Ultrasound Journal 17 - Multiparametric ultrasound approach in the differential diagnosis of focal pathology of the mammary glands
2023-08-14
Introduction
Patient B., 53 years old, complained of compaction and pain in the left breast. On examination, a dense painful formation with an approximate size of 3 cm, mobile, not connected with the skin, was determined in the left mammary gland. According to digital mammography, Fibrocystic mastopathy, Birads 2 was diagnosed.
B-mode and Doppler modes
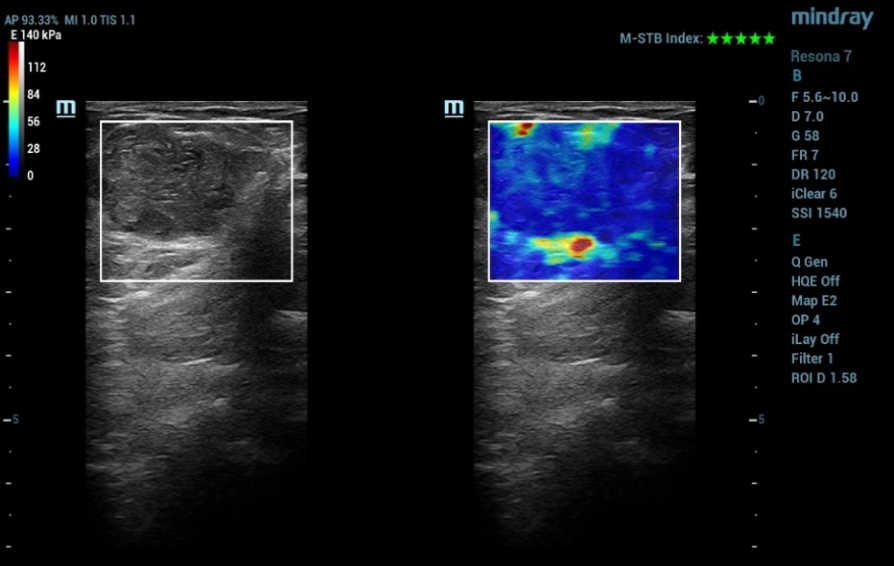
