Ultrasound Journal 21 - Ultrasound Evaluation of Stress Urine Continence in Patients Who Not Require Immediate Surgical Treatment
2024-01-09
Special thanks to Dr. Roberto Gori from Argentina, for sharing these cases.
Introduction
Urinary incontinence (UI), defined as the symptom of involuntary loss of urine, is a bothersomer condition that negatively impacts the lives of millions of women. There are several subtypes of UI and the most common are: Stress incontinence (SUI), defined as the complaint of involuntary loss of urine on effort or physical exertion in which two processes can coexist bladder floor prolapse and alteration of urethral motility; and Mixed incontinence (MUI), defined as the complaint of involuntary loss of urine associated with urgency and also with effort (presence of both SUI and UUI).
The Pelvic Floor Ultrasound can help to identify whether there is one or both causes, in order to define suitable therapeutic strategy. The Ultrasound approach provide visualization in real time of the modifications that occur in the pelvic floor structures which are of interest to the physician. It is necessary not only the subjective evaluation, but also to use a method that allows to quantify the alterations and at the same time to be reproducible, for this, different parameters are evaluated such as "descent" of the different pelvic organs and angles of the urethra with different reference points (urethral angle (UTA), urethral rotation angle (URA), and the retrovesical angle (RVA)).
It is known that, when faced high-grade prolapses, patients may also present urethral motility changes, so it is important to take into account that bladder floor repairing without correcting the urethral abnormality could transform SUI ´patients to Continuous urinary incontinence´s ones.
In other cases, we can find alterations in urethral motility without a cystocele. In this case, it is important to detect if there are changes in the Levator Ani Muscle compression on the urethra (continence effect), by ultrasound with the findings of changes in the urethral angle. In addition, it must be determined if there is an incompetence of the internal or intrinsic urethral sphincter. In