D-dimer in COVID-19
As COVID-19 continues to swipe around the world, rapid diagnosis as well as prognosis and treatment of the COVID-19 patients has become an equally important topic among clinicians. Recently scientists have discovered that COVID-19 has a host cell receptor, Angiotensin Converting Enzyme II[1] or ACE2. With the help of ACE2, COVID-19 invades the human body rapidly by reproducing on its own at a massive rate, destroying normal cell, tissue and microvascular system, finally causing acute lung injury, multiple organ failure[2-4], and intravascular coagulation which occurs in 71.4% of patients who died from COVID-19[5]. It is widely known that D-dimer is a significant bio-marker which correlates with hypercoagulability. More clinical studies have also revealed the relationship between D-dimer and COVID-19.
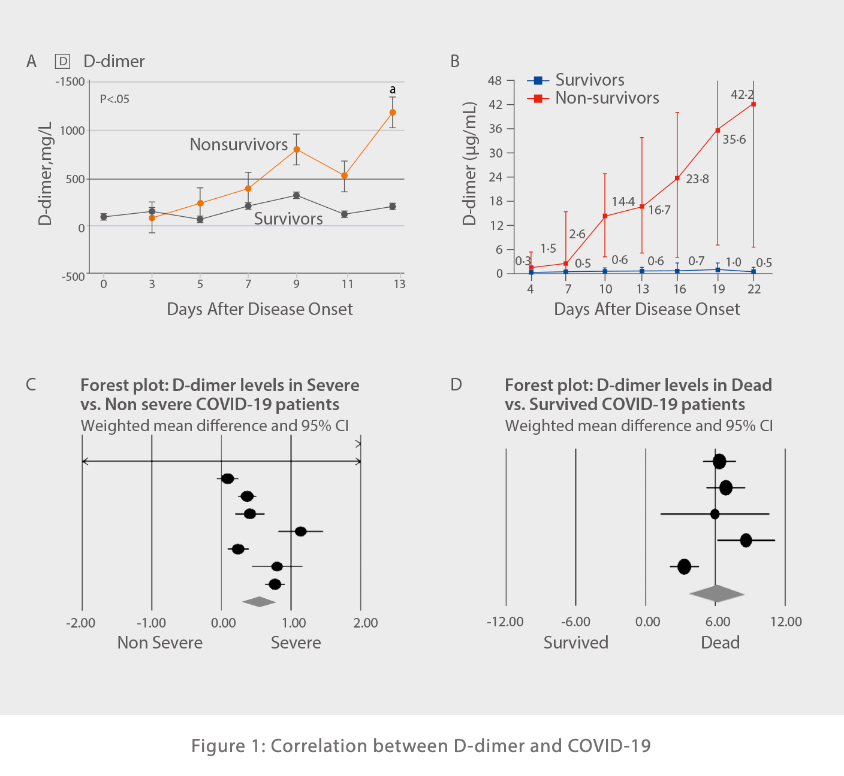
As published on Jama by Zhi Yong’s Group, in the patients’ death(non-survivor) group of novel coronavirus pneumonia, the D-dimer level initially increased as the disease developed, until the 7th day when the D-dimer level broke through the normal range, and finally plateaued at a high level [Figure 1 A][6]. In comparison, the survivor group remained within the normal range consistently. Another article published in the Lancet also claims that there is a close correlation between the D-dimer level and the mortality rate of victims [Figure 1 B][7]. The same conclusion was also drawn in Shah’ s research, which utilized a systematic meta-analysis method (including results from 18 articles and a total of 3,682 patients) to draw the forest plots [Figure 1 C, D][8]. To sum up, whether in severe or dead COVID-19 patients, the D-dimer level was higher than that which was found in non-severe or surviving patients.