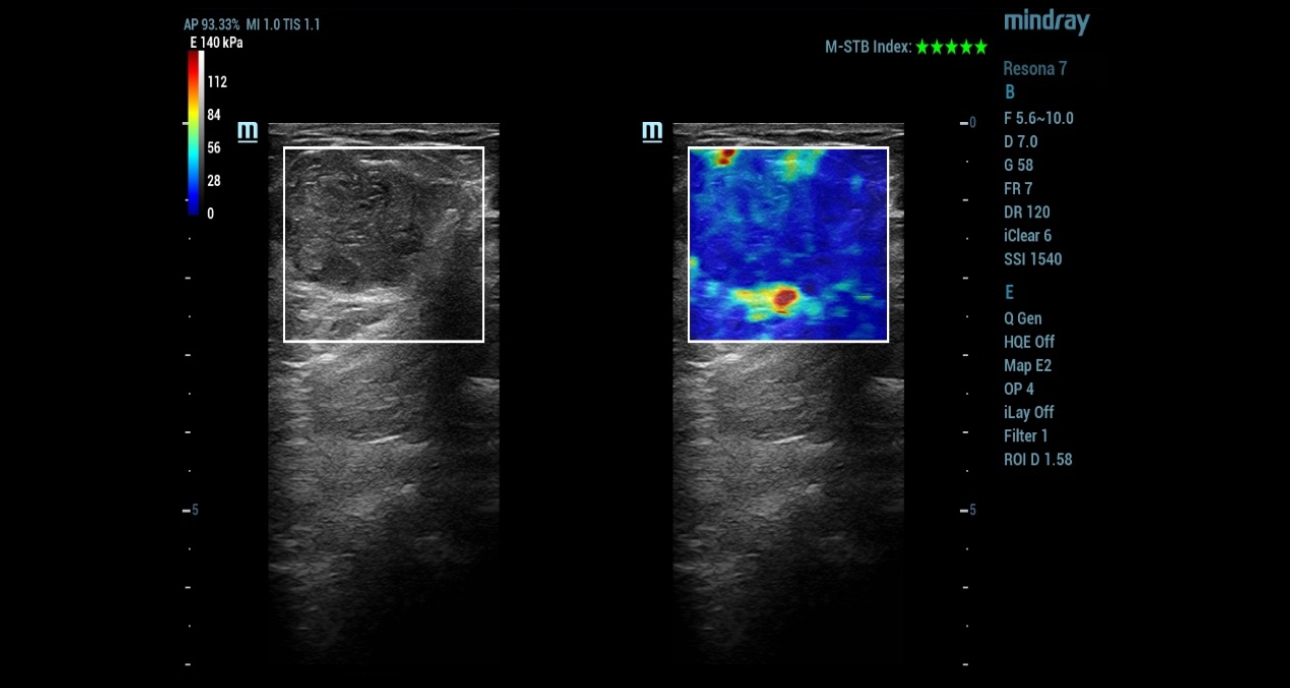
Ultrasound examination was performed on the Resona 7 ultrasound machine (Mindray, China) using a linear high-frequency transducer (up to 18 MHz). In the upper outer quadrant of the left breast, at 13 o'clock, an isoechoic horizontally oriented formation with a smooth, clear contour measuring 40x25 mm was determined (Fig. 1).

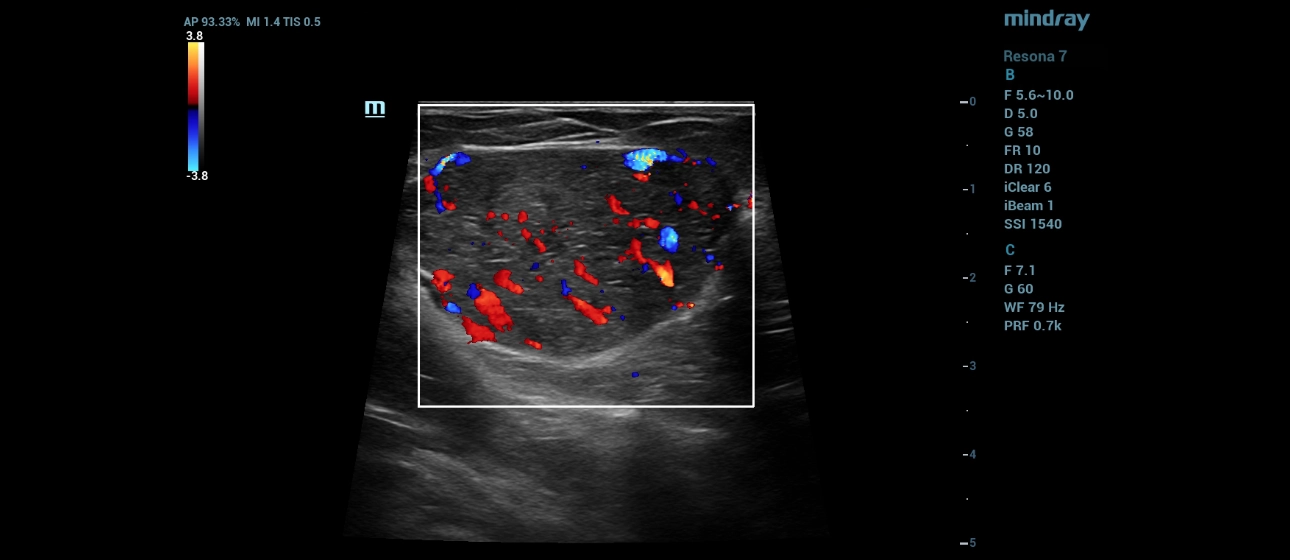
In Doppler modes, multiple uneven color loci were observed in the projection of focal formation (Fig. 2, 3).

