Special Thanks to the Urology Subprofessional Group, Department of Ultrasound medicine, The 10th People's Hospital affiliated to Tongji University.
Key Points
- Prostate cancers can appear isoechoic and be missed on standard grayscale TRUS imaging.
- MRI is highly sensitive for prostate cancer diagnosis, but MRI guided biopsies are complicated and expensive.
- Targeted prostate biopsy using TRUS/MRI iFusion guidance can improve diagnostic accuracy for prostate cancer.
Case Description
A 72 year-old man with a history of increased prostate specific antigen (PSA 7.9 ng/ml) was sent to the department of ultrasound at the 10th People’s Hospital affiliated to Tongji University for treatment. A transrectal ultrasound prostate examination (TRUS) and multiparameter MRI were performed with results as follows:
Multi-parameter MRI findings:
- Suspected lesion in the right anterior lobe of the prostate (PI-RADS classification 4).
- Prostatic hyperplasia with calcifications and small prostatic cysts.
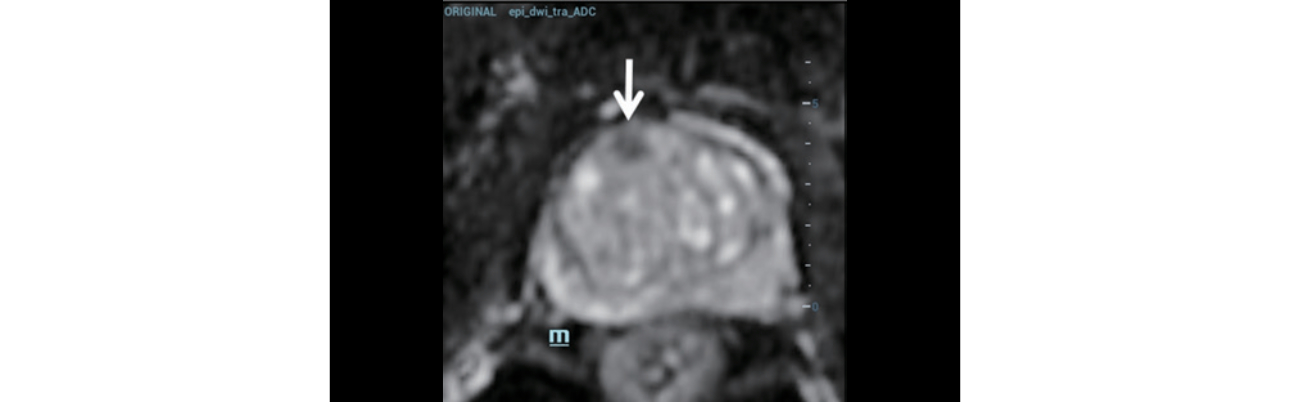
TRUS finding (figure 1):
- Prostatic hyperplasia with calcifications and small prostatic cysts.
- Heterogeneous prostatic echotexture with no discrete lesion identified.
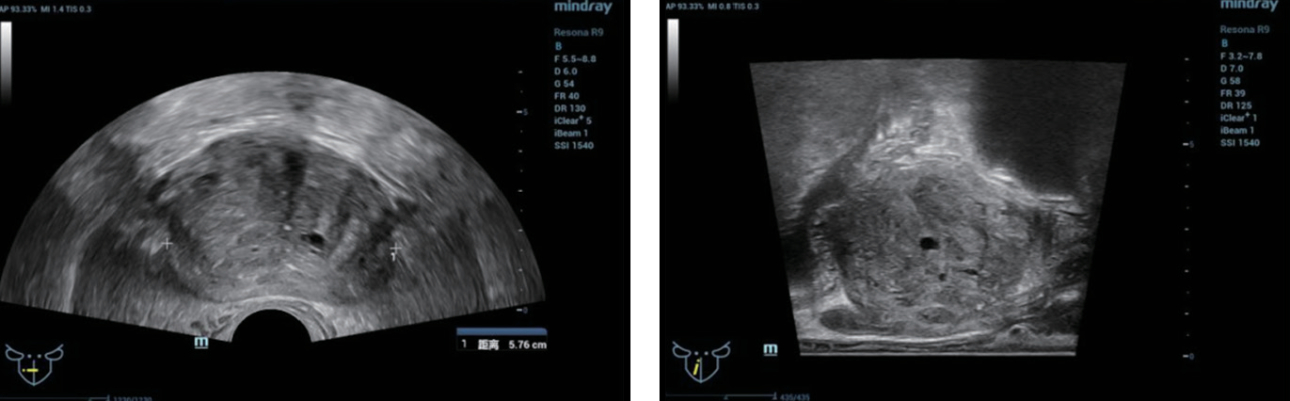
Preoperative discussion: As the suspicious lesion could not be identified on conventional ultrasound, the patient was scheduled for a targeted perineal prostate 12-point systemic needle biopsy under TRUS/MRI fusion guidance.
