How Do Intuitive ECG Summary and Ventricular Arrhythmia Report Assist Accurate Diagnosis?
2022-10-28

In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Case introduction
A 33-year-old female patient was admitted to the hospital due to “pregnancy for 30 weeks and palpitations for 2 days”.
History of Present Illness
Two days ago, the patient experienced sudden palpitations without any apparent predisposing cause and was sent to a local hospital. An electrocardiogram (ECG) indicated sinus rhythm and frequent premature ventricular contractions. An ambulatory ECG indicated frequent premature ventricular contractions, 30,917 beats/day, and 3,202 short bursts of ventricular tachycardia. The patient immediately sought treatment at the emergency department of a tertiary A-level hospital and was admitted to the cardiovascular intensive care unit for “arrhythmia”.
Past Medical History
The patient had no history of hypertension, diabetes, surgical trauma, genetic diseases, or drug allergy based on her past physical examination.
First Physical Examination
- Body temperature: 36.4°C
- Pulse rate: 101 beats/min
- Respiratory rate: 20 breaths/min
- Blood pressure 97/66 mmHg
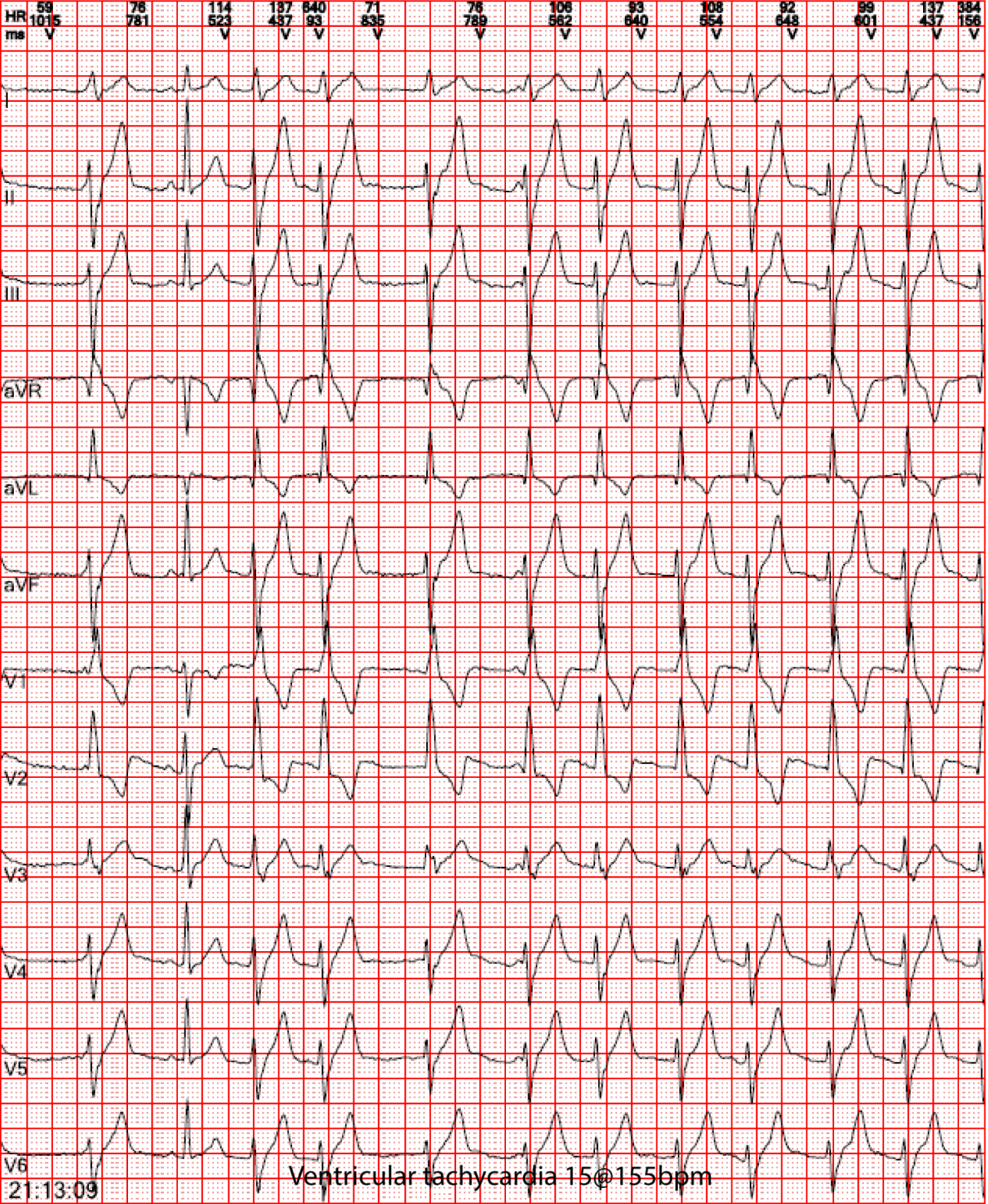
Electrocardiogram: Sinus Rhythm, left posterior fascicular ventricular tachycardia
Laboratory test: Biochemistry test: K+ 3.67 mmol/L, Mg2+ 0.82 mmol/L, P5+ 0.76 mmol/L
Preliminary Diagnosis: Arrhythmia
Conditions after admission are as follows
After admission
5-lead ECG monitoring, SpO , and NIBP 2 monitoring were performed, and relevant examinations were completed. The doctor ordered a Holter monitoring, and oral potassium supplementation was performed to adjust electrolyte levels. The Department of Obstetrics and Gynecology was consulted to assess the condition of the fetus, and the relevant examinations were performed. (Under normal