid conditions. Usually, the process of evaluating for thyroid cancer starts with finding a lump or nodule in your gland.
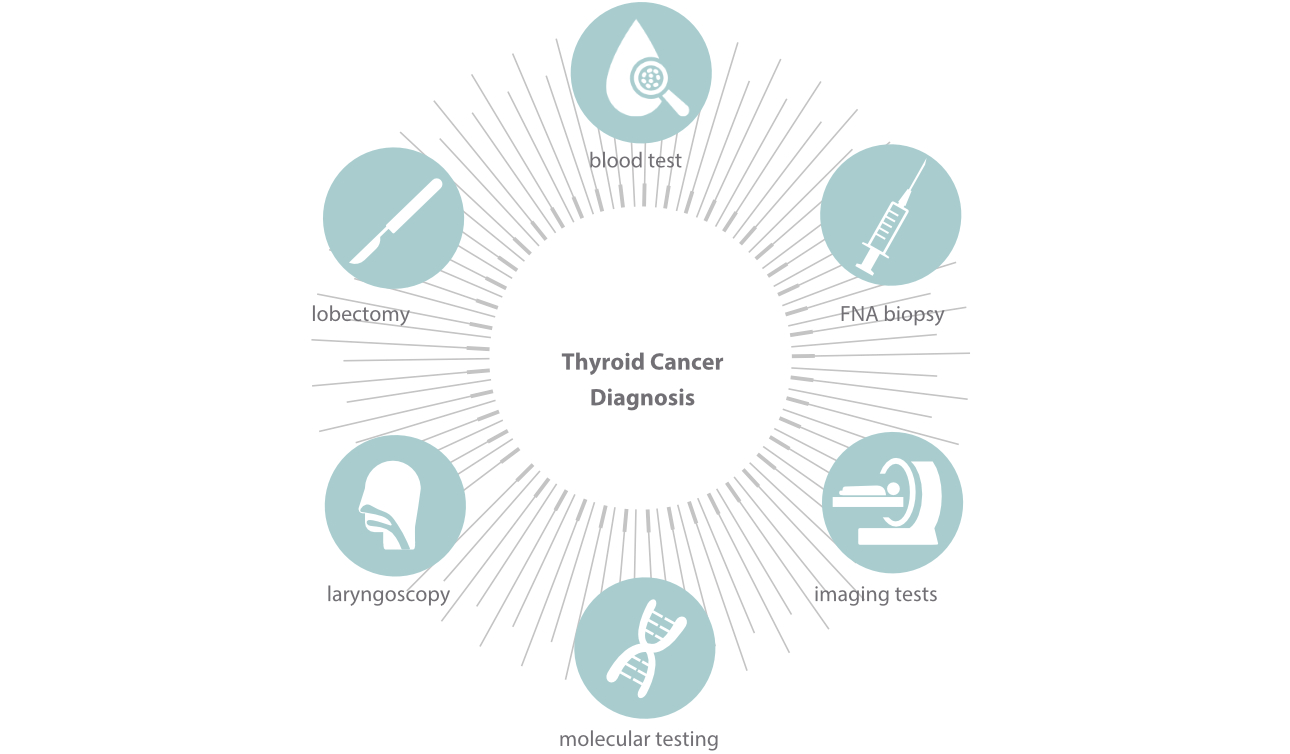
Some of the main methods for diagnosing thyroid cancer are:
Blood tests: Blood tests cannot diagnose thyroid cancer itself or detect a cancerous thyroid nodule, but they can rule out other conditions and determine if your thyroid is working the way it should. Blood tests your healthcare provider may use include thyroid stimulating hormone (TSH), T3, T4, calcium and thyroglobulin.
1. TSH: Your healthcare provider may check the TSH level in your blood to evaluate your thyroid's activity and test for hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid). The result of this test can help your healthcare provider determine which imaging tests to do to visualize your nodule. That said, with thyroid cancer, your TSH level is typically normal.