SUI cases, the solution to the problem is not always surgical; perhaps with a muscular reeducation of the pelvic floor it is enough, thus being able to avoid or delay surgery until a moment when it is more effective.
Clinical Cases
Case 1
Age: 48-year-old patient
Pregnancies 3 - Deliveries 2 - Abortions 0
Medical history: No history of surgery or pulmonary pathologies, without diabetes, hypertension or smoker. Ultrasound requested to rule out SUI without clinical presence of cystocele.
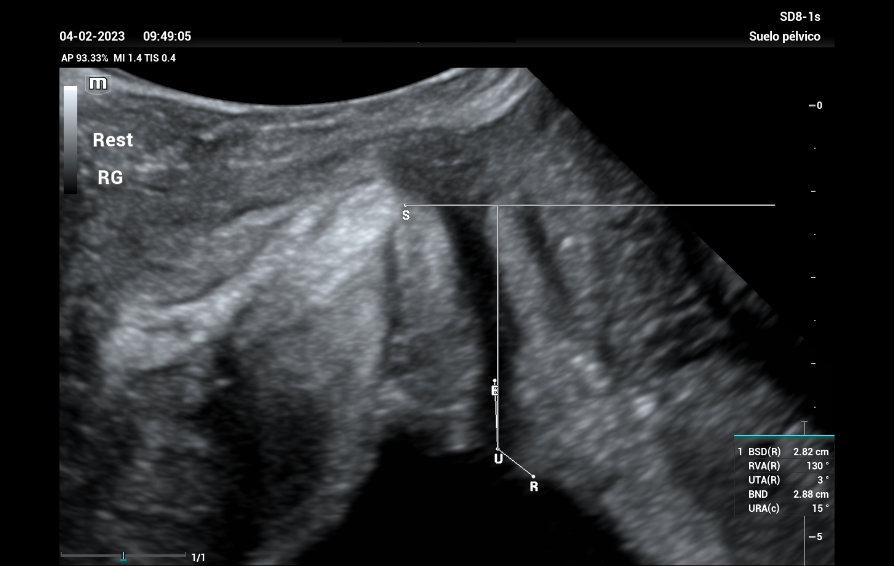
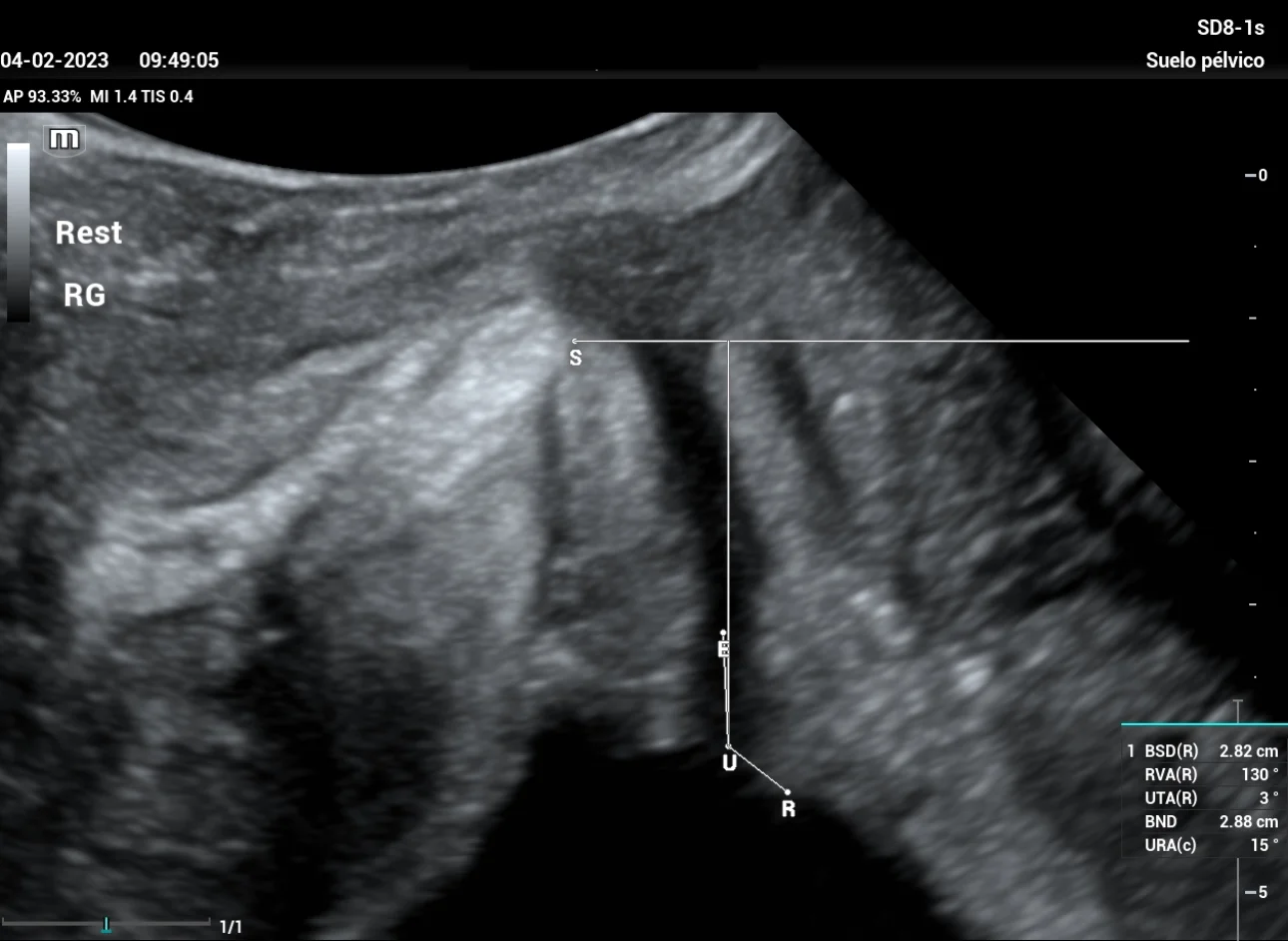
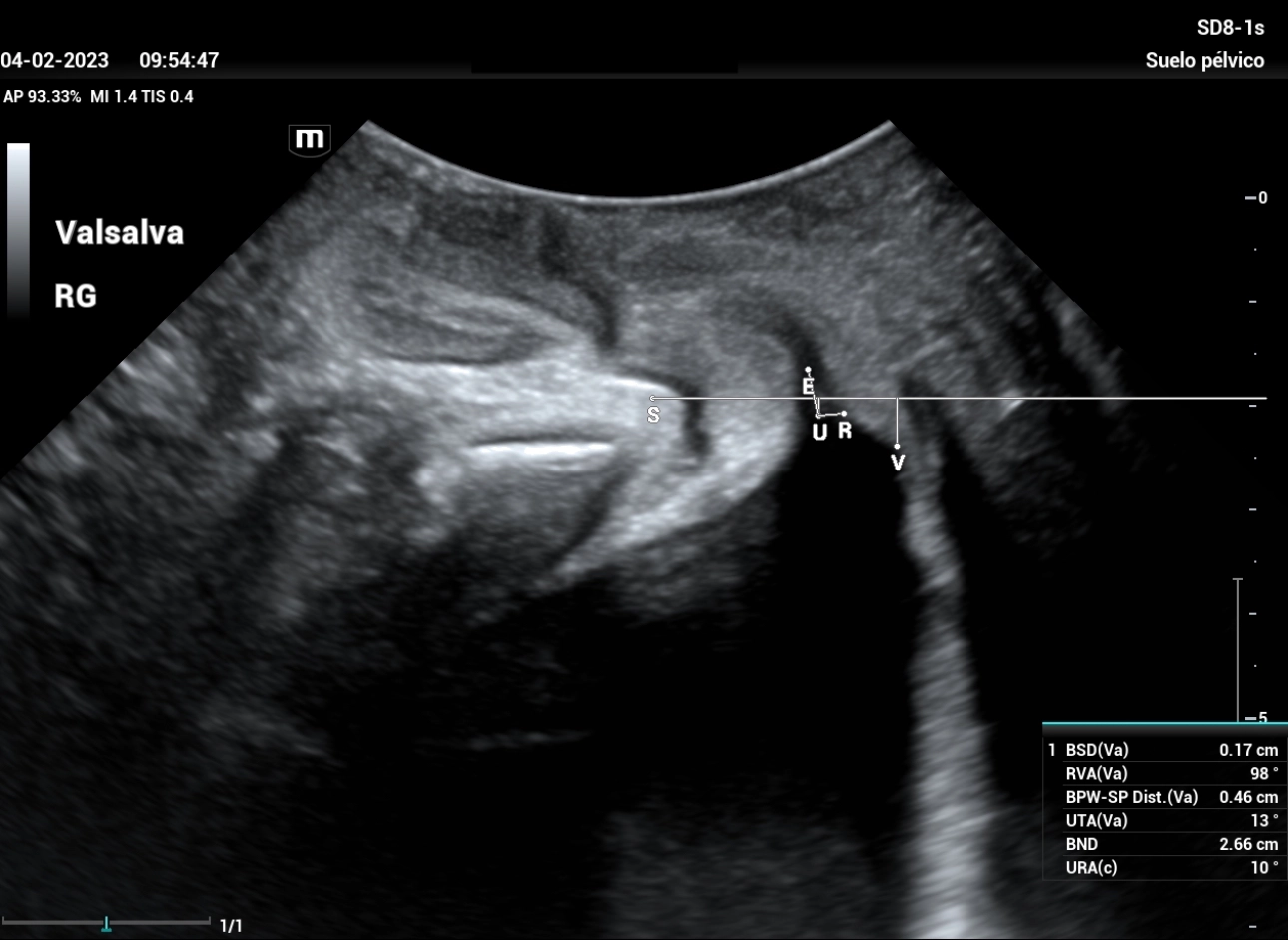
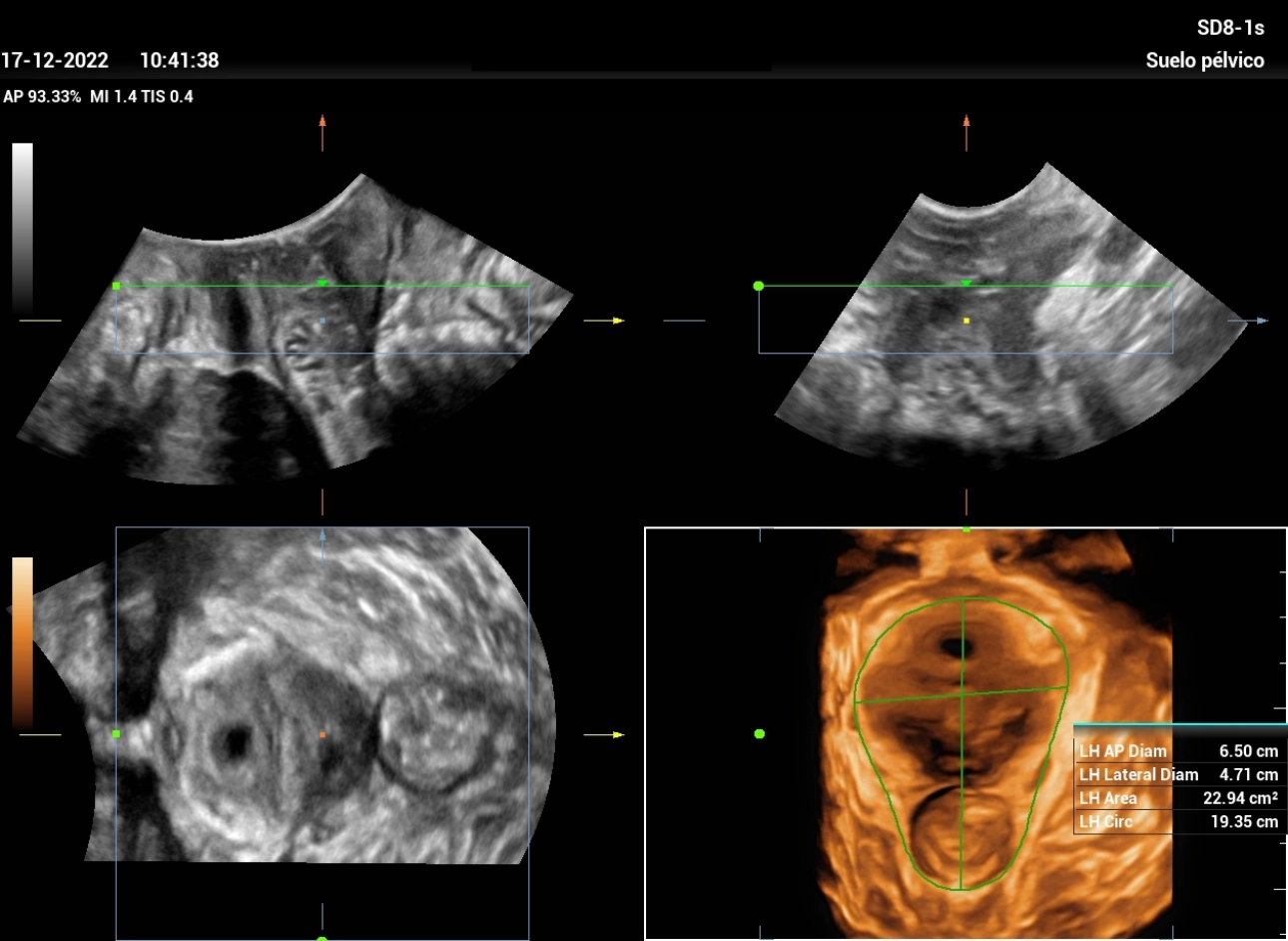
A study was carried out with filling bladder of 300 ml. The reference line is set at the inferior margin of the symphysis pubis, giving a total result of Bladder neck descent (BND) of 28mm, a UTA angle of 3º and a beta angle (RVA) of 130º (Figure 1), both within normal parameters, we performed the Valsalva maneuver showing a 26mm descent, and after maneuvering of Valsalva (Figure 2) a UTA angle of 13º (10º rotation) is observed, RVA of 98º.