TRUS/MRI Fusion guided biopsy protocol:
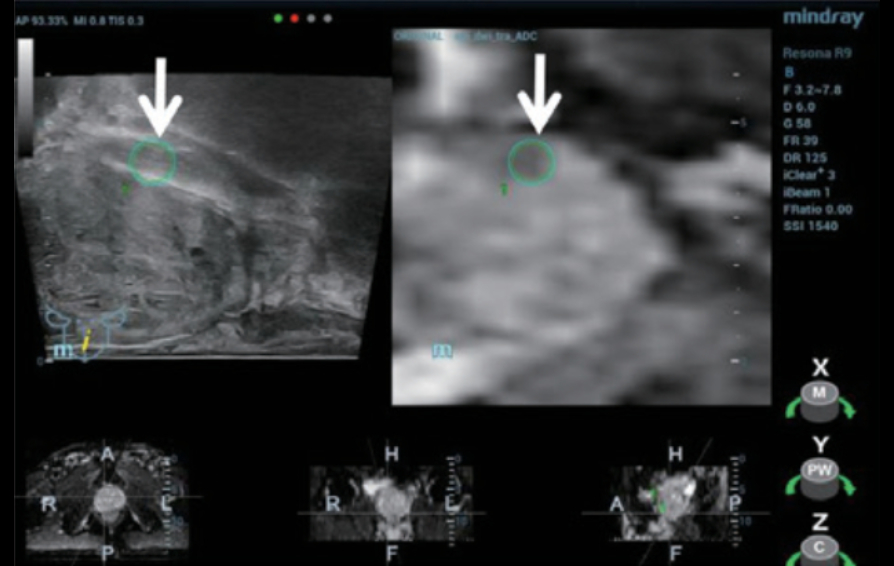
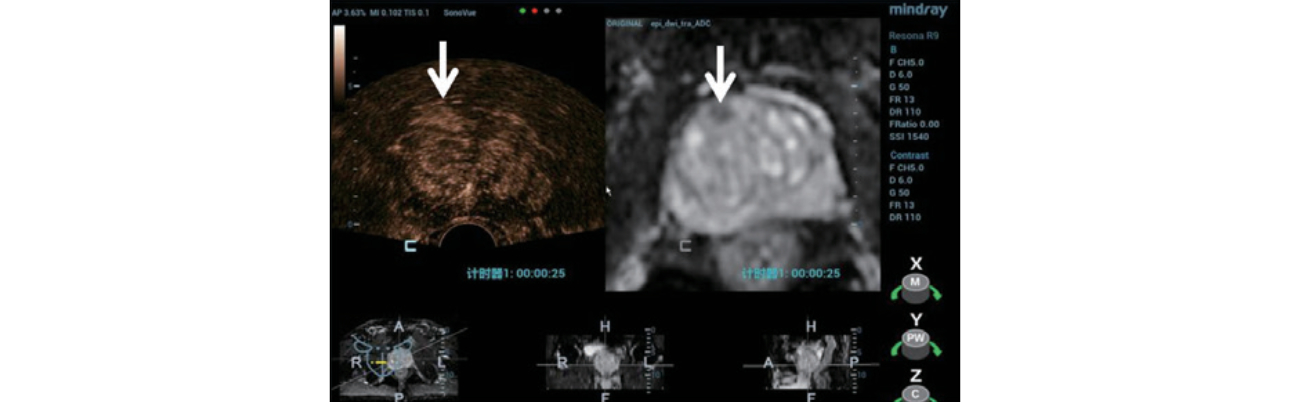
Step 1: The appropriate MRI sequence (Figure 2) was selected and the dataset imported onto the Resona 9 and into the live ultrasound exam.