circumstances, it takes 48 hours to obtain the Holter monitoring results on the first day. During this period, doctors can only judge and provide treatment regimens based on the patient’s resting ECG results, biochemical indicators, and clinical manifestations.)
After Admission for 1 hour and 22 minutes
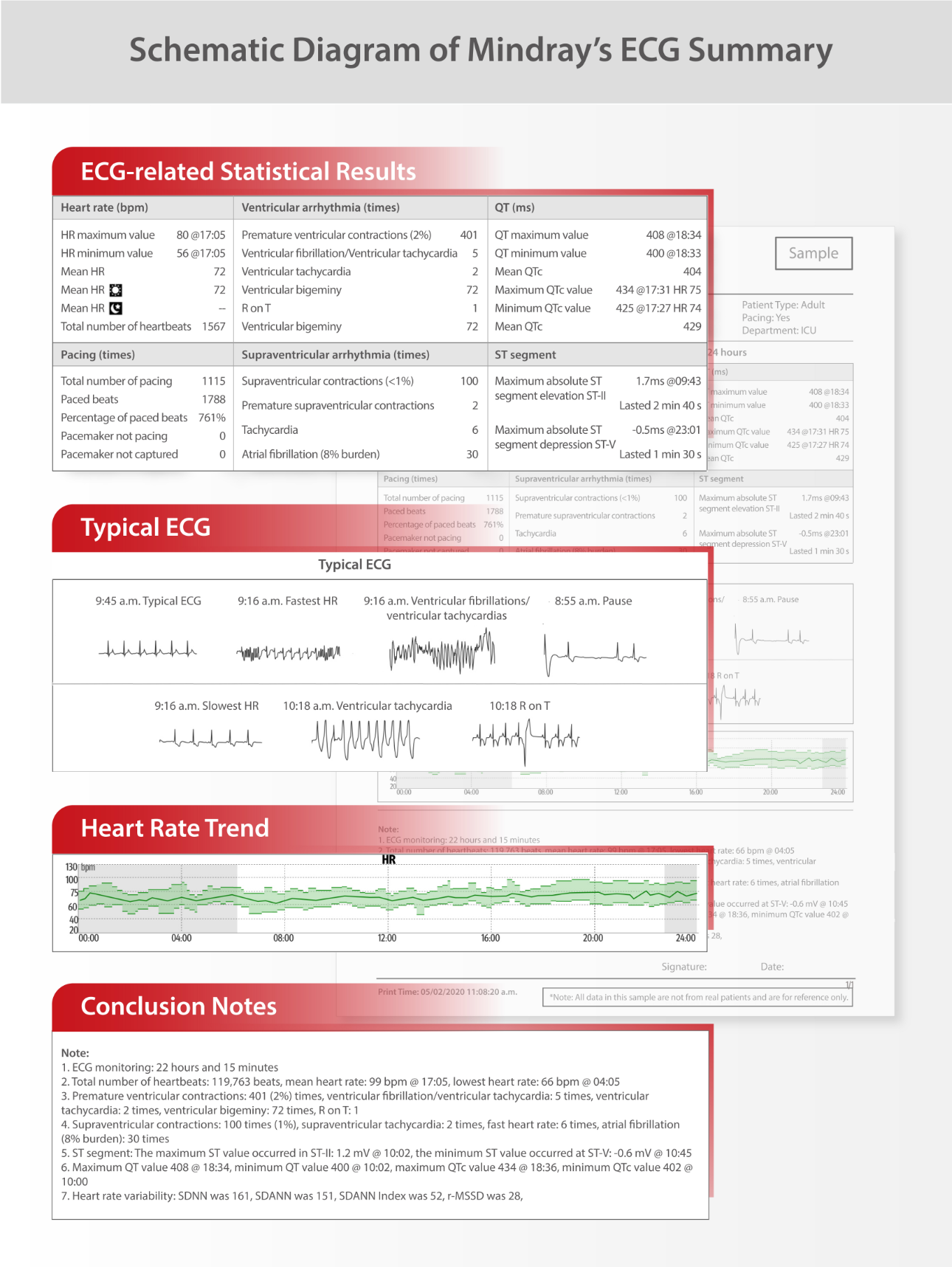
The doctor viewed the patient’s ECG monitoring through the newly released ECG Summary function on Mindray CentralStation, and obtain the following results:
- The total number of heartbeats was 6,454, including 1,807 premature ventricular contractions, accounting for 28%
- 193 short bursts of ventricular tachycardia.
Compared with the primary Holter results, the frequency of occurrence of premature ventricular contractions and short-burst ventricular tachycardia was similar, with no significant increase or decrease, and the patient’s arrhythmia did not aggravate or mitigate.
