In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Case introduction
A 55-year-old female patient underwent arthroscopic surgery at a local hospital on June 3, 2021, due to pain in the right shoulder joint. The patient returned to the ward at 17:00, and at 23:00, she presented with chest heaviness, breath fatigue together with palpitations, and profuse sweating, with an SBP of 170-180 mmHg, and an HR of 100 bpm.
Chest pain occurred an hour later, and the 12-lead ECG report was suggestive of myocardial infarction of “the inferior wall and high lateral wall". The patient was considered to be in critical condition and was immediately transferred to a local specialist center. Echocardiography was suggestive of “diffuse myocardial hypokinesis".
The patient was admitted into the ICU after tracheal intubation. She presented ventricular fibrillation once after cardioversion by defibrillator, but the patient still experienced persistent hemodynamic instability. Relying on high-dose norepinephrine plus epinephrine to maintain hemodynamic stability, as well as VA-ECMO supported by the ECMO team in a superior hospital, the patient was transported to the ICU of the superior hospital at 07:22 on June 4 after a 3-hour patient transfer.
Primary diagnosis:
- Acute myocardial infarction (inferior and extensive anterior myocardial infarction), lethal arrhythmia (ventricular fibrillation), acute heart failure, post cardiopulmonary resuscitation, VA-ECMO supportive;
- Pulmonary edema, acute respiratory failure
Treatment after transfer to the superior hospital:
2021-06-04
Coronary CTA test:
No stenosis in the left coronary artery (LMCA), left anterior descending coronary artery (LAD), circumflex branch of the left coronary artery, and the right coronary artery; left ventricular angiography showed: diffuse ventricular wall motion decrease.
Echocardiography:
Heart function parameters: LVDd: 48 mm
LVEF: 20%M-mode
2-DE: normal dimension of atrium-ventricle, no enlargement of the ascending aorta, an obvious primary wave, a clear dicroitic wave, and a clearly visible aortic valve that opened and closed normally; a slender mitral valve composed of an anterior leaflet with two waves, and a posterior leaflet moving in the opposite direction to the anterior leaflet.
Ventricular wall thickening is absent, and movement of the ventricular septum and the posterior wall of the left ventricle is in opposite directions.
Obvious attenuation of beats of the middle segment and apex of the left ventricle at rest, and fair motility of its base.
DOPPLER: Color Doppler ultrasound showed signals of small amounts of regurgitation through the mitral and tricuspid valves.
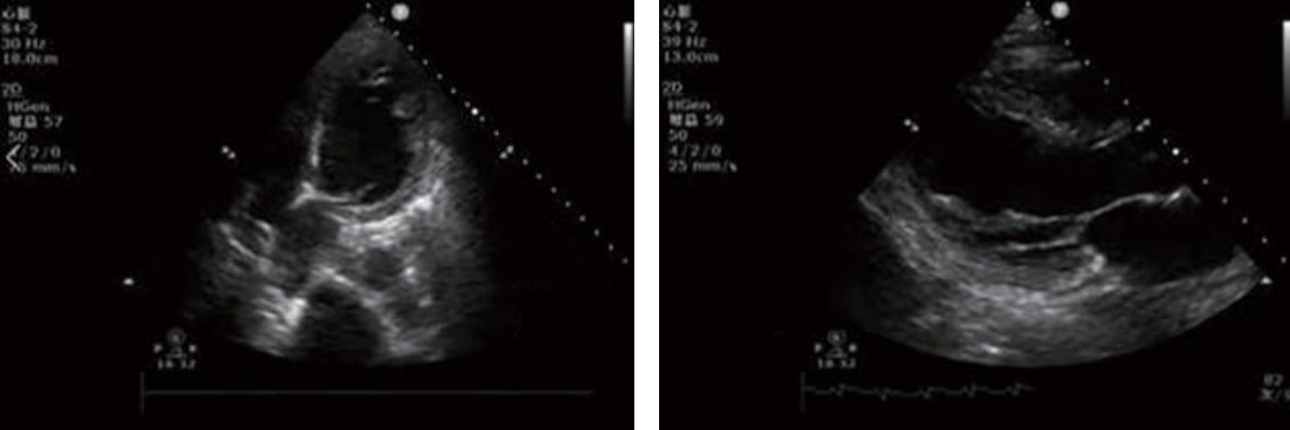
Diagnostic comments: Decreased left ventricular systolic function (LVEF: 20%), Takotsubo syndrome (stress cardiomyopathy) to be excluded, and mild mitral and tricuspid regurgitation.
The medical history recorded that the patient has a hyperglycemia for nearly 5 years without treatment, and is prone to impulsivity, while details about diagnosis remain unknown. Suspected Takotsubo syndrome was considered?
