When the platelet (PLT) count is extremely low, is platelet transfusion really required? Let’s analyze the following case, which tells us a different answer.
Case background
A 49-year-old woman went to the emergency department due to transient cognitive disorder. She had obvious paroxysmal headaches, with vomiting and epigastric pain. Brain CT revealed no abnormalities. The laboratory results revealed anemia and severe thrombocytopenia. What should be expected?
Blood Test
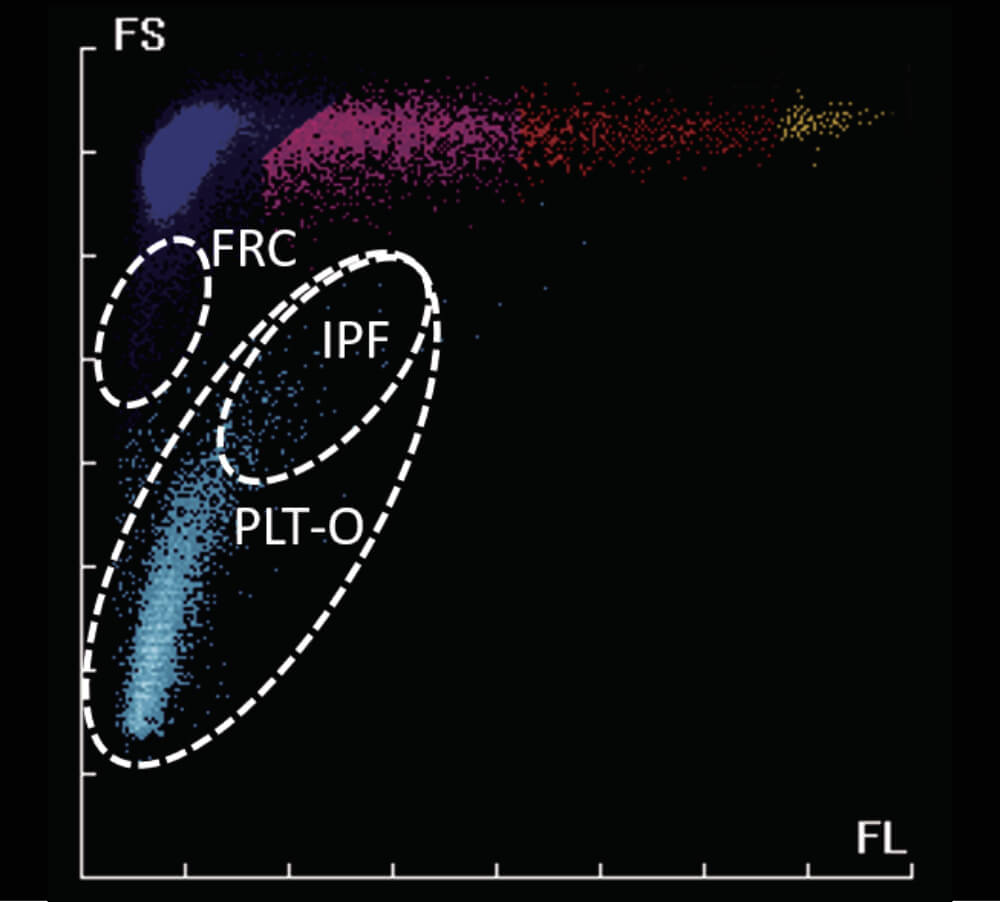
Blood test (Figure 1) showed low RBC count of 3.07×1012/L and low HGB concentration, which indicated anemia. PLT-O count was 15×109/L (CDR mode, Mindray BC-6200). Such a low PLT count and abnormal RBC-related parameters caught our attention: Should platelet transfusion be initiated?
