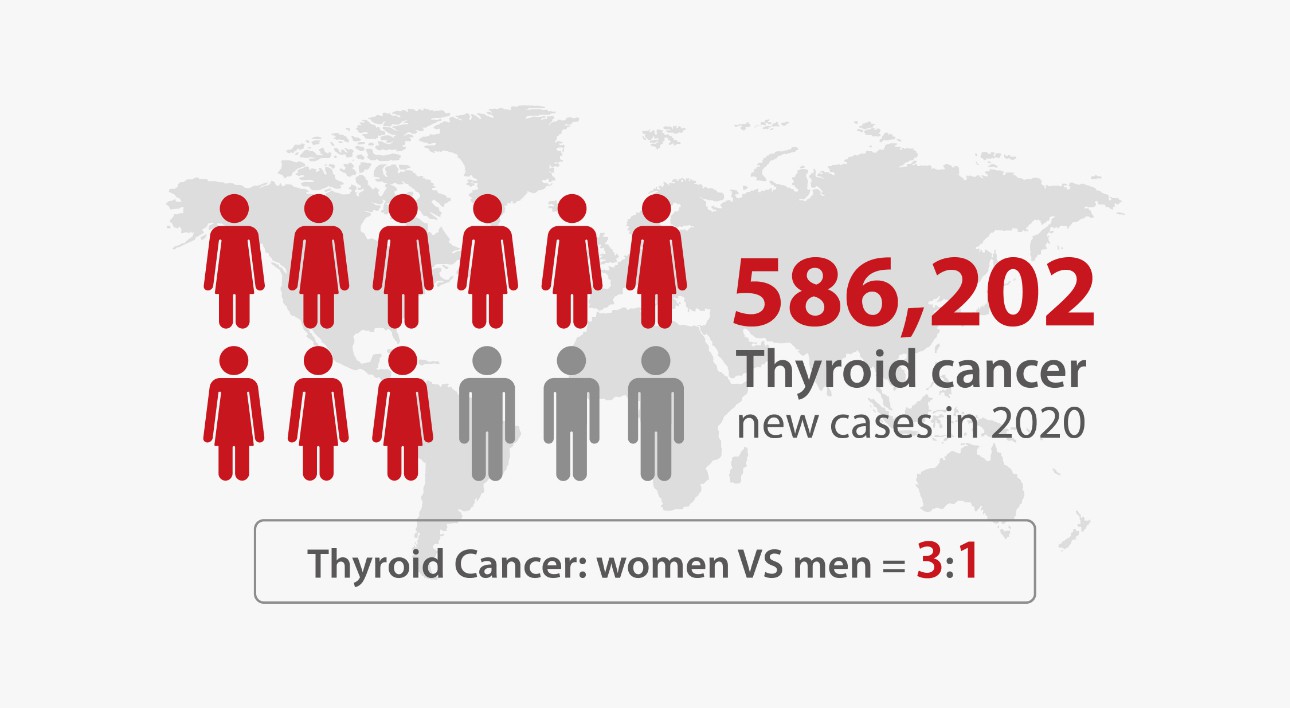
Thyroid cancer has become an increasingly serious threat to public health. It is the seventh most common cancer in women. Worldwide, an estimated 586,202 people were diagnosed with thyroid cancer in 2020.[1]
The growing number of new thyroid cancer cases was largely due to increased detection in the early stage, which would actually benefit the treatment and prognosis of the patients.[2] Hence, proper diagnosis and monitoring technologies would be of great importance for all patients.