2021-06-04 - 2021-06-05
Early morning
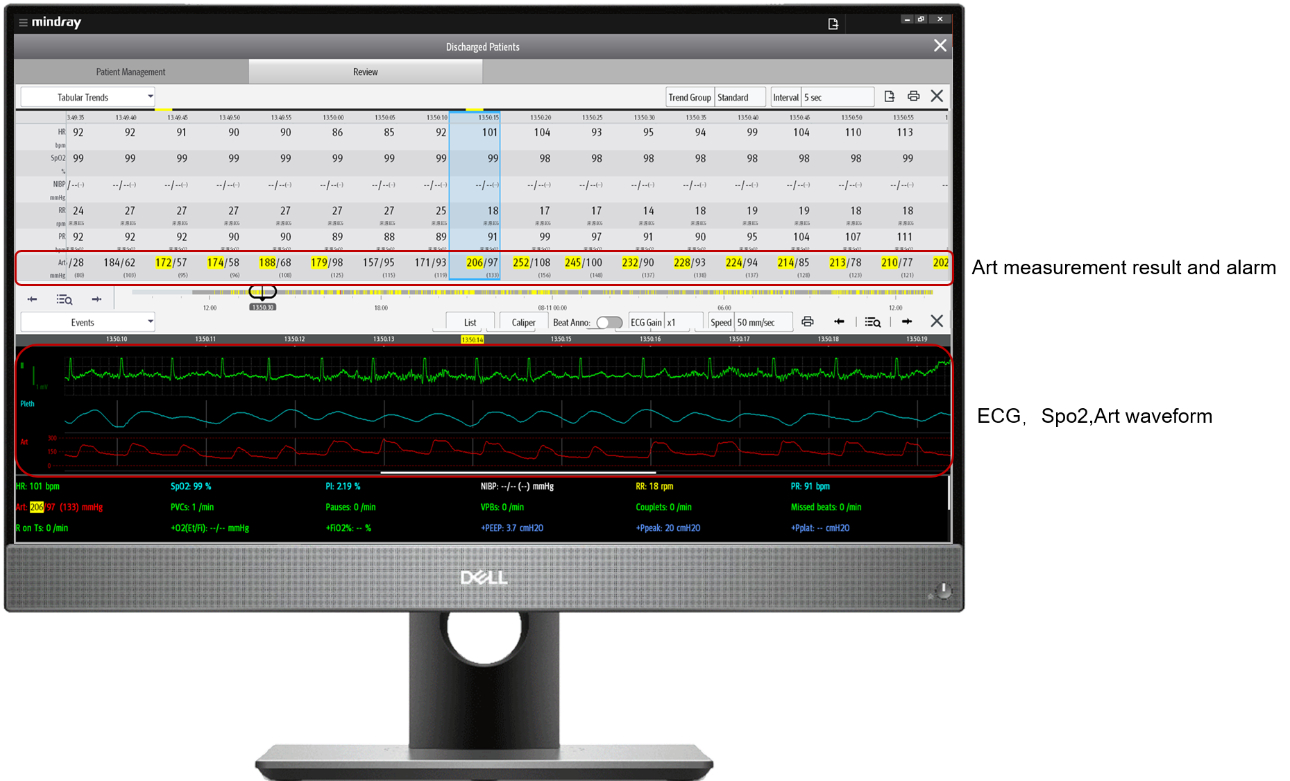
The physician in charge repeatedly received an alarm that the patient's IBP exceeded the limit from the application“Mobile Viewer” in his phone (Figure 2).
Through the Mobile Viewer, the doctor found that the patient presented with multiple episodes of abnormal IBP after admission into hospital. The ECG and SPO2 were normal, however, the IBP increased up to 207/187 mmHg and dropped to 60/49 mmHg within a few minutes (as shown in Figure 3). The doctor checked both real-time and historical vital signs in the WorkStation. Wondering what caused the multiple dramatic spikes and drops of the IBP?
