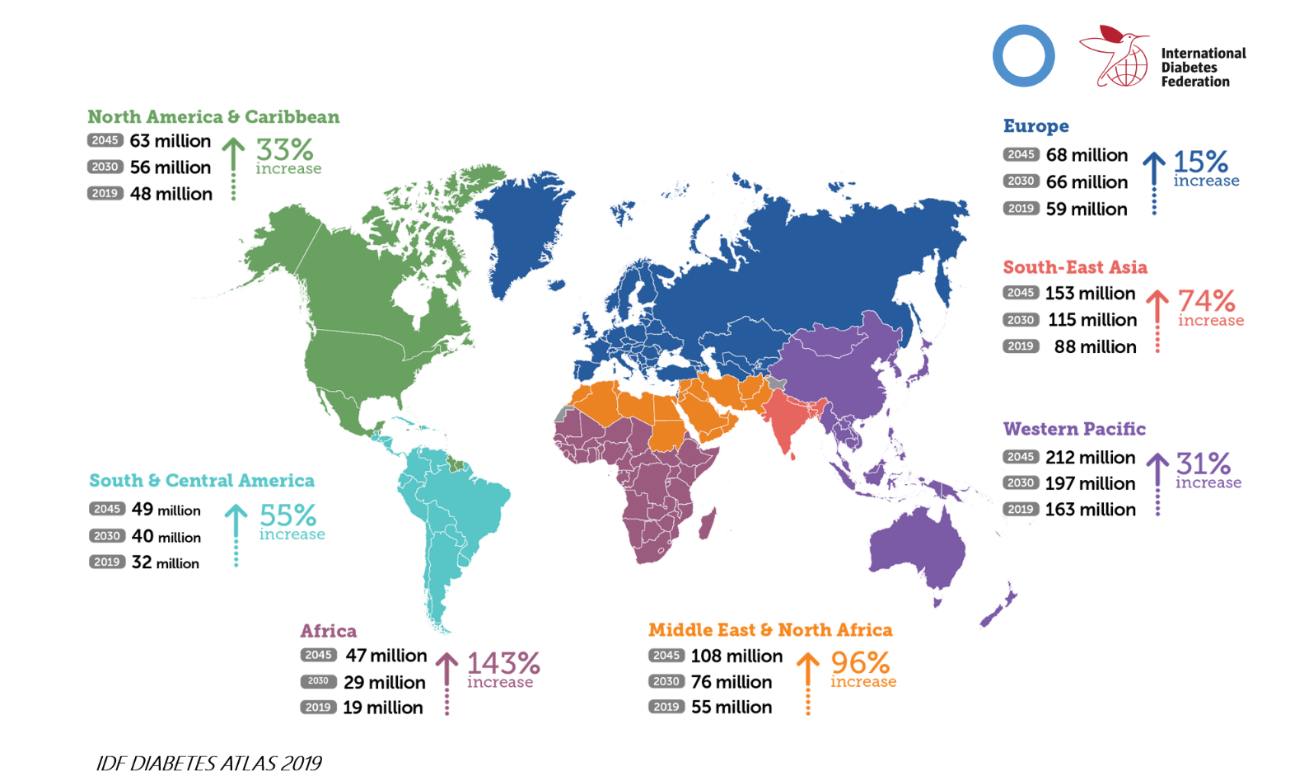
Diabetes Mellitus (DM) is a global health challenge. One in 11 adults (20-79 years) were reported to have DM by the International Diabetes Federation (IDF) in 2019, and this proportion is on the rise as society changes and the population ages.[1] DM complications include a series of problems, such as nephropathy, retinopathy, and coronary artery disease.
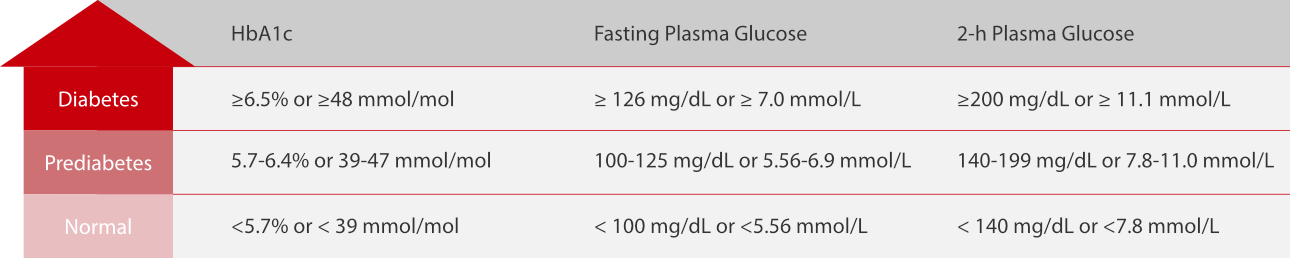
Diagnosis, proper treatment, and glycemic control monitoring are essential to DM management. As a result, many laboratory tests have been introduced in practice, such as glycated hemoglobin (HbA1c), glycated protein (fructosamine, FUN), fasting plasma glucose, and 2-hour plasma glucose. Among them, HbA1c is widely recognized as a core test for DM management.