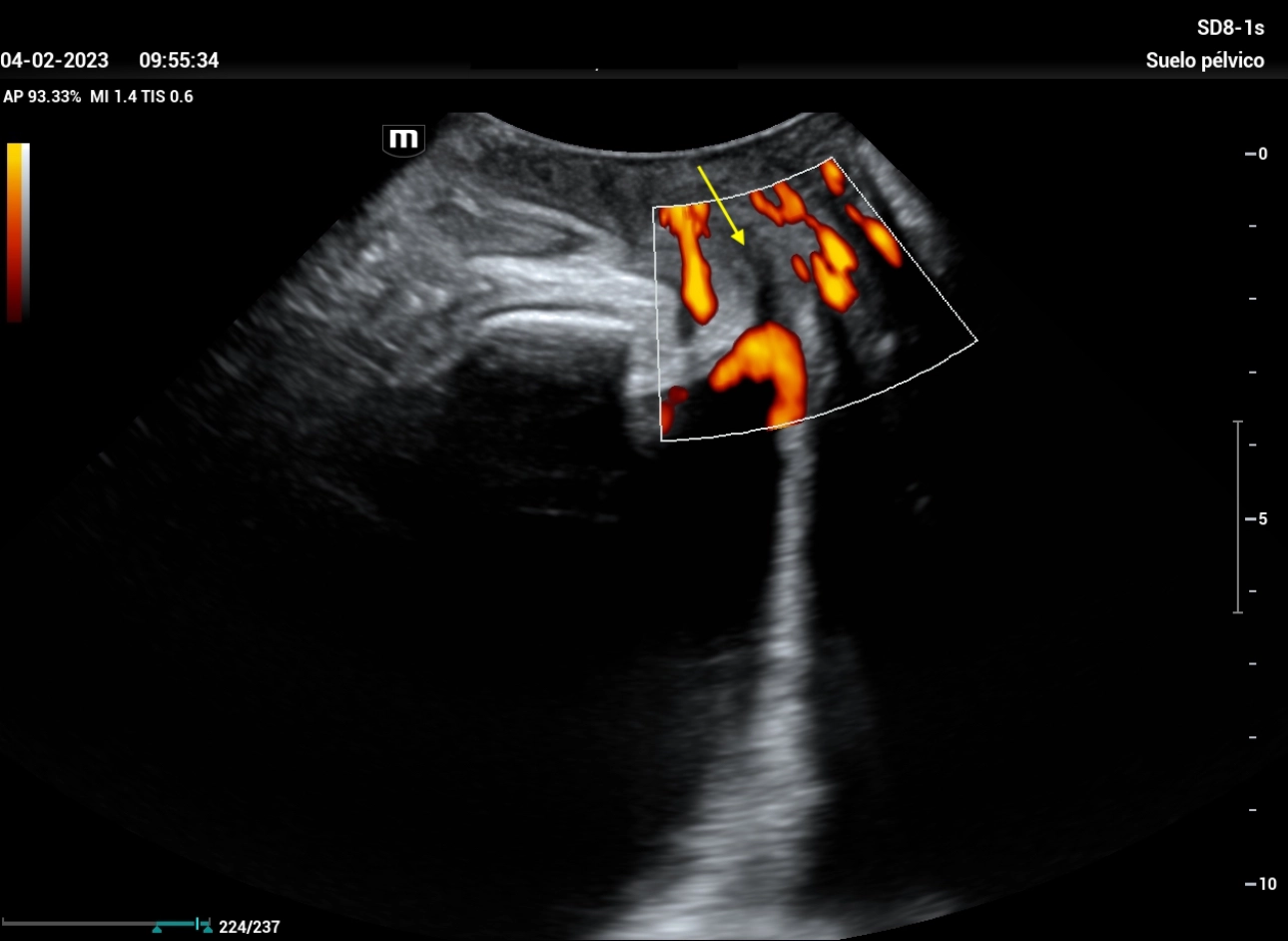
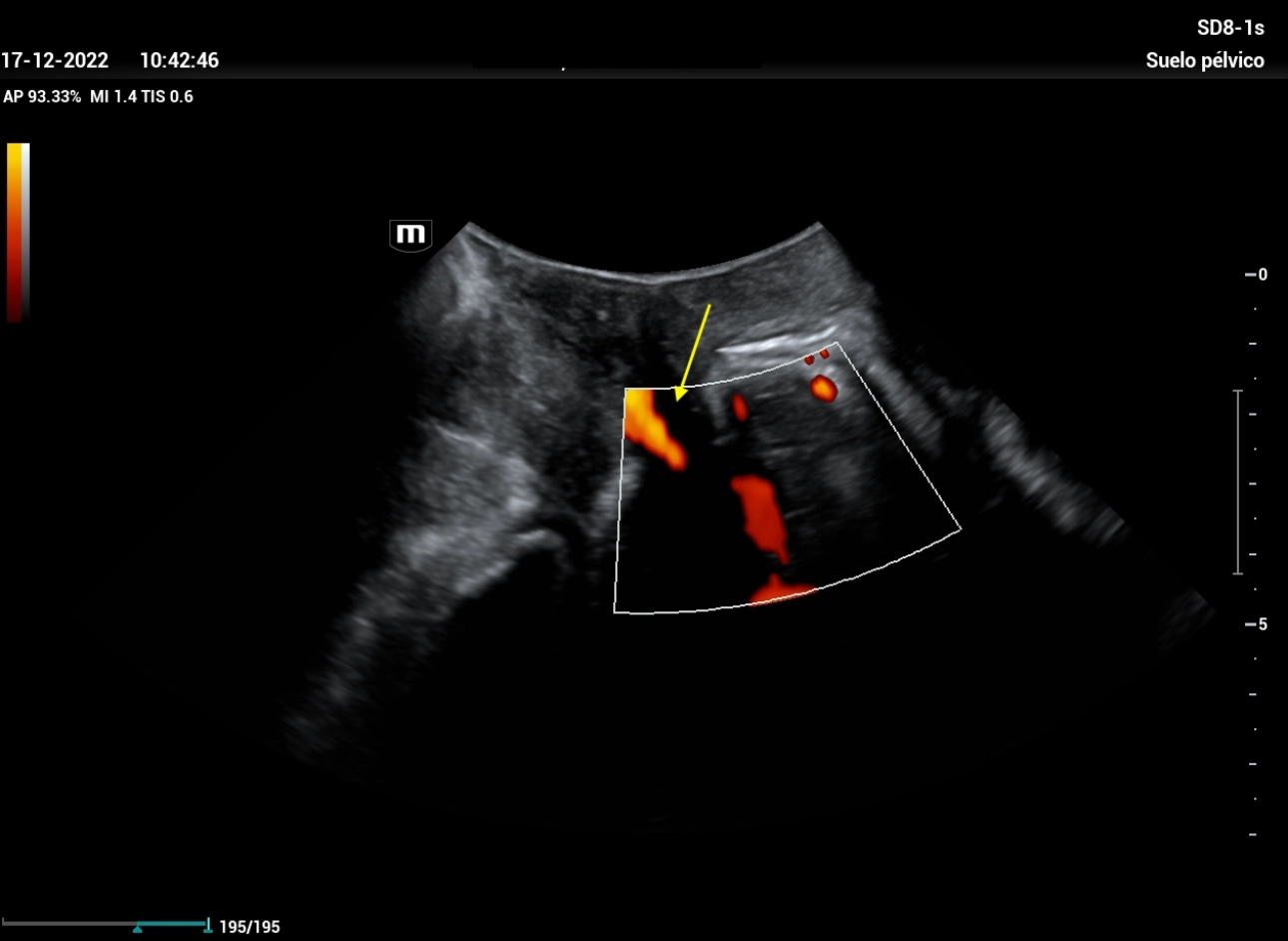
It is examined with color Doppler without filling of the urethra, which infers internal sphincter competence (Figure 3). After evacuating the bladder, a post-micturition residue of 8 ml and a detrusor thickness of 3.4 mm were found. When evaluating the hiatus in 3D, at rest and after Valsalva, a ‘normal’ distensibility of the levator hiatus is observed. (Figures 4 and 5)
Case 2:
Age: 53-year-old patient
Pregnancies 4 - Deliveries 2 - Abortions 2.