2021-06-05
Morning
Daily Case Discussion in the morning: this patient's condition was complicated and given such condition, the director checked the patient's real-time and historical vital signs and discussed inside the team. (As shown in Figure 4)

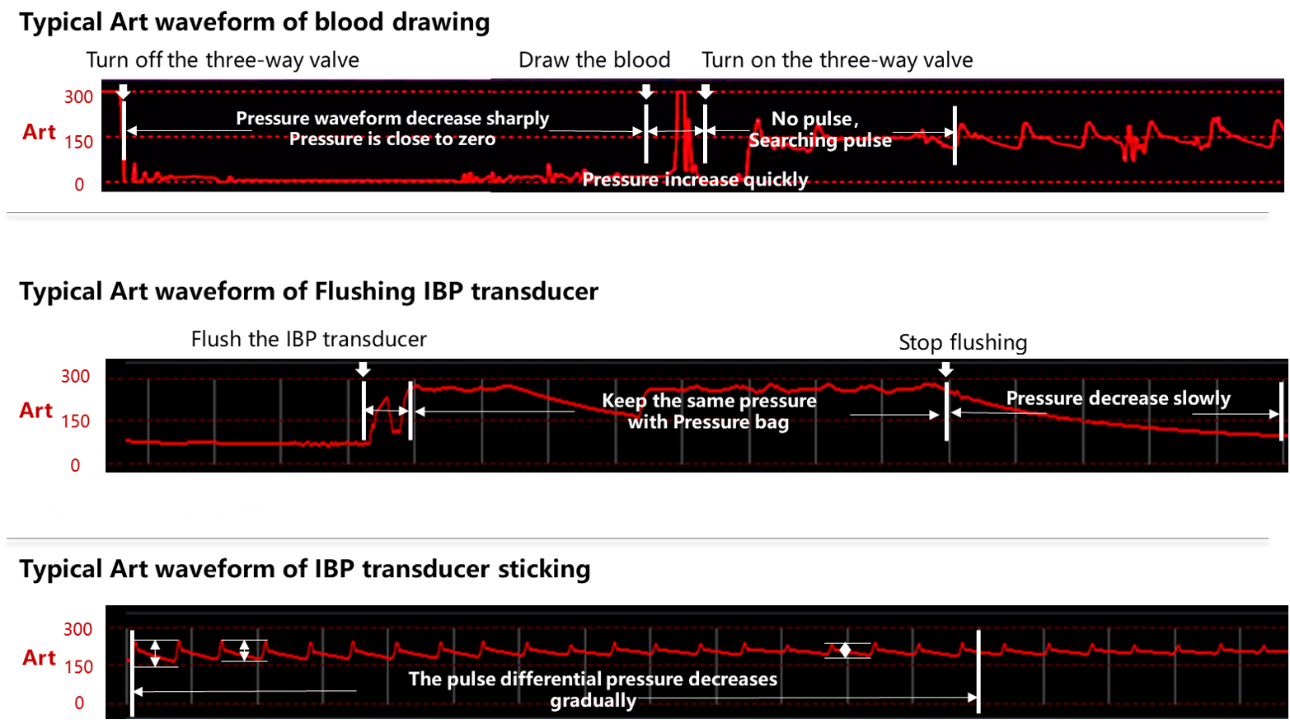
The vital signs trend table (as shown in Figure 5) shows that the patient experienced multiple dramatic spikes and drops of IBP after admission. Since IBP monitoring is easilyaffected by artificial factors, including blood drawing, tube flushing and bending, it is necessary to exclude the IBP interference and analysis patient’ s blood pressure fluctuations, after confirming that it is not caused by interference, they reviewed all the vital signs again and found that multiple over-limit IBP alarms existed in a short period of time.
Doctors checked the full disclosure wave- forms of ECG, SPO2 and IBP, confirming that the sudden deterioration IBP were real phenomenon and happened to this patient. and also the abnormal IBP fluctuations could appear even though there were no adjustment of vasoactive agent and bedside manipulation stimulation.
Based on the ultrasonographic findings (obvious attenuation of beats of the middle segment and apex of the left ventricle, i.e., a similar shape of an “octopus pot”) and negative coronary angiographic findings, the patient was diagnosed with Takotsubo syndrome. However, repeated abnormal fluctuations in IBP were observed in the patient, therefore, pheochromocytoma was also simultaneously considered.
2021-06-05
Adrenal ultrasound:
In the right adrenal gland, there was a quasi-circular area of mixed echogenicity with a size of 2.3*1.8cm, a regular margin, and enhanced echoes showing a bright light bundle with homogeneous internal echoes; a part of such area adjacent to the kidney appeared to be hyperechoic.
Adrenal CT scans:
A space-occupying lesion in the main trunk of the right adrenal gland, which was considered to be a possible adenoma.
2021-06-04 - 2021-06-06
When the patient’ s IBP fluctuated extremely, exsanguinated for testing levels of metanephrine & normetanephrine several times and results showed: metanephrine reached up to 2244.56 pg/ml (normal range: 14-90 pg/ml), and normetanephrine was up to 3021.31 pg/ml (normal range: 19-121 pg/ml).