Thyroid cancer is a disease in which malignant (cancer) cells form in the thyroid gland. The thyroid gland is located at the base of your neck and produces hormones that regulate your metabolism. Thyroid cancer can be either benign or malignant, but it's more common for tumors to be malignant.[3] There are four main types of thyroid cancer: papillary, follicular, medullary, and anaplastic
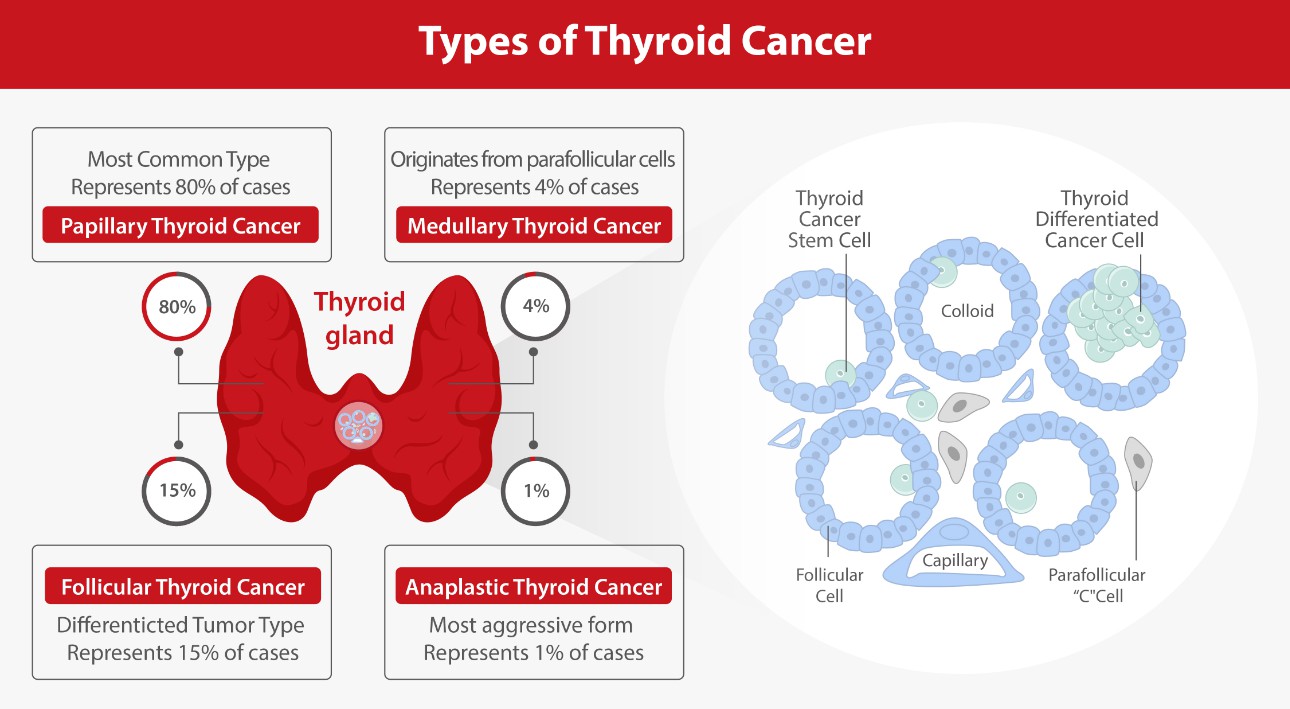
Papillary carcinoma accounts for about 80% of all thyroid cancer cases, making it the most common type overall. It tends to grow slowly and rarely spreads outside the thyroid gland unless left untreated for a long time or if it's very large when diagnosed (highly differentiated). Follicular carcinoma makes up about 15% of all thyroid cancer cases. It grows quickly but not as aggressively as other types do (moderately differentiated). It tends to spread into nearby lymph nodes before spreading elsewhere in the body via blood vessels. The follicular and papillary types can be classified as differentiated thyroid cancer,[4] which carry a more favorable prognosis than the other types.
Normally, the confirmation of thyroid cancer is required when a thyroid nodule is found in a physical examination. An ultrasound of the thyroid and a biopsy examination are often used. Blood tests that measure thyroid hormones and antithyroid antibodies may also be helpful for identifying other types of thyroid disease. For example, the measurements of thyroid stimulating hormone (TSH), free and/or total triiodothyronine (T3) and thyroxine (T4) levels, and antithyroid antibodies help to decide if a functional thyroid disease such as Hashimoto's thyroiditis is present, a known cause of a benign nodular goiter.[5]

Besides, there are several serum biomarkers that have been identified as useful for thyroid cancer detection and monitoring, including thyroglobulin (Tg) and calcitonin (CT). Tg is a protein produced by the thyroid gland that is used as a marker for thyroid cancer. Tg levels are typically elevated in patients with thyroid cancer, and monitoring Tg levels can help to detect the recurrence of the disease after treatment. Tg levels can also be used to monitor the effectiveness of treatment, as a decrease in Tg levels typically indicates a positive response to treatment.[6]
Moreover, measurements of CT levels are necessary to exclude the presence of medullary thyroid cancer. CT is a hormone that is produced by the thyroid gland and is used as a marker for medullary thyroid carcinoma (MTC),[7] a rare form of thyroid cancer. Elevated levels of CT can indicate the presence of MTC, and monitoring CT levels can help to detect the disease early on.