Shear Wave Elastography
In the mode of elastography by a shear wave, the focal formation of the breast was uniformly colored in non-rigid blue tones (Fig. 4).
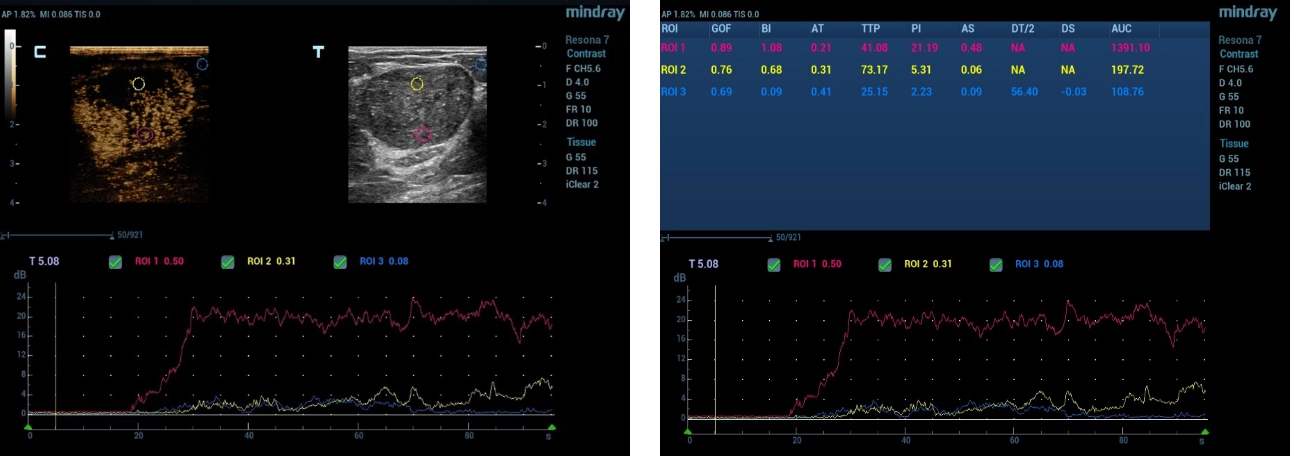
Ultrasound examination with contrast enhancement
In contrast, 2.4 ml of the finished mixture of the drug "Sonovue" (Bracco Swiss, SA, Switzerland) was used. Visualization was carried out immediately after injection for 2 minutes. Most of the focal formation of the mammary gland was characterized by hyperintensive contrast enhancement of relatively unchanged parenchyma, with rapid accumulation and slow leaching of contrast agent. A small part of the formation was characterized by an absence of contrast (Fig. 5).