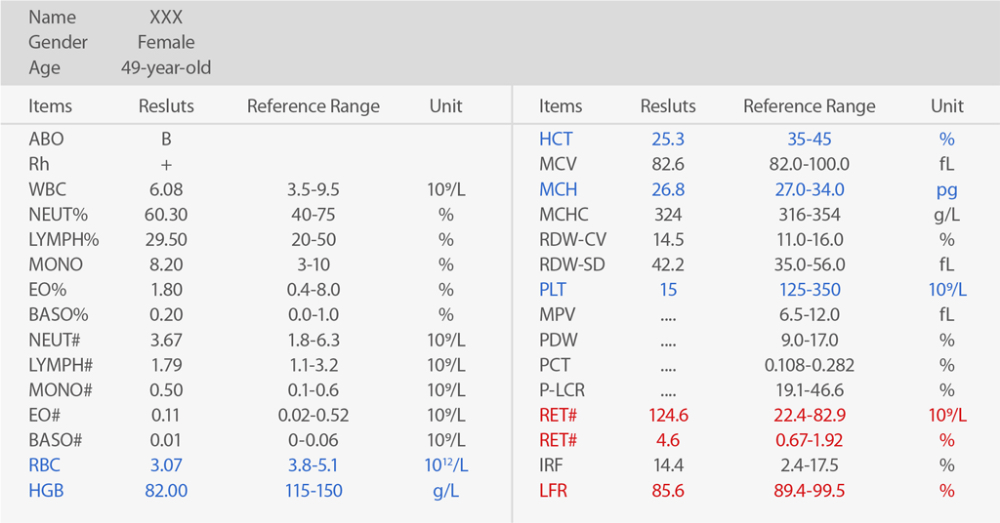
The PLT histogram was far from the normal ones. We then checked RET scattergram, in which few PLT dots were observed and RET increased (Figure 2).
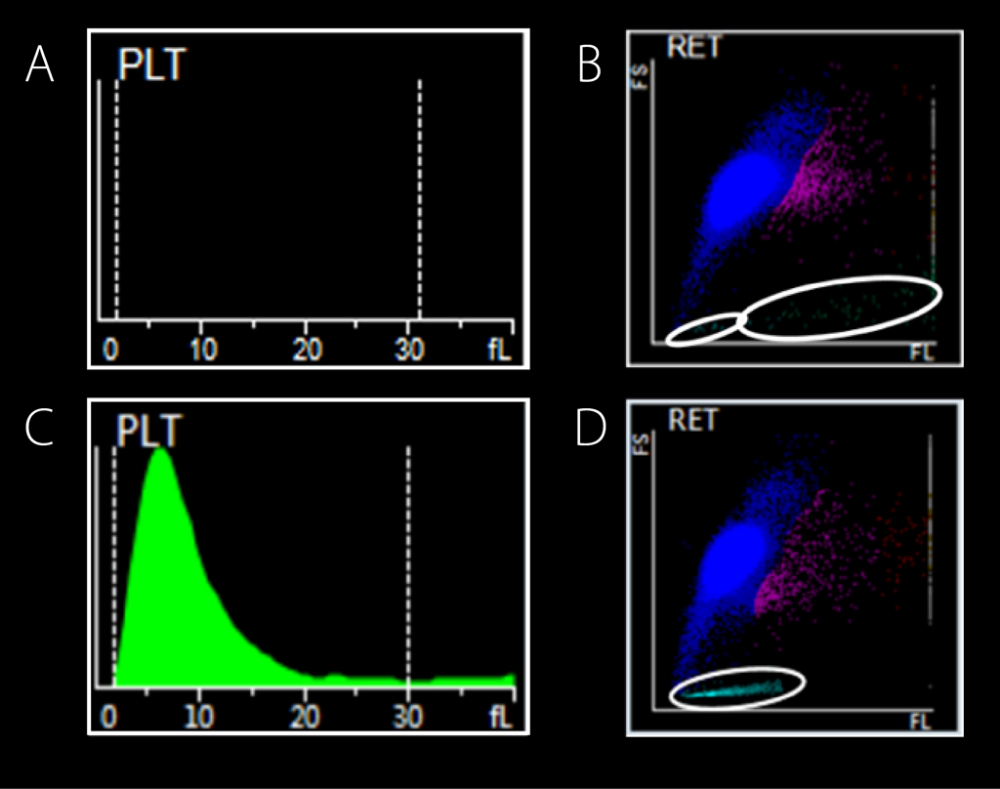
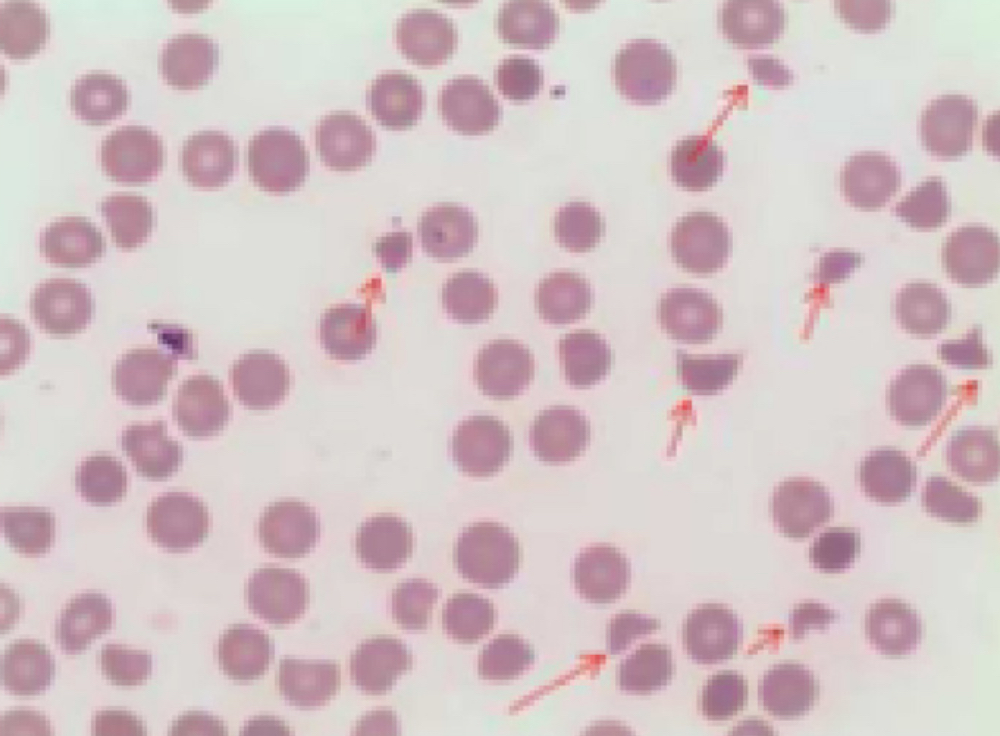
These abnormal results triggered the re-exam rule, and then the peripheral blood smear was reviewed (Figure 3). The result demonstrated evidence of intravascular hemolysis, which included schistocytes, a small number of spherocytes, helmet cells, and thrombocytopenia.
Bone Marrow Examination
Erythrocytic cell lines 44%, Granulocytic cell lines 40%, G/E=0.91/1.