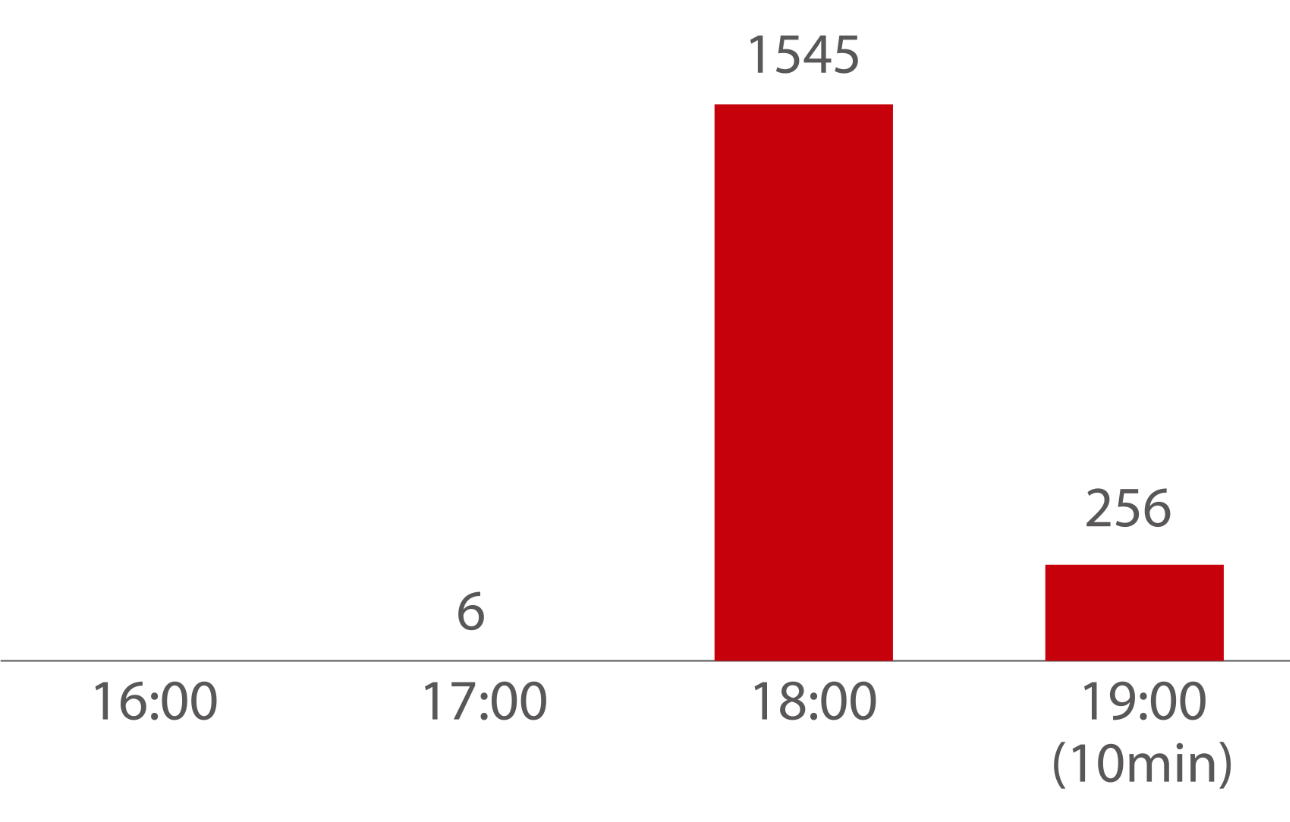
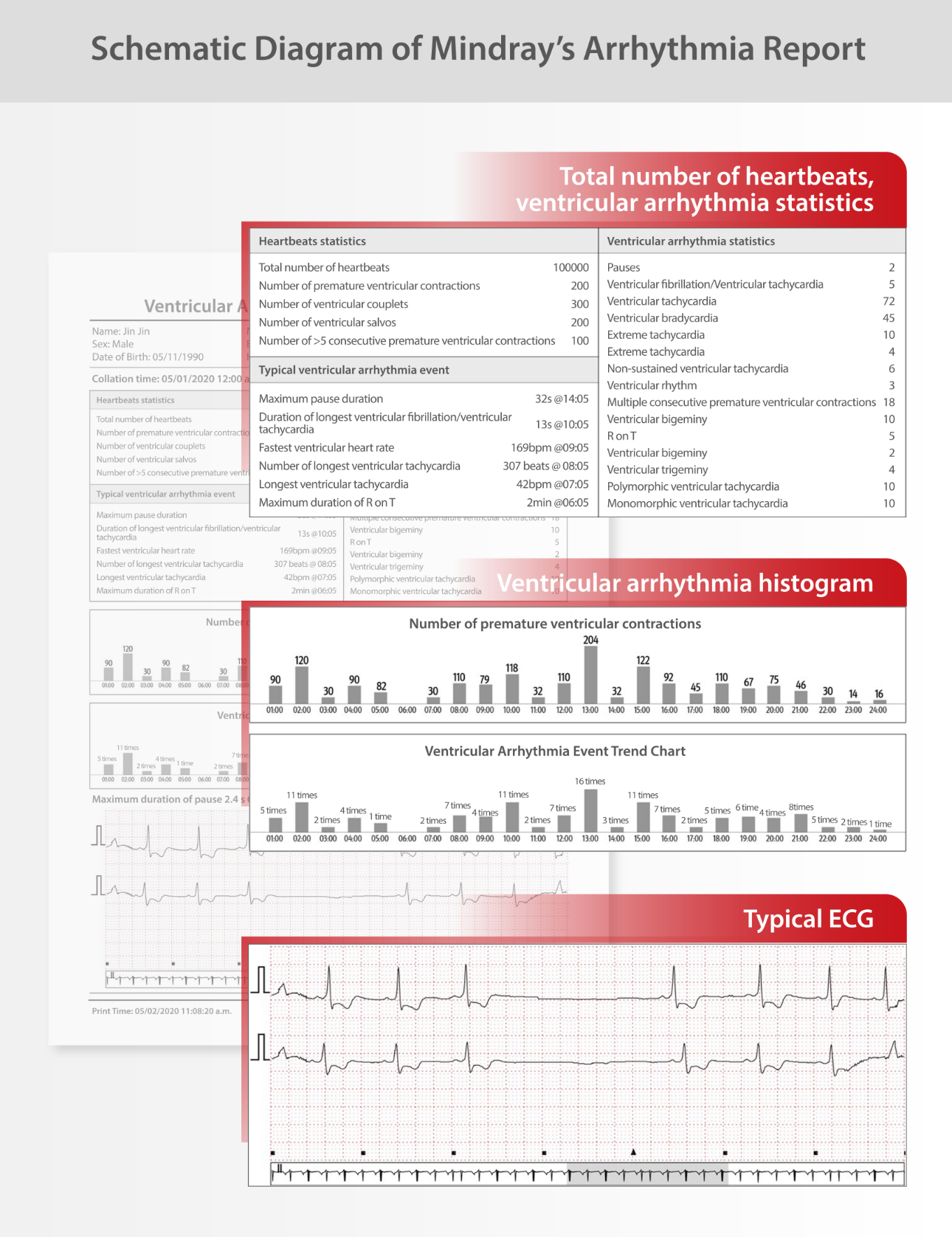
The histogram of the ventricular arrhythmia report is shown as follows:
Day 1 of admission
A retest of electrolyte levels showed: K+ 4.16 mmol/L, Na+ 138.7 mmol/L, Cl 106.8 mmol/L, Ca2+ 2.19 mmol/L.
At the same time, the patient’s Day 1 ECG Summary was tracked on the ViewStation in the doctor’s office. The total number of heartbeats was 128,418, including 13,300 premature ventricular contractions, accounting for 10%, and 265 short bursts of ventricular tachycardia. Potassium supplementation was effective, the patient’s condition improved, and the current treatment remained unchanged.
Day 2 of admission
A retest of electrolyte levels showed: K+ 4.24 mmol/L, Na+ 135.5 mmol/L, Cl 103.4 mmol/L, Ca2+ 2.27 mmol/L. The patient’s Day 2 ECG Summary continued to be viewed on the Mindray ViewStation. The total number of heartbeats was 138,622, including 13,157 