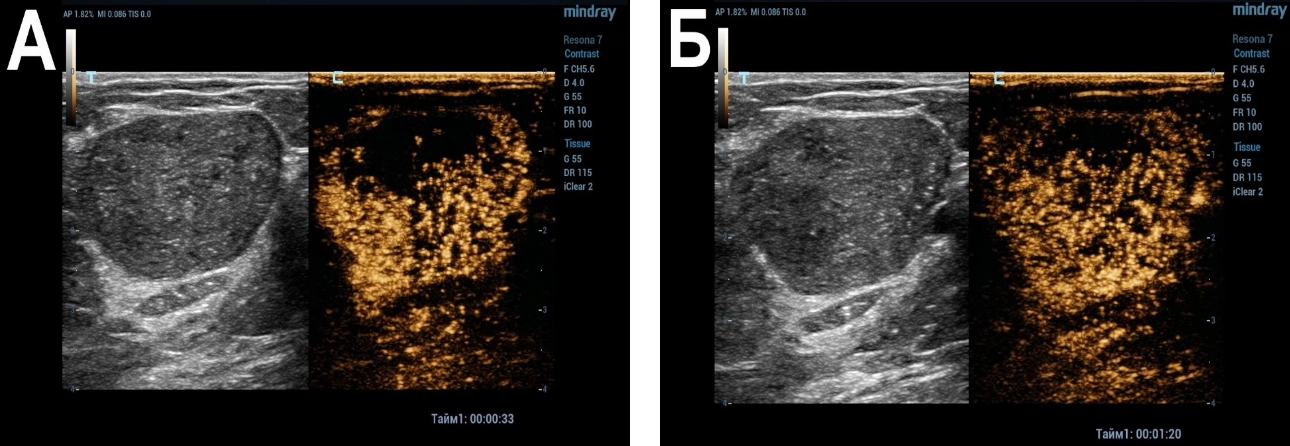
Quantitative analysis was performed by constructing accumulation curves. The time–intensity curve for focal formation was characterized by a rapid rise followed by a plateau phase. The main quantitative indicators were TTP 41.1, PI 21.2, AUC 1391.1, the parameter DT/2 was not determined. For the intact breast area and the hypointensive area of focal formation contrast, the time–intensity curves were characterized by a slight rise and a subsequent plateau phase, the parameters of TTP, PI, AUC were 73.2; 5.3; 197.7 and 25.2; 2.2; 108.8, respectively. The parameter DT/2 was not determined in the intact area, in the hypointensive area of focal formation contrast was 56.4 seconds. (fig. 6).
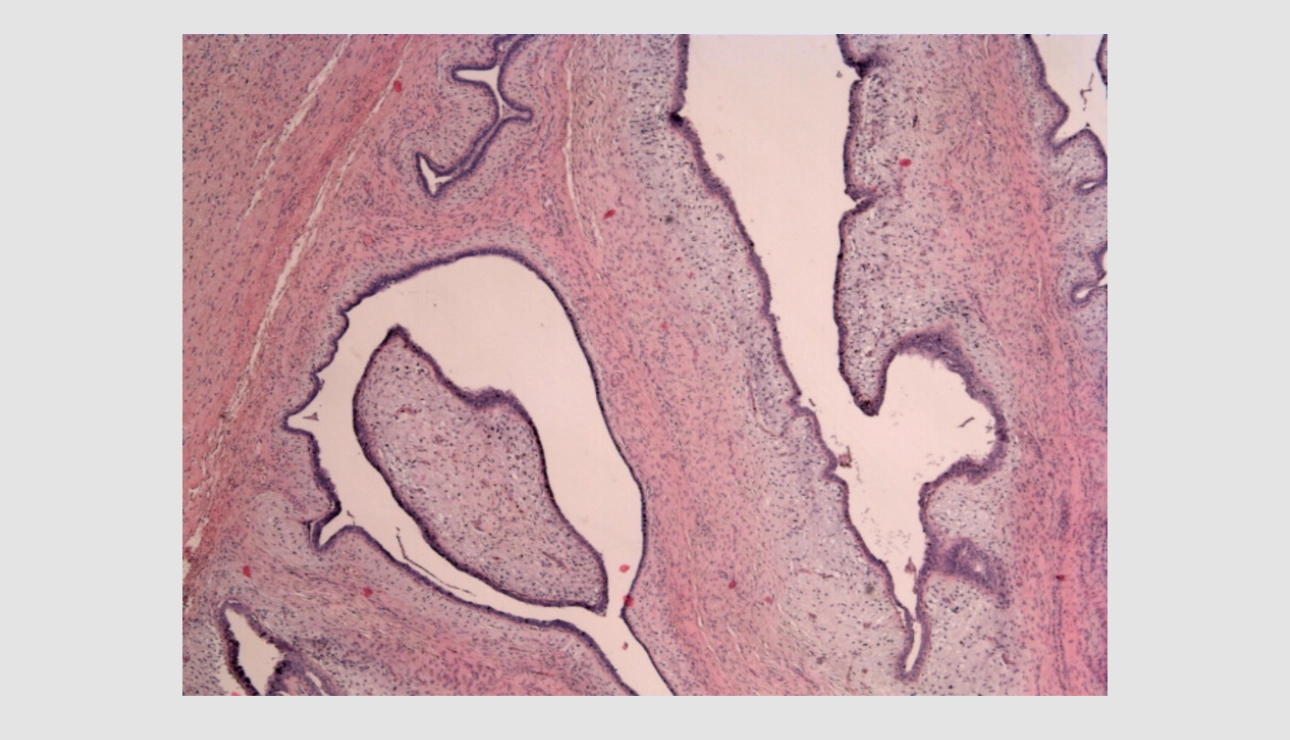
Biopsy result
Resection of the focal formation of the left breast was performed at the Republican Clinical Oncological Dispensary of the Ministry of Health of the Republic of Tatarstan named after Professor M.Z. Sigal. According to the results of histological examination, a benign phylloid breast tumor was diagnosed. In Figure 7: – pronounced stroma proliferation with the formation of "leaf-like" structures lined with normal single-layer glandular epithelium. Staining hematoxylin and eosin. The magnification is 50 times (Fig. 7).