Application of D-dimer in COVID-19 Prognosis
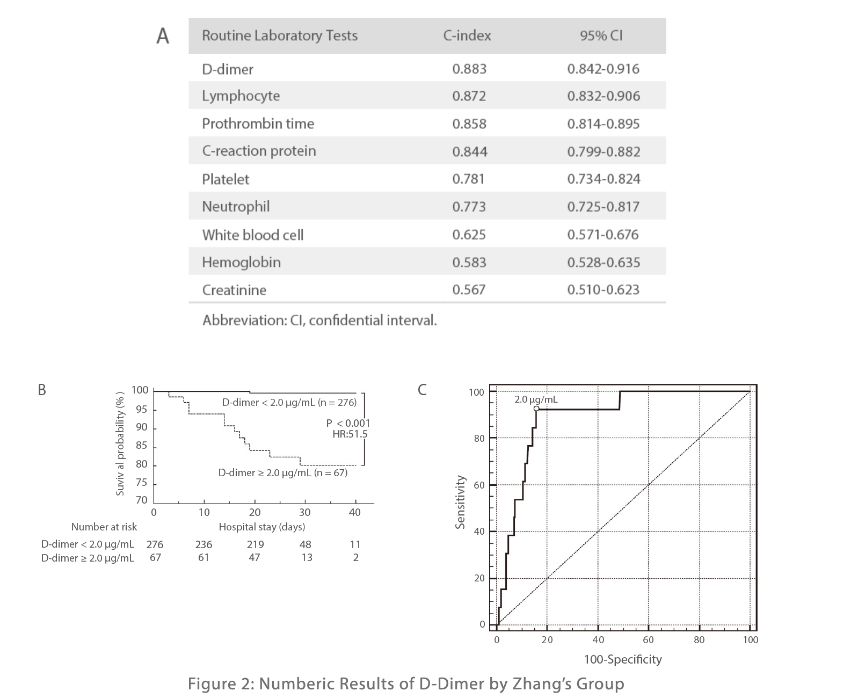
According to the study by Zhang’s group, D-dimer among all parameters tested in patients with COVID-19 had the highest C-index, which indicates that it has the highest prediction coincidence rate in routine lab testing methods [Figure 3 A]. In addition, they also found the 2 μg/ml of D-dimer could be the cut-off value of mortality risk of COVID-19, as DD > 2 μg/ml the survival probability will decrease dramatically [Figure 2 B]. Consequently, they based the evaluation of this value and manifested that when 2 μg/ml was set as the cut-off value, 92.3% of sensitivity and 83.3% of specificity is the optimum in all groups [Figure 2 C][9].
There has been evidence regarding an increased incidence of venous thromboembolic events (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE), in patients with severe COVID-19 infection[9], and D-dimer can also be used as a monitoring indicator of VTE and PE with a cut-off value of 0.55 μg/ml. Furthermore, Yao not only found that patients with over 2 μg/ml D-dimer needed intensive care and early intervention, but suggested a cut-off value of 1 μg/ml could help doctors identify patients with a poor prognosis [10].
In conclusion, D-dimer has enormous clinical values in the treatment and prognosis of COVID-19 as a sensitive monitoring index. In consideration of disordered coagulation micro-environment in patients infected with COVID-19 or at high risk of VTE induced by reduced activity, increased bed time, or in people being quarantined for hospitalization, testing of D-dimer on a regular basis is necessary for rapid monitoring of disease treatment. While a cut-off value of over 2 ug/ml has been proved by many researchers monitoring patients’ treatment, laboratories are still advised to set their own standard so the variation in demographics can be taken into account.