premature ventricular contractions, accounting for 9%, and 237 short bursts of ventricular tachycardia. The patient’s condition continued to improve. The treatment remained unchanged, and observation was continued.
Day 3 of admission
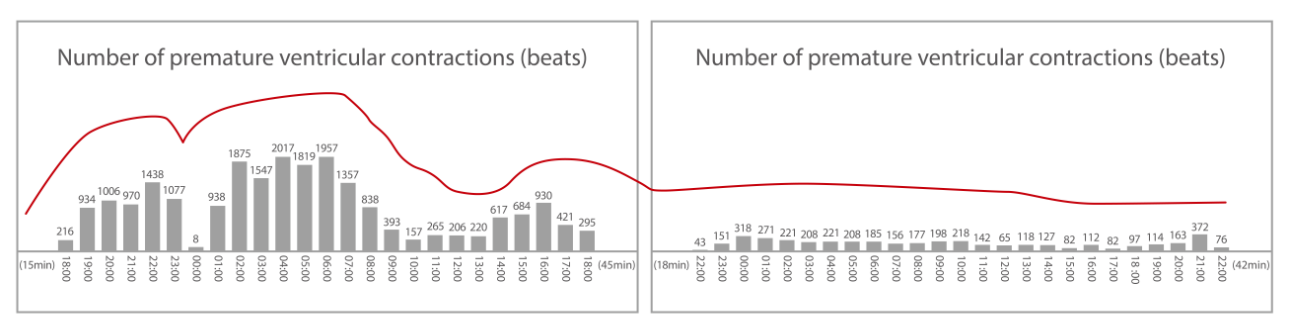
During the morning ward round, the doctor found that the patient’s number of ventricular arrhythmias increased again through the histogram of the ventricular arrhythmia report. A retest of electrolyte levels found that K+ was
3.93 mmol/L, which was lower than the previous day. The rate of potassium supplementation was increased again. After the potassium supplementation rate was increased from 8:00 a.m. to 9:00 a.m. in the morning, the proportion of ventricular beats began to decrease significantly, which proved that the frequency of premature ventricular contractions was strongly correlated with the potassium concentration in the patient’s blood.