2. T3 and T4: These are the main hormones that your thyroid makes. Your healthcare provider may test your levels to check how your thyroid is functioning. Like TSH, these hormone levels are usually normal when you have thyroid cancer.
3. Calcium: When medullary thyroid cancer is suspected, your healthcare provider will typically test for high levels of calcium, as this can be an indicator of the disease.
4. Thyroglobulin: The thyroid makes a protein called thyroglobulin that is then converted into T3 and T4. If you have already been treated for thyroid cancer and you have had a thyroidectomy, your healthcare provider may check to make sure your cancer is gone or to see if it has come back by looking at your thyroglobulin level. Though this test cannot diagnose cancer, it can be a marker for it. Since you no longer have a thyroid to make thyroglobulin, if there is more than a very low level in your blood, or if it rises after having been low, this may indicate cancer. In this case, your healthcare provider will likely do some other tests to verify and treat you accordingly.

Treatment of Thyroid Cancer [6-8]
1. Surgical Treatment
Surgery is the basic method for treating various types of thyroid cancer except for ATC. Other auxiliary treatment methods such as nuclide, thyroid hormone and external radiation are usually used.
Surgical treatment of thyroid cancer includes partial thyroidectomy or lobectomy and total thyroidectomy.
2. Endocrine Therapy
TSH can stimulate the proliferation of thyroid cancer cells through its receptor. Therefore, thyroid hormone therapy such as TSH inhibitors is used after surgery. This method can significantly reduce recurrence and cancer-related mortality in patients with different types of thyroid cancer. Meanwhile, patients should take enough thyroxine supplements.
3. Radionuclide Therapy
Some patients with papillary or follicular carcinoma may require systemic radioactive iodine (RAI) after thyroidectomy. When radioactive iodine enters the bloodstream, it selectively destroys the remaining thyroid tissue and cancer cells without affecting any other cells. The adjuvant therapy is applicable to patients over 45 years old, multiple cancerous foci, locally invasive tumors, and distant metastases.
4. Chemotherapy
Chemotherapy is rarely used to treat thyroid cancer, except for malignant tumors such as undifferentiated thyroid cancer.
5. External Radiation Therapy
This method is mainly used to treat ATC.
Mindray provides reliable thyroid kits for thyroid cancer diagnosis and management. These tests can be performed on Mindray's wide range of robust CLIA analyzers tailored to different laboratories, making reliable diagnostics accessible to all.

References
1. Hoffman K, Lorenzo A, Butt C M, et al. Exposure to flame retardant chemicals and occurrence and severity of papillary thyroid cancer: A case-control study [J]. Environment International, 2017, 107: 235-242.
2. Lodish M B, Stratakis C A. RET oncogene in MEN2, MEN2B, MTC and other forms of thyroid cancer [J]. Expert Review of Anticancer Therapy, 2008, 8(4): 625-632
3. None. Integrated Genomic Characterization of Papillary Thyroid Carcinoma [J]. Cell, 2014, 159(3): 676-690.
4. Raman P, Koenig R J. Pax-8–PPAR-γ fusion protein in thyroid carcinoma [J]. Nature Reviews Endocrinology, 2014, 10(10): 616-623.
5. American Cancer Society. Tests for Thyroid Cancer.
6. Biondi B, Filetti S, Schlumberger M. Thyroid-hormone therapy and thyroid cancer: a reassessment [J]. Nature Clinical Practice Endocrinology & Metabolism, 2005, 1(1): 32-40.
7. Mazzaferri E L. Current Approaches to Primary Therapy for Papillary and Follicular Thyroid Cancer [J]. Journal of Clinical Endocrinology & Metabolism, 2001, 86(4):
1447-1463
8. Spitzweg C, Bible K C, Hofbauer L C, et al. Advanced radioiodine-refractory differentiated thyroid cancer: the sodium iodide symporter and other emerging therapeutic targets [J]. The Lancet Diabetes & Endocrinology, 2014, 2(10): 830-842.