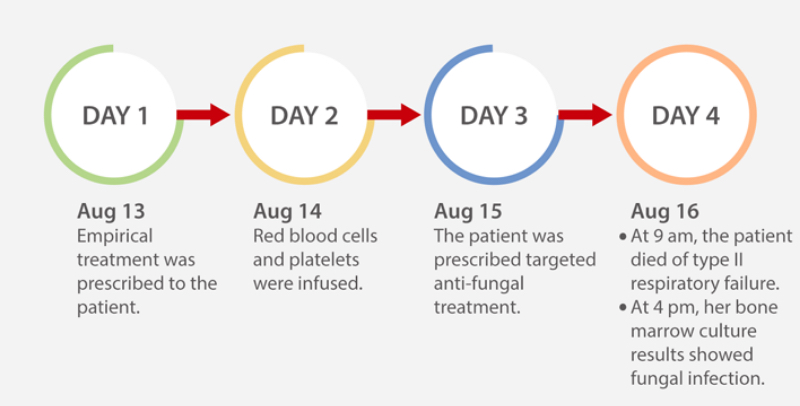
A 43-year-old woman presented with persistent fever for two months. She had visited different hospitals more than three times, but there was no significant improvement in her symptoms. After being admitted to a top-tier hospital in China, she underwent a series of examinations. Her serology test was positive for human immunodeficiency virus (HIV) infection. Her chest computed tomography (CT) scan showed diffuse small nodules in both lungs. Disseminated Talaromyces marneffei infection was considered, based on the patient’s symptom of fever, laboratory test and CT scan results. She was prescribed targeted anti-fungal treatment.
Unfortunately, she died four days after admission to the hospital as the infection worsened and her condition rapidly deteriorated. Seven hours after she died, hyphae-like structures were spotted on the gram stain of the positive bone marrow culture.
What is Talaromyces marneffei?
Talaromyces marneffei is a fungus that causes opportunistic systemic mycoses in patients with AIDS or other immunodeficiency syndromes. The fungus was first isolated from the hepatic lesions of a bamboo rats (Rhizomys sinensis) in 1956 (Figure 2). It has been suggested that these animals serve as a reservoir for the fungus. It is not clear whether the rats are infected by Talaromyces marneffei or are merely carriers of the fungus.

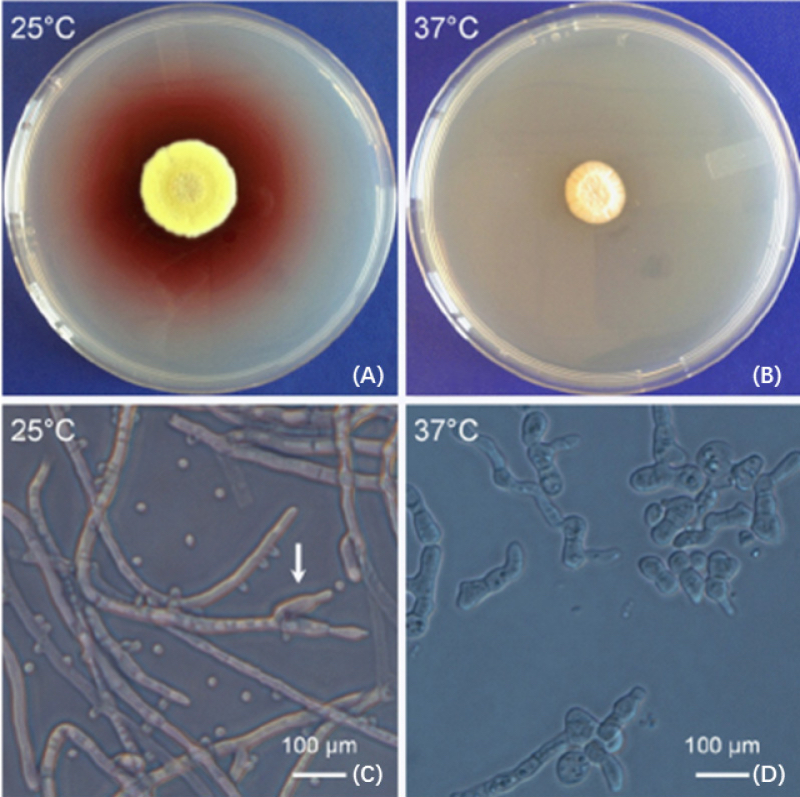
Talaromyces marneffei is usually diagnosed by microscopic identification of the fungus in various clinical specimens and by standard microbiological culture, based on its morphological characteristics and thermally dimorphic properties between 25°C (mycelium form) and 37°C (yeast form) (Figure 3).
Epidemiology
Talaromyces marneffei is endemic in Myanmar, Cambodia, Southern China, Indonesia, Laos, Malaysia, Thailand and Vietnam. Patients spread the AIDS and Talaromycosis all over the world through travel (Figure 4).

Clinical presentation
Talaromycosis is a potentially fatal infection causing rapid deterioration [4]. The main manifestations of Talaromyces marneffei infection are fever, cough, lymphadenectasis, hepatosplenomegaly, skin lesion, dyspnea, and weight loss, but they are nonspecific and have no significance for differential diagnosis.[5]
Since its clinical manifestations lack specificity, it is easy to be dismissed as a diagnosis or misdiagnosed, leading to high mortality and poor prognosis.