The histogram of the number of premature ventricular contractions is shown in the figure.
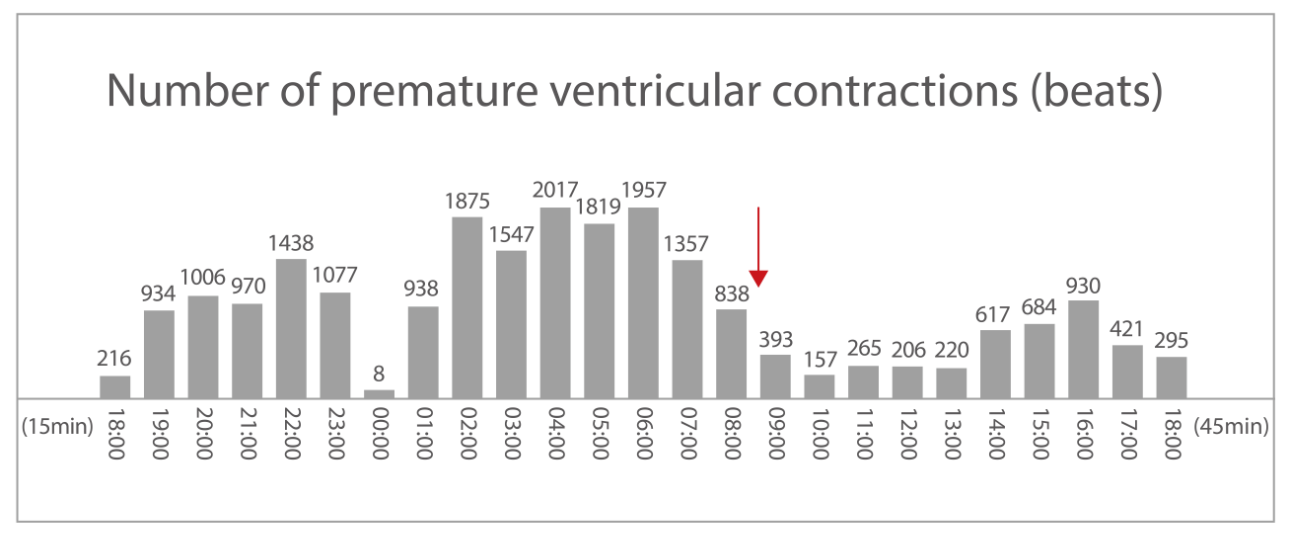
A review of the patient’s Day 3 ECG Summary showed that the total number of heartbeats was 135,816, including 22,185 premature ventricular contractions, accounting for 16%, and 1,777 short bursts of ventricular tachycardia.
On the same day, the patient’s 24-hour Holter result on Day 1 came out, with a total of 132,715 heartbeats, a total of 13,577 premature ventricular contractions, and a total of 317 bursts of ventricular tachycardia, which were close to the ECG Summary results on Day 1 [the 24-hour start and end time of the analysis was slightly different]. The ECG Summary of the Mindray monitor was consistent with the Holter result.
The patient had left posterior fascicular ventricular tachycardia, also known as verapamil-sensitive reentrant ventricular tachycardia, and the onset of ventricular tachycardia was correlated with serum potassium level. From the multi-day ECG Summary and ventricular arrhythmia report of the monitor, it can be found that potassium supplementation treatment is effective, and the patient’s condition is stable. After weighing the risks of using verapamil, the doctor and the patient agreed to not use verapamil for the time being.