Medical history: with a history of appendectomy, and high blood pressure, without pulmonary pathologies, or diabetes, not a smoker. Ultrasound requested to rule out SUI without clinical presence of cystocele.
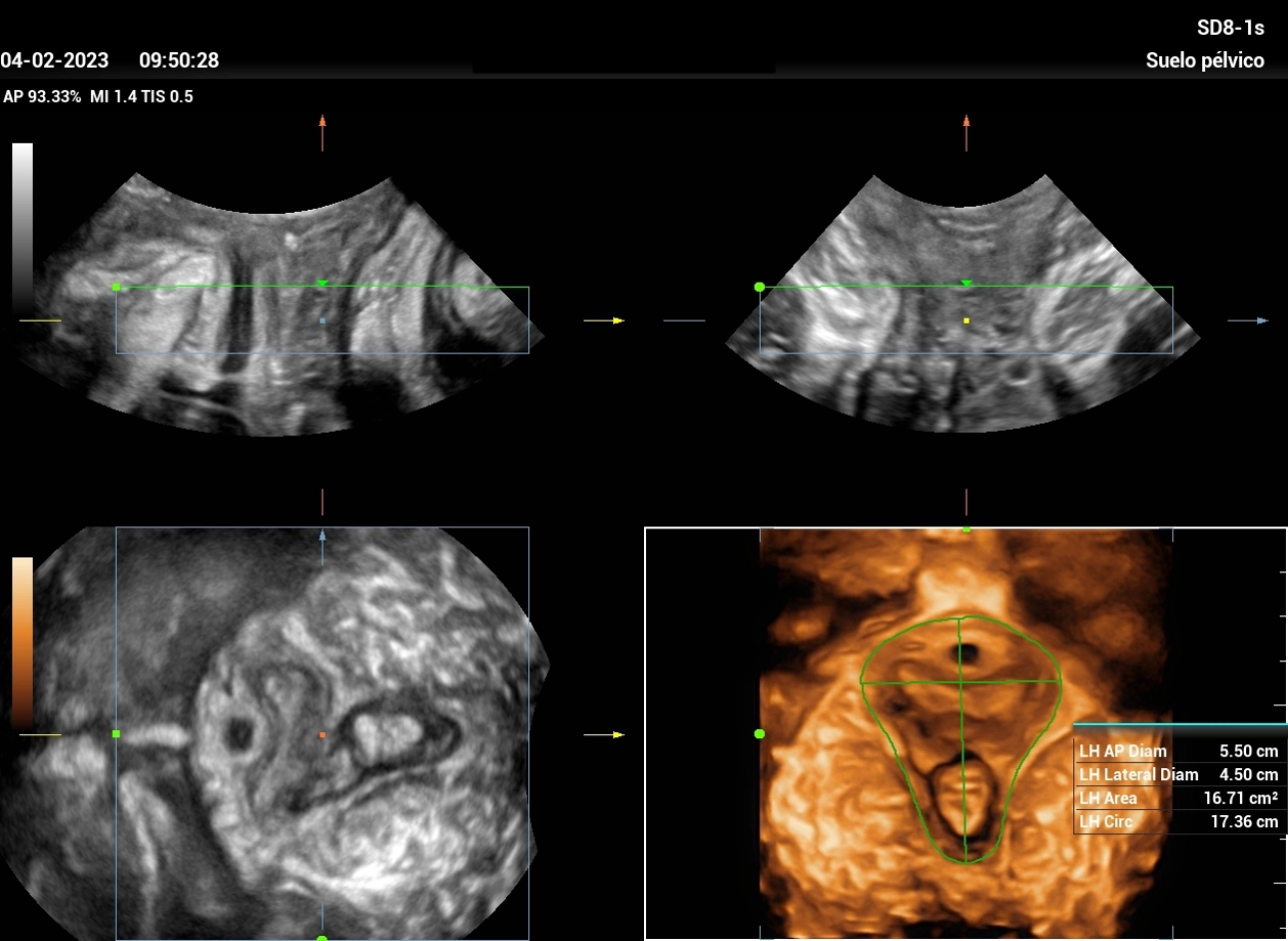
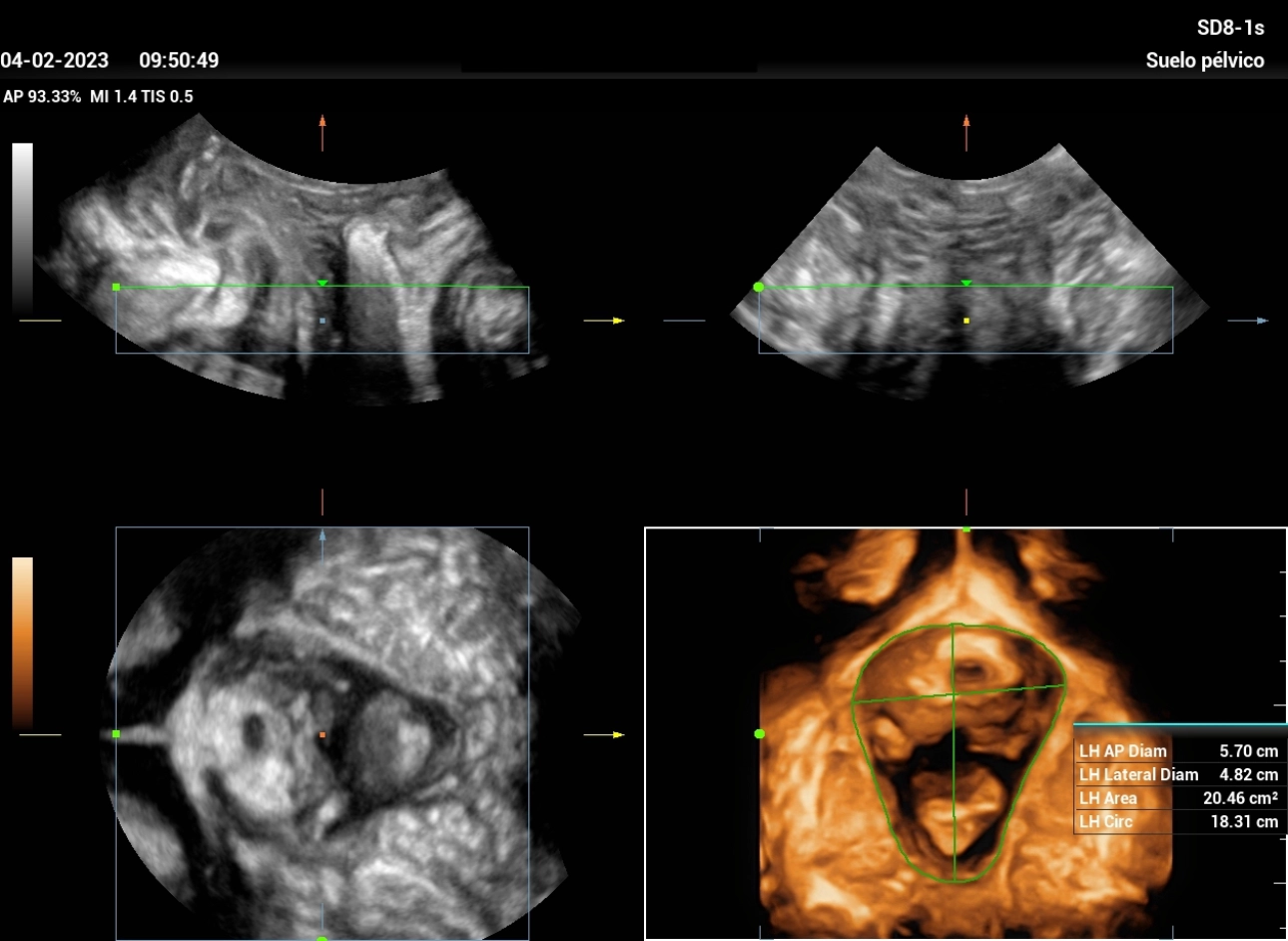
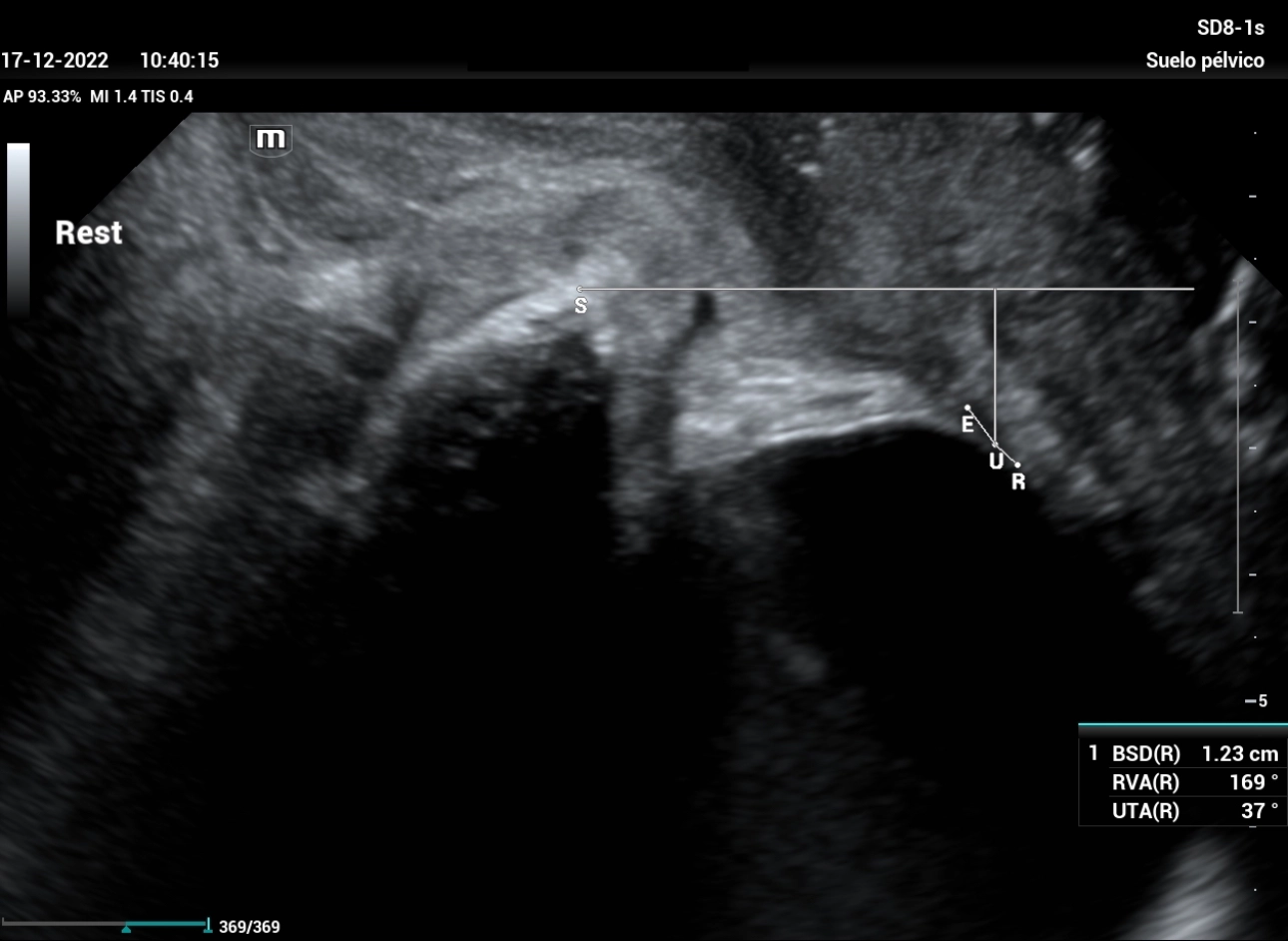
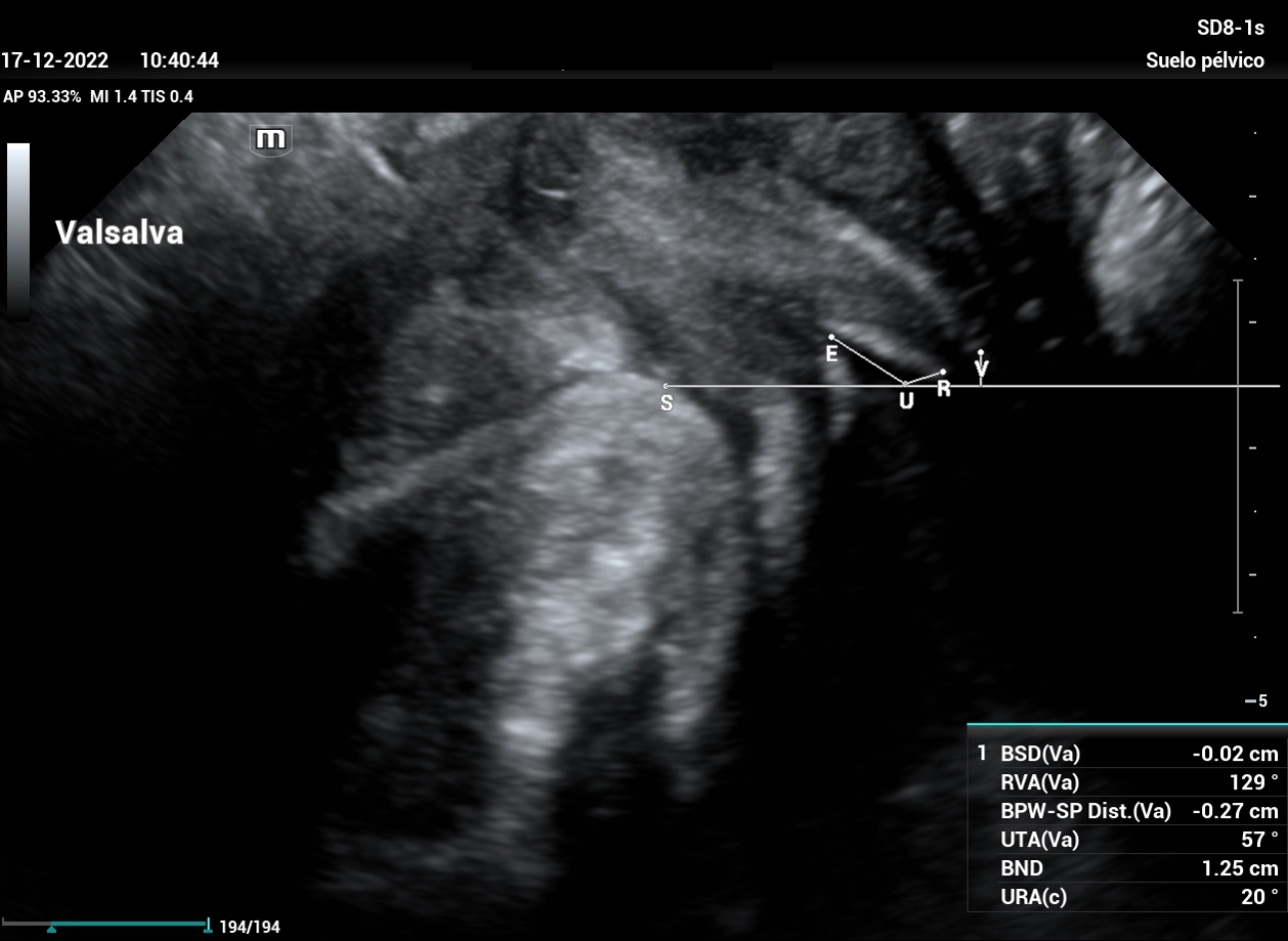
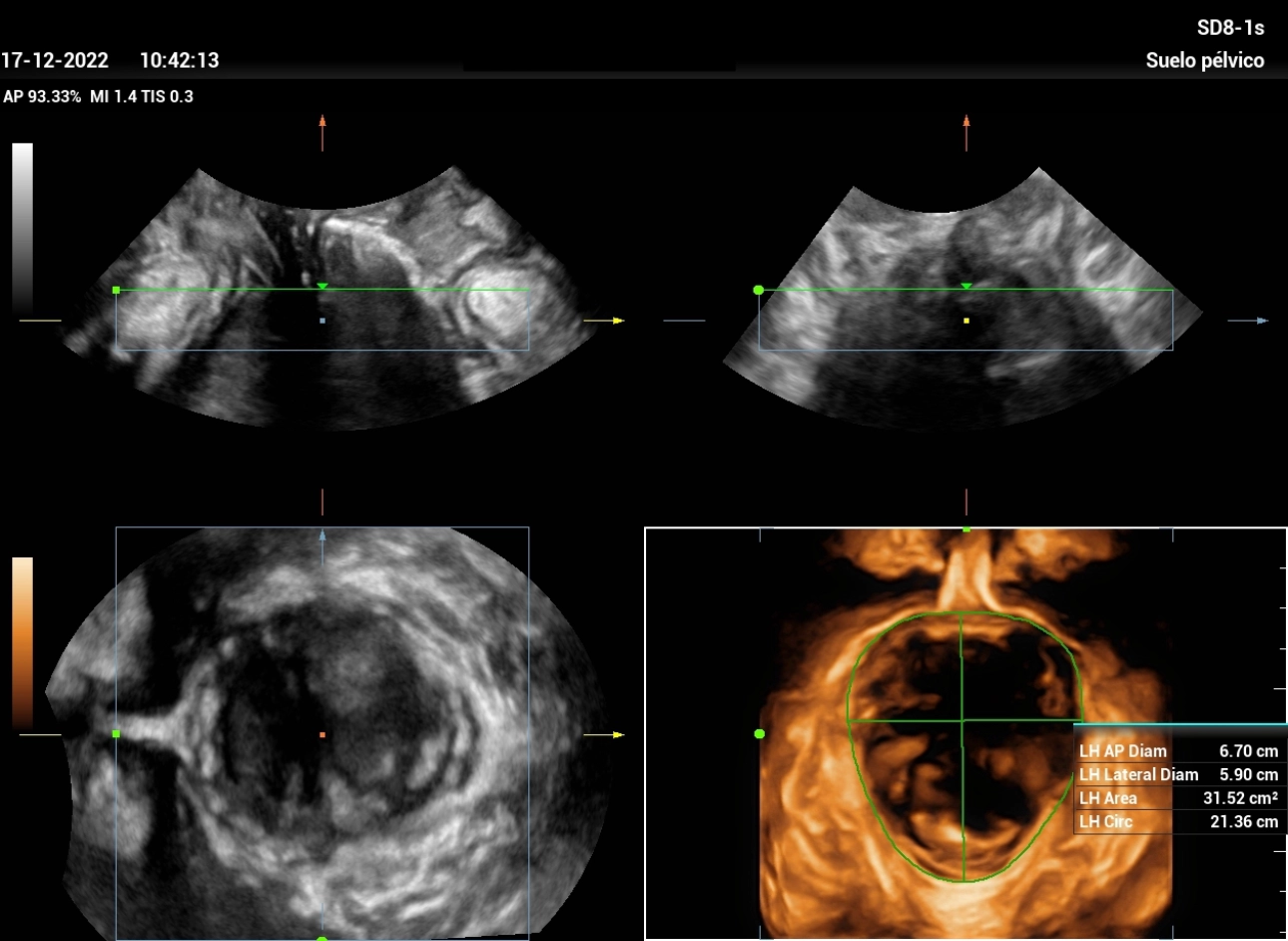
A study was carried out with a 200 ml filling bladder, with a Bladder neck symphyseal distance (BSD) result within