Discussion
Breast cancer currently ranks first in morbidity and mortality among malignant diseases in women in the world [1].
Ultrasound examination is one of the most common methods of screening breast tumors, but differential diagnosis of focal formations based on B-mode and Dopplerography is not possible in all cases [2].
Angiogenesis is the basis of the tumor process in human tissues, including breast cancer [3].
However, signs of increased vascularization can be observed in both benign and malignant processes. Ultrasound with contrast enhancement allows you to visualize the smallest vessels with low-velocity blood flow in real time, as well as to conduct a quantitative analysis of the accumulation and leaching curve [4].
Evaluation of the effectiveness of quantitative analysis is currently an area of active study [5].
In this clinical example, the focal formation of the breast according to the B–mode and elastography by the shear wave was characterized as benign. According to the results of Doppler modes, there were signs of suspected neovascularization. Ultrasound with intravenous contrast also demonstrated increased vascularization of the formation with slow washout of the contrast agent. The quantitative analysis made it possible to objectify the data of qualitative analysis in the form of time-intensity curves and quantitative parameters.
Thus, the multiparametric approach made it possible to exclude neovascularization detected by Dopplerography, which was confirmed by morphological results.
Reference
[1] Menezes G.L., Knuttel F.M., Stehouwer B.L., Pijnappel R.M., van den Bosch M.A. Magnetic resonance imaging in breast cancer: A literature review and future perspectives. World J Clin Oncol. 2014 May 10;5(2):61-70. doi: 10.5306/wjco.v5.i2.61.
[2] Yuan Y, Xu M, Ren Y, He L, Chen J, Sun L. Clinical Value of Contrast-Enhanced Ultrasound in Breast Cancer Diagnosis. Comput Math Methods Med. 2022 Sep 5;2022:2017026. doi: 10.1155/2022/2017026. PMID: 36105240; PMCID: PMC9467778.
[3] Weidner N, Semple JP, Welch WR, Folkman J. Tumor angiogenesis and metastasis—correlation in invasive breast carcinoma. N Engl J Med 1991;324(1):1–8.
[4] Drudi, F., Cantisani, V., Gnecchi, M., Malpassini, F., Di Leo, N., & de Felice, C. (2012). Contrast-Enhanced Ultrasound Examination of the Breast: A Literature Review. Ultraschall in Der Medizin - European Journal of Ultrasound, 33(07), E1–E7. doi:10.1055/s-0031-1299408
[5] Boca Bene I, Dudea SM, Ciurea AI. Contrast-Enhanced Ultrasonography in the Diagnosis and Treatment Modulation of Breast Cancer. J Pers Med. 2021 Jan 30;11(2):81. doi: 10.3390/jpm11020081. PMID: 33573122; PMCID: PMC7912589.