Day 4 of admission
A retest of electrolyte levels by the doctor revealed: K+ 4.11 mmol/L.
A review of the patient’s Day 4 ECG Summary showed that the total number of heartbeats was 130,675, including 4,150 premature ventricular contractions, accounting for 3%, and 98 short bursts of ventricular tachycardia.
The histogram of the ventricular arrhythmia report is shown in the figure:
Subsequently, the patient’s blood potassium level was stable, and the patient had occasional premature ventricular contractions and no short bursts of ventricular tachycardia. The patient was transferred to the Department of Cardiology for continued treatment, and then the patient was discharged from the hospital after she recovered.
Analysis
The pregnant patient was diagnosed with left posterior fascicular ventricular tachycardia by ECG, and hypokalemia was the predisposing factor for ventricular tachycardia. For such patients, the improvement of ventricular arrhythmia needs to be evaluated in combination with blood potassium levels. So, does more treatment (such as verapamil therapy or radiofrequency ablation) need to be administered while correcting hypokalemia? This answer requires more and more timely vital sign information support to assist doctors in making decisions.
The low-frequency resting ECG summary cannot reflect the arrhythmia changes throughout the day. The output of the Holter results is delayed for 48 hours, which cannot assist the medical staff in timely control of the patient’s current ventricular arrhythmia or improve the progression during hospitalization, affecting the medical staff’s judgment of patients' condition and current treatment efficacy.
Mindray BeneVision Patient Monitoring System, based on big data and intelligent algorithms, calculates the past abnormal changes of patients, automatically captures typical abnormalities, and generates long-term status summary (including ECG Summary, ventricular arrhythmia Summary, atrial fibrillation Summary, etc., as shown below), which is easy to obtain, intuitive, continuous and complete, allowing doctors and nurses to clearly and comprehensively assess the context of patient status changes, and improve the efficiency and quality of diagnosis and treatment.
Appendix
Left posterior fascicular ventricular tachycardia[1]
The most common idiopathic left ventricular tachycardia (ILVT) is verapamil-sensitive reentrant ventricular tachycardia. It originates in the left posterior fascicle. Its electrocardiographic manifestations are Right Bundle Branch Block (RBBB) and left inferior axis deviation. Therefore, it is also known as verapamil-sensitive ventricular tachycardia and fascicular ventricular tachycardia. In 1979, Zipes et al. first described the electrocardiographic features of this ventricular tachycardia and proposed the preliminary diagnostic criteria, namely, atrial stimulation-induced, RBBB+ left axis deviation, and no basis for structural heart disease. In 1981, Belhassen et al. first confirmed that this type of ventricular tachycardia was sensitive to verapamil.
Pharmacotherapy
The efficacy of verapamil on ILVT is well known. Intravenous verapamil is preferred when ventricular tachycardia occurs. Intravenous diltiazem can also be used. Intravenous verapamil may not terminate ILVT if the ventricular tachycardia has persisted for a long time and a large number of catecholamine products have been produced, and intravenous amiodarone or sotalol can be used at this time.
For long-term pharmacological prophylaxis of ILVT, oral verapamil can effectively prevent or reduce the occurrence of tachycardia. Class III antiarrhythmics, amiodarone, and sotalol, can also be used to prevent the onset of ILVT.
Radiofrequency ablation therapy
Hemodynamic changes at the time of ILVT onset, recurrent persistent ILVT, and patients with ILVT who cannot tolerate pharmacotherapy or failed to respond to pharmacotherapy can be treated with catheter ablation for radical treatment. The long-term results and complications of ILVT ablation are basically similar to those of RVOT-VT, but its success rate is slightly lower, ranging from 80% to 90%.
References
[1] Zhu Li, Cao Kejiang. Idiopathic ventricular tachycardia [J]. Chinese Journal of Cardiac Arrhythmias, 2002, 6(1):8.