Mindray’s Coagulation D-dimer Solution
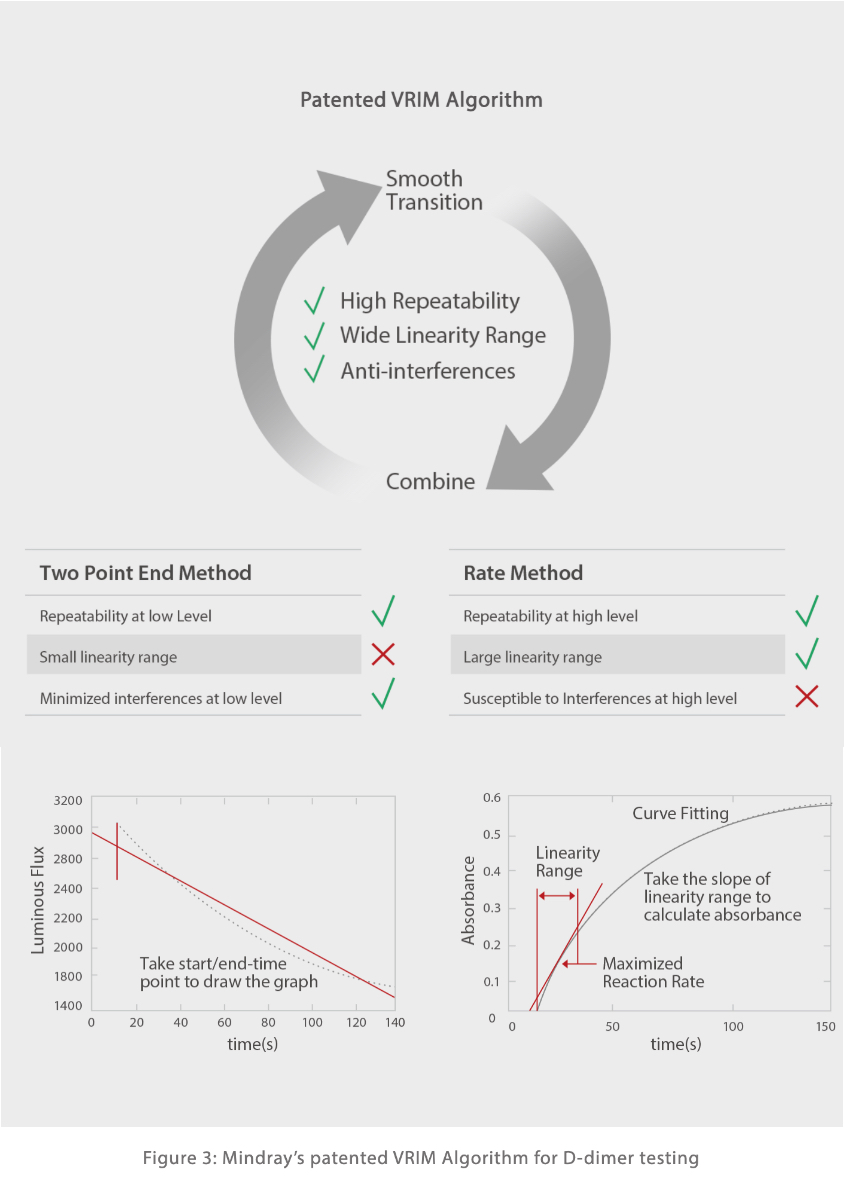
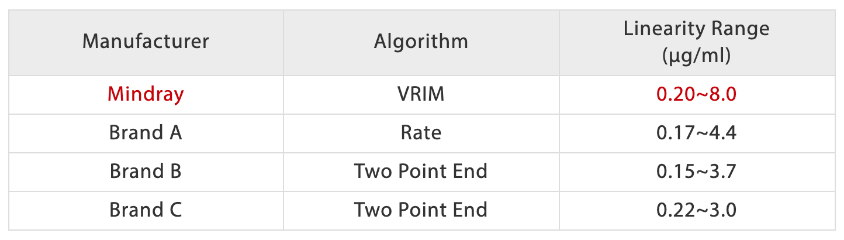
Mindray’s auto-coagulation analyzers C3100 & C3510 are equipped with both classic mechanical and optical detection mechanisms. The mechanical methodology is insensitive to interference from icteric, lipemic, chylus and hemolytic samples. Moreover, the patented VRIM(VLin-Rate Integrative Method) algorithm has also been developed to combine “Two Point End Method” at a low D-dimer concentration together with “Rate Method” at a higher level [Figure 3]. This has enabled a much wider linearity range of D-dimer results compared with other models on the market [Figure 4].