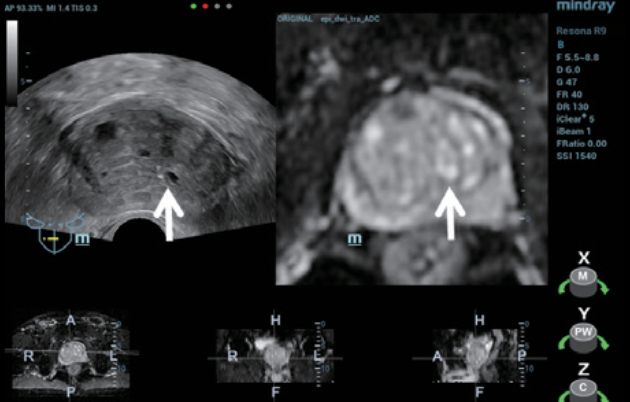
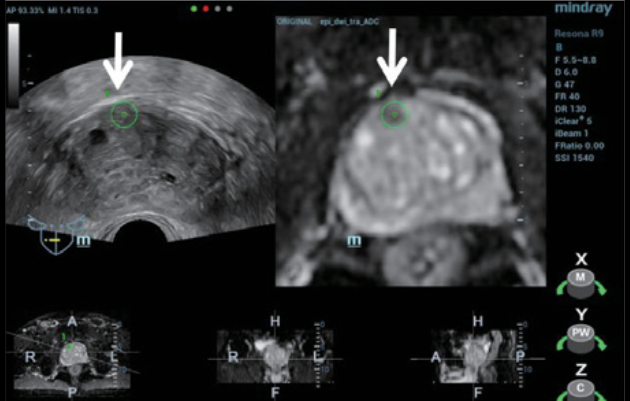
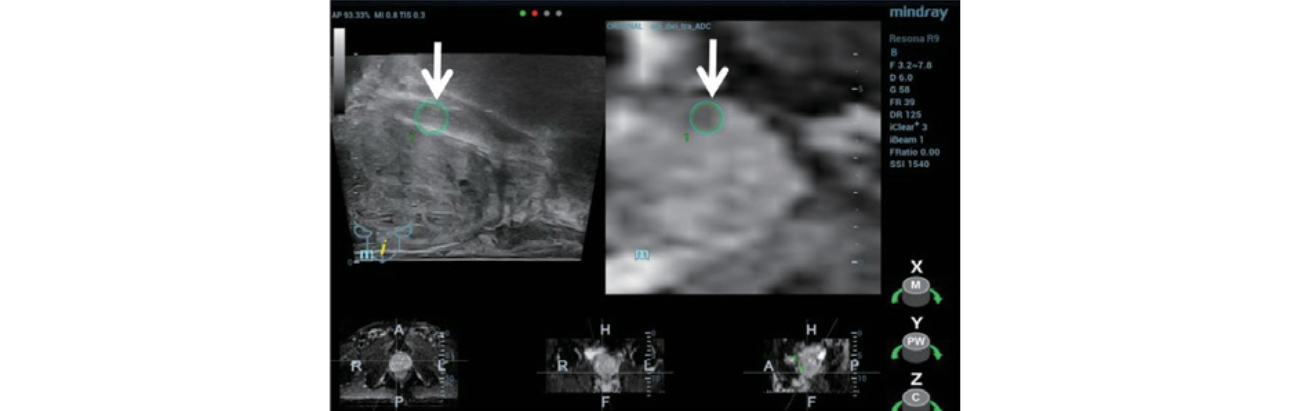
Step 2: Using Mindray’s iFusion software, the TRUS and MRI images were aligned and fused (Figure 3) and the target was labeled (Figure 4).
Step 3: To verify the lesion location, a contrast enhanced ultrasound (CEUS) was performed using the MRI image for anatomical reference (Figure 5).
Step 4: Under TRUS/MRI fusion guidance, a 12 core systemic biopsy was performed, followed by a targeted biopsy including 3 samples from the suspected lesion. (Figure 6) No complications were seen post procedure.
Pathology result: All 12 systemic punctures demonstrated benign prostatic hyperplasia. One of the three targeted punctures revealed prostatic adenocarcinoma.
Discussion and reflection
TRUS-guided biopsy combined with PSA is an important method for the diagnosis of prostate cancer (PCa). Peripheral zone hypoechoic nodules are a typical sign of PCa, however, in early PCa these lesions appear isoechoic in many cases which makes differentiation from prostatic hyperplasia and low-grade prostatic intraepithelial neoplasia difficult and can result in missed diagnosis [1]. In this case, PSA was increased, but no suspicious lesions were detected on TRUS imaging.
Systemic biopsy is the current main diagnostic method for PCa. As the biopsy sites are standardized rather than targeted at a particular suspicious lesion, this method may also result in missed diagnosis or underestimation of disease. Multi parameter MRI has a high sensitivity and specificity for the diagnosis of PCa, however, MRI guided biopsy is complicated and expensive. Mindray iFusion software on the Resona 9 provides a solution by fusing the MRI dataset with live ultrasound imaging. Using bi-plane TRUS/MRI fusion guidance for targeted prostate biopsy improves the accuracy of clinical prostate cancer diagnosis [2].
In this case, the suspicious lesion was detected on MRI and using iFusion navigation the corresponding plane and target area were labeled on ultrasound. A CEUS exam provided additional diagnostic information and three guided biopsies were performed into the suspect area. While the standard 12-point samples were negative, one of the targeted samples came back positive for PCa. This case clearly shows how biplane TRUS/MRI fusion targeted biopsy can help avoid missed diagnosis and improve diagnostic accuracy.
References:
1. HUANG Haiming, XU Haiyan, CHEN Yane, ZHANG Zhongxin. Application value of guided prostate puncture under ultrasonic magnetic resonance. JOURNAL OF MINIMALLY INVASIVE UROLOGY, 2021, 10(1): 50-54.
2.Moore CM, Robertson NL, Arsanious N, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013. 63(1): 125-140.