What is Euthyroid Sick Syndrome (ESS)?
Euthyroid sick syndrome (ESS) is also known as nonthyroidal illness syndrome and refers to changes in thyroid function tests that are administered in the inpatient or intensive care setting during critical illness. It is not a true syndrome, and transient alterations in the hypothalamic-pituitary-thyroid axis are present in about 75% of hospitalized patients. This condition is often seen in patients with severe critical illness, deprivation of calories, and after major surgeries. The causes of ESS vary, including critical illness, pneumonia, starvation, anorexia nervosa, sepsis, stress, history of trauma, cardiopulmonary bypass, myocardial infarction, malignancies, congestive cardiac failure, hypothermia, inflammatory bowel disease, cirrhosis, major surgeries, renal failure, and diabetic ketoacidosis.

Symptoms of Euthyroid Sick Syndrome
ESS very often mimics hypothyroidism. It is a condition in which the patient generally exhibits signs and symptoms of hypothyroidism such as:
Prevalence of Euthyroid Sick Syndrome[1]

Who is at high risk of ESS?
ESS is seen in 40% of patients presenting with any major illness. Other conditions that may put the patients at an increased risk of ESS include:

Changes in thyroid tests during the course of Euthyroid Sick Syndrome[2]

An overview of reverse T3
Thyroid Releasing Hormone is made by the hypothalamus and it stimulates the pituitary gland in the brain to make TSH (Thyroid Stimulating Hormone). TSH stimulates the thyroid gland to produce Free T4 as the final product. Free T4 undergoes two forms of conversion: into an ACTIVE Free T3 or INACTIVE ReverseT3 (rT3)[3].

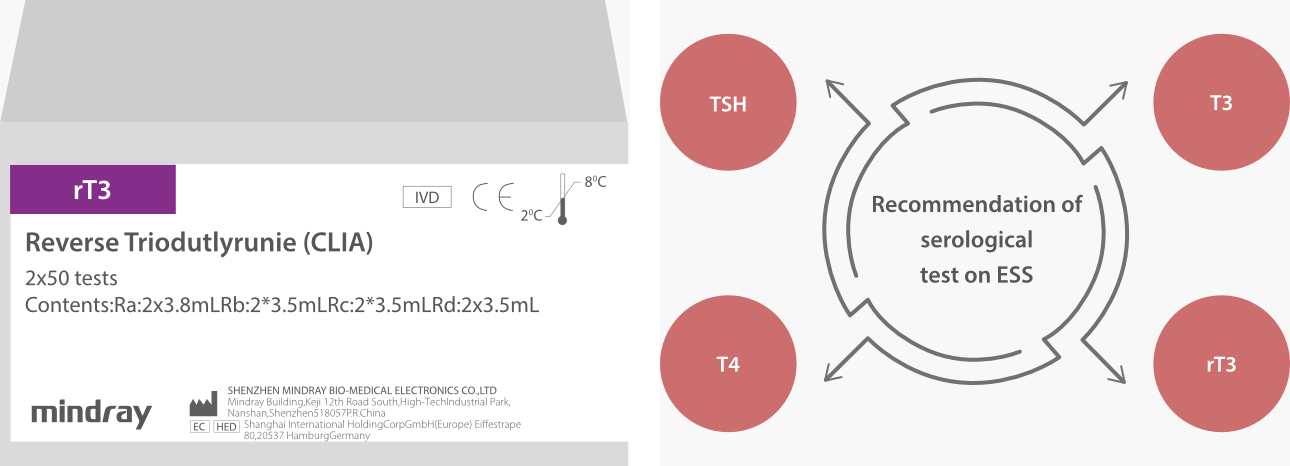
Clinical applications of rT3 assay
Clinical application 1: Differential diagnosis of ESS and hypothyroidism
rT3 plays a very important role in the differential diagnosis of ESS and hypothyroidism!

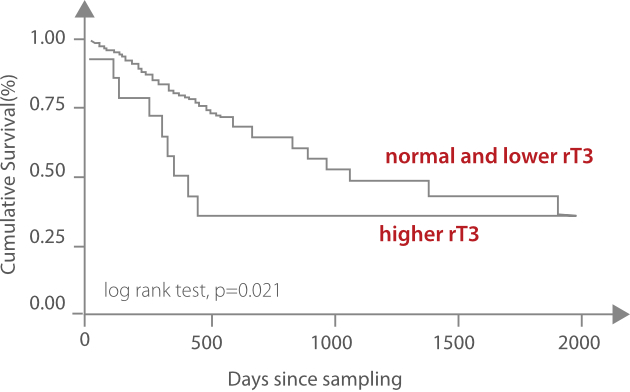
Clinical application 2: Prediction of prognosis of ESS[4-5]

Critically ill patients with ESS have a poor state of health. Higher rT3 values are associated with severe illness.
Mindray provides reliable rT3 assay to support differential diagnosis and management of ESS.
References
1. Adler, S. M. , and L. Wartofsky . "The nonthyroidal illness syndrome. " Endocrinology & Metabolism Clinics of North America 36.3(2007):657-672.
2. Radovick, S. , and M. H. Macgillivray . "Pediatric Endocrinology || Non-thyroidal Illness Syndrome." 10.1007/978-1-60761-395-4.Chapter 17(2013):289-302.
3. https://sproutshealth.com/the-role-of-reverse-t3-in- thyroid-function-part-1/
4. Friberg, L. , et al. "Association between increased levels of reverse triiodothyronine and mortality after acute myocardial infarction. " American Journal of Medicine 111.9(2001):699-703.
5. Horacek, J. , et al. "Thyroid hormone abnormalities in hemodialyzed patients: low triiodothyronine as well as high reverse triiodothyronine are associated with increased mortality. " Physiological Research 61.5 (2012):495-501.