Laboratory diagnosis
Microbiological culture is a ‘gold standard’ diagnostic method. However, it lacks sensitivity and is time-consuming, which affects clinical decisions and delays the initiation of appropriate treatment. Although metagenomic next-generation sequencing (mNGS), polymerase chain reaction (PCR) and Tzanck cytology smear tests can detect Talaromyces marneffei, they are relatively expensive and they require sophisticated instruments and skilled laboratory personnel.[6-8]
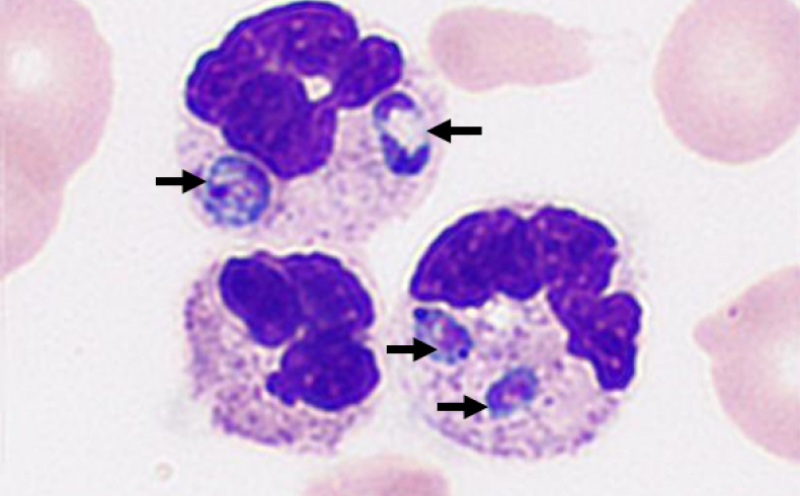
In the previous clinical case, using peripheral blood smears, Mindray’s brand new Automatic Digital Cell Morphology Analyzer detected Talaromyces marneffei yeast cells (black arrow) that had been phagocytized by neutrophils (Figure 5). The yeast cells were round to oval and measured 2-5μm in diameter. Occasional clear cross wall septa were seen.
In adults, Talaromyces marneffei infects patients with AIDS. Nevertheless, recent studies showed most pediatric patients were HIV negative, yet still had severe systemic complications and poor prognosis.
Therefore, simpler and faster tests with higher sensitivity and specificity are required. A digital morphology system can help to establish a rapid clinical diagnosis of talaromycosis before results from cultures are reported. In particular, Mindray’s brand-new digital morphology system can provide a convenient and high-performance method to aid diagnosis of Talaromyces marneffei infection. Please stay tuned for more details on this new system.
References:
[1] Huang, X., He, G., Lu, S., Liang, Y. & Xi, L. Role of Rhizomys pruinosus as a natural animal host of Penicillium marneffei in Guangdong, China. Microb Biotechnol 8, 659-664, doi:10.1111/1751-7915.12275 (2015).
[2] Yang, E.; Wang, G.; Woo, P. C.; Lau, S. K.; Chow, W. N.; Chong, K. T.; Tse, H.; Kao, R. Y.; Chan, C. M.; Che, X.; Yuen, K. Y.; Cai, J. J., Unraveling the molecular basis of temperature-dependent genetic regulation in Penicillium marneffei. Eukaryot Cell 2013, 12 (9), 1214-24.
[3] Fungal infections. Talaromyces marneffei infection. Cheshire (UK): Leading International Fungal Infection (LIFE). Available: www.life-worldwide.org/fungal-diseases/talaromyces-marneffei-infection (accessed 2019 Nov. 21).
[4] Wu T, Chan JW, Ng C, Tsang DN, Lee M, Li PC. Clinical presentations and outcomes of Penicillium marneffei infections: A series from 1994 to 2004. Hong Kong Med J 2008;14:103.
[5] Zeng, Q. et al. Peripheral immune profile of children with Talaromyces marneffei infections: a retrospective analysis of 21 cases. BMC Infect Dis 21, 287, doi:10.1186/s12879-021-05978-z (2021).
[6] Shi, J., Yang, N. & Qian, G. Case Report: Metagenomic Next-Generation Sequencing in Diagnosis of Talaromycosis of an Immunocompetent Patient. Front Med (Lausanne) 8, 656194, doi:10.3389/fmed.2021.656194 (2021).
[7] Zhou, Y., Liu, Y. & Wen, Y. Gastrointestinal manifestations of Talaromyces marneffei infection in an HIV-infected patient rapidly verified by metagenomic next-generation sequencing: a case report. BMC Infect Dis 21, 376, doi:10.1186/s12879-021-06063-1 (2021).
[8] Lai, S. K., Rauf, N. A., Preet, K. R. & Tan, L. J. Tzanck cytology smear in diagnosis of cutaneous talaromycosis (penicilliosis). Indian J Dermatol Venereol Leprol, 1-4, doi:10.25259/IJDVL_268_20 (2021).