Undifferentiated erythroblasts were common in the bone marrow smear, and Howell-Jolly body were found. A total of 257 megakaryocytes were found in the smear, and 50 were differentiated, including 3 megakaryoblasts, 44 promegakaryocytes and 3 naked nucleus megakaryocytes. PLT was rarely seen. Such bone marrow smear showed a megakaryocytic thrombocytopenia, increased function of erythroid differentiation.
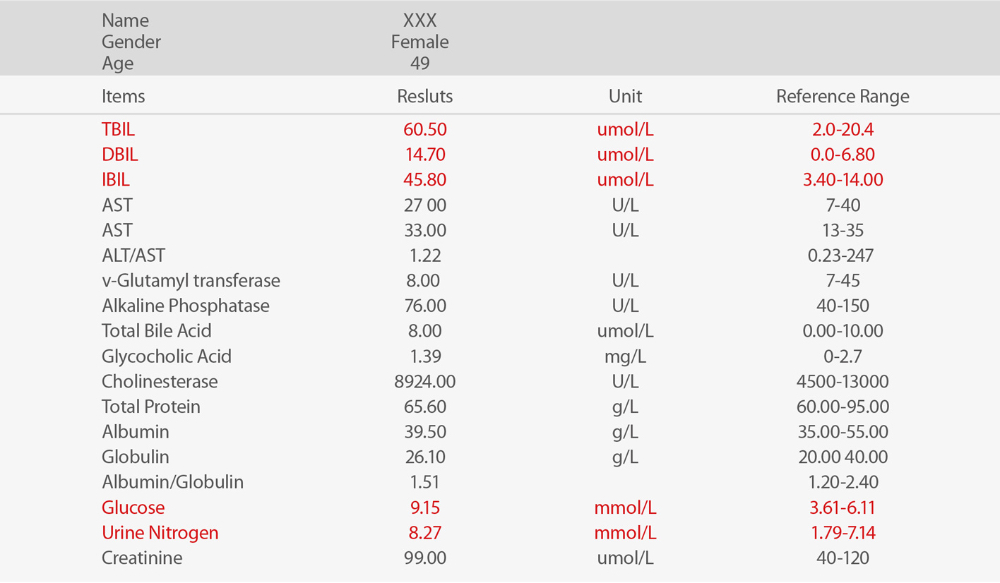
Chemistry Test
In the chemistry test, the result of total bilirubin (TBIL) increased, indirect bilirubin (IBIL) increased, which showed hemolytic disease.