normal values, a UTA angle of 37º and a beta angle (RVA) of 169º (Figure 6), both within normal parameters, and when performing the Valsalva maneuver (Figure 7), the bladder neck is below the reference line, and funneling of the bladder neck is observed. With color Doppler the urethra is filled, inferring internal sphincter incompetence (Figure 8). After evacuating bladder, a post-void residue of 14 ml and a detrusor thickness of 3.2 mm were found. When evaluating the hiatus in 3D, at Rest and Valsalva, we can observe the hiatal ballooning on Valsalva manoeuvre. (Figure 9 and 10)
Conclusion
The Pelvic Floor Ultrasound allowed us to define in case 1 that: the patient does present hypermobility of bladder neck, which maybe cause of SUI, that the urethral angles do not present an alteration that justifies surgical intervention. While in case 2, there is mild cystocele, with angle modifications within normal parameters, with intrinsic urethral sphincter incompetence.
Therefore, the patient in case 1 benefited from the Pelvic Floor scanning, combining the use of 2D and 3D, since it allowed re-education of the pelvic floor to be defined as a treatment. In the case of patient 2, drug treatment is recommended, and if it fails, surgical correction should be performed.
Both cases allow us to understand the importance of using a diagnostic method complementary to the physical examination, not only to determine the type of incontinence, but also the therapeutic approach. Due to its practicality, simplicity and low cost, Pelvic Floor Ultrasound is the best choice method.