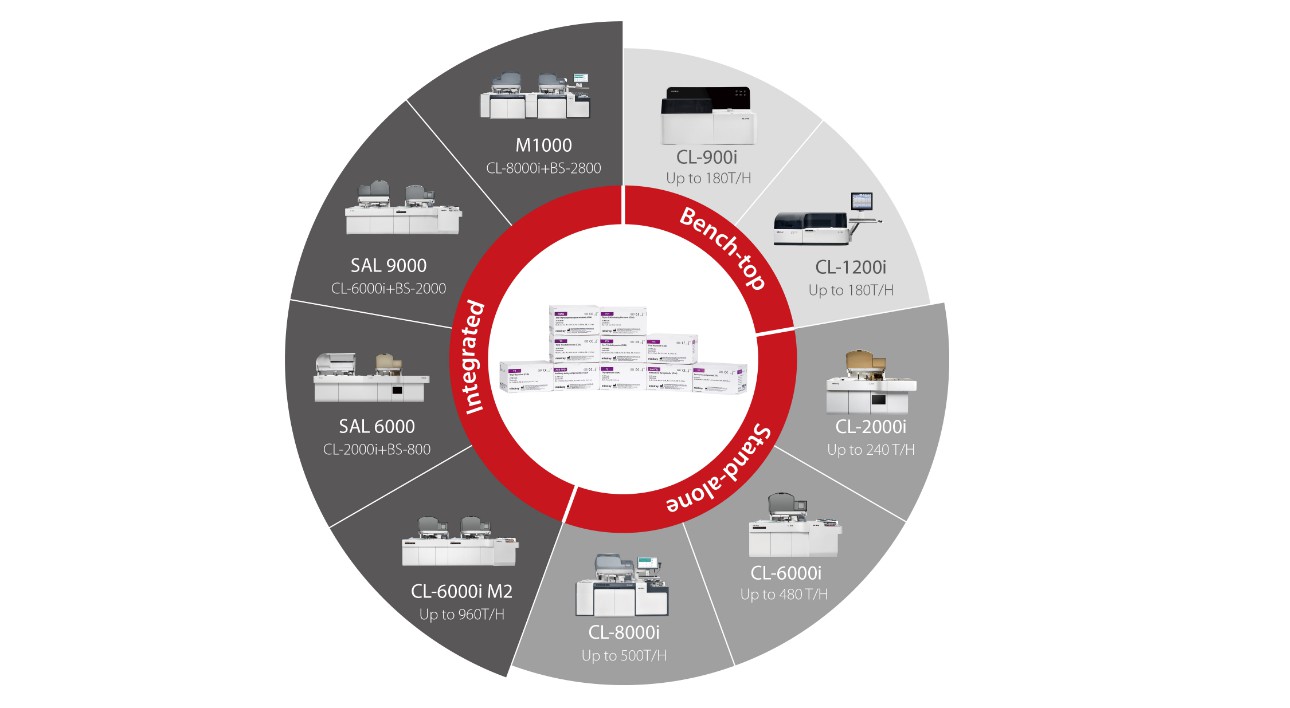
As a leading in-vitro diagnostics solutions provider globally, Mindray offers a complete chemiluminescence immunoassay portfolio of thyroid total solutions. With excellent performance and high quality, all these thyroid assays can be applied to all Mindray chemiluminescence platforms. Mindray’s Thyroid Total solutions are expected to serve as reliable and stable enablers for clinical diagnosis.
References:
[1] https://www.thyca.org/
[2] Nguyen, Quang T et al. “Diagnosis and treatment of patients with thyroid cancer.” American health & drug benefits vol. 8,1 (2015): 30-40.
[3] https://www.cancer.gov/types/thyroid/hp/thyroid- treatment-pdq
[4] Nix, P et al. “Thyroid cancer review 2: management of differentiated thyroid cancers.” International journal of clinical practice vol. 59,12 (2005): 1459-63. doi:10.1111/j.1368-5031.2005.00672.x
[5] Bennedbaek, F N et al. “Diagnosis and treatment of the solitary thyroid nodule. Results of a European survey.” Clinical endocrinology vol. 50,3 (1999): 357-63. doi:10.1046/j.1365-2265.1999.00663.x
[6] Spencer, C. A., & Lopresti, J. S. (2008). Measuring thyroglobulin and thyroglobulin autoantibody in patients with differentiated thyroid cancer. Nature clinical practice. Endocrinology & metabolism, 4(4), 223–233. https://doi.org/10.1038/ncpendmet0757
[7] Verbeek, Hans Hg et al. “Calcitonin testing for detection of medullary thyroid cancer in people with thyroid nodules.”The Cochrane database of systematic reviews vol. 3,3 CD010159. 16 Mar. 2020, doi:10.1002/14651858.CD010159.pub2