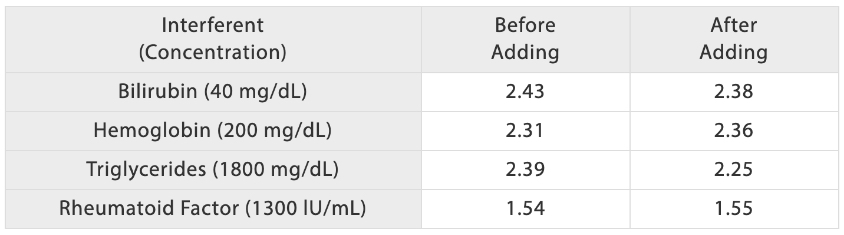
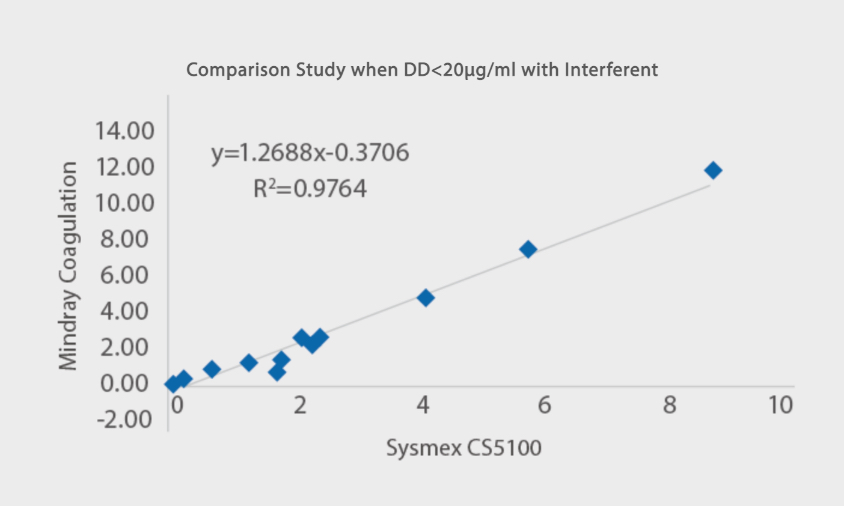
In addition, Mindray’ s coagulation solution to D-dimer testing is less susceptible to common interferents. As is shown in [Figure 5], when the serum samples are added with bilirubin, hemoglobin, triglycerides and rheumatoid factors at respective concentration, D-dimer results remain at constant levels as before. The Comparison study with Sysmex CS5100 has also shown a good correlation with R2> 97% with interferents added.
Mindray’ s D-dimer coagulation reagents are all manufactured in a bottled liquid state which are ready to use [Figure 6], while the majority of coagulation testing kits are made into powder. Simply by opening the cap and loading D-dimer reagents onto the analyzer, preparation can be set up rapidly with ease on Mindray’s coagulation analyzers.

References:
[1] Behl T., Kaur I., Bungau S., Kumar A., Uddin M. S., Kumar C., et al. (2020). The dual impact of ACE2 in COVID-19 and ironical actions in geriatrics and pediatrics with possible therapeutic solutions. Life Sci. 257, 118075. 10.1016/j.lfs.2020.118075.
[2] Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020.
[3] Chousterman BG, Swirski FK, Weber GF. Cytokine storm and sepsis disease pathogenesis. Semin Immunopathol. 2017;39(5):517–28.
[4] Ding YQ, Bian XW. Analysis of coronavirus disease-19 (covid-19). Chin J Pathol. 2020;49(00):E003.
[5] Tang N., Li D., Wang X., Sun Z. (2020. b). Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 18, 844–847. 10.1111/jth.14768
[6] Dawei Wang, Bo Hu ,et al. Clinical Characteristics of 138 hospitalized patients with 2019 novel Coronavirus-Infected Pneumonia in Wuhan,China[J]. JAMA. 2020.
[7] Fei Zhou., MD,a., Ting Yu., MD,b. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 28 March-3 April; 395(10229): 1054–1062.
[8] Shah Siddharth., Shah Kuldeep., Patel Siddharth B., Patel Foram S., Osman Mohammed., Velagapudi Poonam., Turagam Mohit K., Lakkireddy Dhanunjaya., Garg Jalaj.(2020). Elevated D-Dimer Levels Are Associated With Increased Risk of Mortality in Coronavirus Disease 2019: A Systematic Review and Meta-Analysis. Cardiol Rev, 28(6), 295-302. doi:10.1097/CRD.0000000000000330
[9] Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38.
[10] Simadibrata Daniel Martin., Lubis Anna Mira.(2020). D-dimer levels on admission and all-cause mortality risk in COVID-19 patients: a meta-analysis. Epidemiol Infect, 148(undefined), e202. doi:10.1017/S0950268820002022