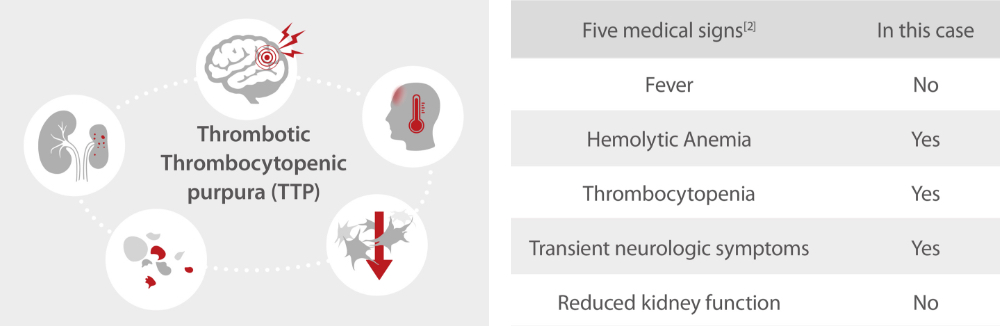
Considering the cases with typical symptoms:(1) hemolytic anemia (schistocytes); (2) thrombocytopenia; (3) neurologic symptoms (transient mental disorder), thrombotic thrombocytopenia (TTP) disease is likely. The results and TTP diagnostic suggestion were transferred to doctors immediately. And Further ADAMTS13 testing confirmed TTP. Finally, plasma exchange instead of platelet transfusion was taken.
Conclusion
If the PLT level is lower than the decision-making threshold, experienced doctors will immediately recheck whether the specimen is qualified, the histogram and scattergram are normal or not and any other abnormal cell counting results or significant flag messages, etc. Further confirmation will be carried out by blood smear examination under the microscope. Finally, after considering the patient's symptoms and medical history information, the laboratory can report the results and provide possible diagnosis.
Mindray’s automatic 8x PLT-O counting (SF Cube technology) provides accurate and stable counting for thrombocytopenia samples. Together with high quality blood smear from SC-120 Auto Slide Maker, Mindray hematology solutions support efficient management of thrombocytopenia. PLT-O is available in Mindray BC-6000 Series Auto Hematology Analyzers and the CAL 8000/6000 Cellular Analysis Lines.
Extension: Why is platelet transfusion not recommended in thrombotic thrombocytopenia?
Common causes of thrombocytopenia include decreased production in bone marrow, increased destruction in peripheral blood, and medication induced[1].
Thrombotic thrombocytopenia, including TTP in this case, is a kind of disease caused by increased PLT destruction. Because of von Willebrand factor (VWF) cleavage protease (ADAMTS13) deficiency, VWF cannot be cut off normally, and ultra-large VWF (ULVWF) accumulate, resulting in abnormal PLT aggregation, microthrombosis and fragmented RBC[2]. Under such condition, platelet transfusion may accelerate thrombosis, leading to worsening symptoms[3]. So for thrombotic thrombocytopenia, the main treatment should be plasma exchange.
Acknowledgement:
We would like to extend our thanks to Dr. Xiao Zuomiao, Dr. Chen Xianchun, Dr. Xiao Dejun and Dr. Luo Shi from Ganzhou People’s Hospital, China, for providing the case information.
References:
[1] What Is Thrombocytopenia? - NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 2015-05-01.
[2] Tsai, Han-Mou(2010). “Pathophysiology of thrombotic thrombocytopenic purpura.” International journal of hematology vol. 91,1: 1-19. doi:10.1007/s12185-009-0476-1.
[3] Joly, BS; Coppo, P; Veyradier, A (2017). "Thrombotic thrombocytopenic purpura." Blood. 129 (21): 2836–2846. doi:10.1182/blood-2016-10-709857.