Comprehensively considering the patient’ s proneness to impulsivity in daily life, repeated episodes of chest heaviness, an acute postoperative onset, extremely abnormal IBP fluctuations , combine with ultrasonographic manifestations, CT and ultrasound findings in the adrenal glands as well as the levels of metanephrine and normetanephrine, the patient was diagnosed with myocardial damage, heart failure and ventricular fibrillation due to large fluctuations in blood pressure caused by the release of epinephrine resulting from pheochromocytoma.
2021-06-08
At a multidisciplinary team (MDT) consultation, the current diagnosis of pheochromocytoma was confirmed, a surgical treatment plan was proposed, and preoperative preparation based on hemodynamics was made.
2021-06-15
ECMO-assisted laparoscopic right adrenalectomy was performed, after which the patient no longer experienced significant fluctuations in blood pressure. Pathologic diagnosis: The space-occupying lesion in the right adrenal gland was consistent with pheochromocytoma, and measured 2*1.5*1cm.
2021-06-16
ECMO was successfully withdrawn.
2021-06-29
The patient recovered and was discharged.
Takotsubo syndrome
Takotsubo syndrome refers to a disease in which transient left ventricular dysfunction occurs under serious mental or physical stress (including disorders). It is also known as Tako Tsubo cardiomyopathy, apical ballooning syndrome or broken heart syndrome. This disease is mainly characterized by a transient ventricular apical wall motion abnormality, and in all patients with said disease, left ventricular dysfunction is typically reversible: it usually returns to normal in a few days or weeks, and the prognosis is generally good. In the 2015 expert consensus report from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC),
it was proposed that such clinical syndrome should be uniformly named Takotsubo syndrome, and the term Takotsubo cardiomyopathy was discarded to distinguish it from other cardiomyopathy.
Takotsubo syndrome is mainly characterized by a transient ventricular apical wall motion abnormality, which resembles a balloon-like shape. It was named Takotsubo syndrome because the shape of the left ventricle resembles a Japanese octopus trap, with a round bottom and narrow neck. Approximately 90% of patients are postmenopausal women, but it can also occur in young women or men. Most patients are >65 years old at the time of onset, and less than 10% of patients are younger than 50 years old.
Takotsubo syndrome is classified into primary and secondary subtypes. Primary subtype: There is no clear trigger, or the trigger is "excitability", without underlying physical or mental impairment. Secondary subtype: At the time of visits, there is a confirmed physical or mental impairment (such as surgery, medical diseases, obstetric or psychiatric disorders), sudden activation of the sympathetic nervous system, or a sudden increase in blood catecholamine levels. So far, the pathophysiological mechanism of Takotsubo syndrome is not clear yet. It is currently believed to be mainly related to the excessive release of catecholamines (abnormal response of the hypothalamic–pituitary–adrenal (HPA) axis to stress, and a response of the sympathetic nervous system to sudden sympathetic activation). It is also believed to be possibly related to the individual's genetic susceptibility (gene polymorphisms of α1, β1 and β2 receptors or estrogen receptors).
According to Japanese and American guidelines, the diagnosis of Takotsubo syndrome requires the exclusion of pheochromocytoma. Since pheochromocytoma can cause the release of epinephrine, large fluctuations in blood pressure, and even myocardial damage, heart failure (such as the patient in this case) or sudden death in severe cases, it needs to be diagnosed based not only on clinical manifestations (mainly blood pressure fluctuations, heart lesions, and hypermetabolism caused by catecholamine secretion), but also on blood “metanephrine" level monitoring, CT or MRI, and final surgical pathology. In this case, the patient had an uncertain past history of hypertension. The level of blood "metanephrine" is also often significantly increased in clinically severe patients with Takotsubo syndrome (not caused by pheochromocytoma). Although there were imaging findings and "metanephrine" levels, continuous monitoring of blood pressure fluctuations was an important basis for the preoperative clinical diagnosis of this patient.
Influence of different operations on the shape of the blood pressure waveform
Summary
Continuous real-time monitoring and historical review of the vital signs can assist clinicians in evaluating, diagnosing and treating patients. Currently, the patients’ vital sign is the most easily obtained clinical information and also the most easily overlooked information. Because clinicians cannot view and review continuous real-time vital sign data on patients, failure to timely detect the changes in the patient's condition is tend to happen, thereby missing the best treatment opportunity, and affecting the quality of diagnosis and treatment.
Mindray’ s M-Connect IT Solution is a patient-centric, distributed monitoring solution integrating all bedside equipment data into the monitor to allow clinicians to access patient data including real-time and historical data at bedsides, nurse stations and doctor's offices in the hospital and even outside the hospital at any time, so as to adjust the diagnosis and treatment plans in time and assist in diagnosis and treatment.