DM Diagnosis
According to the IDF, there are approximately 232 million people with undiagnosed DM worldwide. Many guidelines tend to suggest DM screening in the population with or without specific medical conditions, and HbA1c is a convenient test to meet this objective.[2] Unlike glucose tests, HbA1c is not affected by recent food intake, so patients do not have to fast or intake certain quantities of glucose before the test. Accompanied with medical history and some auxiliary evidence, doctors can make the DM diagnosis if the patient’s HbA1c matches the criteria.
Therapeutic Monitoring
Once diagnosed, patients may receive treatment, such as lifestyle changes, medication, and/or insulin. Regardless of the treatment method, monitoring is crucial to holistically manage this disease. As HbA1c can reveal the average blood glucose over an approximate 3-month period, many guidelines have published HbA1c targets for glycemic control monitoring. These targets can be used to guide therapeutic improvements.
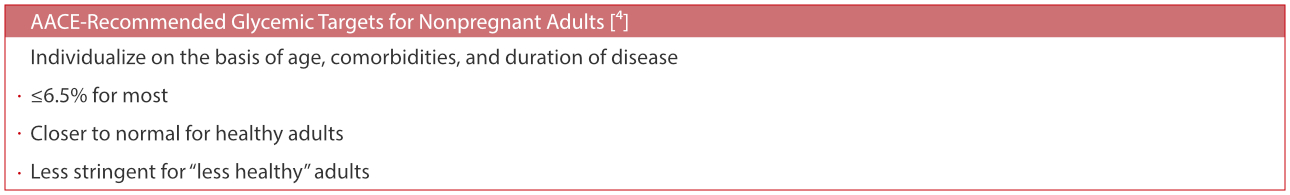
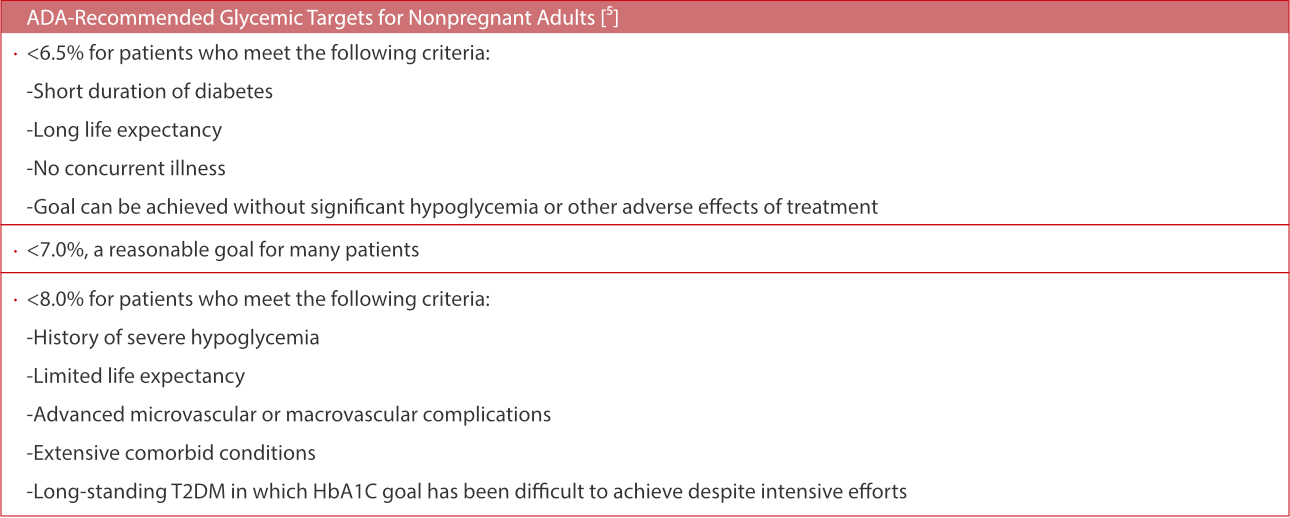
HbA1c is an ideal marker for the assessment of glycemic control. Every small reduction in HbA1c can significantly reduce the risks of DM-related morbidity and mortality. The test frequencies are every 6 months for well-controlled patients, and every 3 months for poorly-controlled patients, or patients who are making changes to their therapeutic regimen.[6]

Summary
Since HbA1c was first separated in 1958, a series of studies have proved it to be highly valuable in the diagnosis and monitoring of DM. As a core marker recommended by multiple guidelines, HbA1c tests are much easier for patients to complete, much faster for laboratory technicians to analyze, and much more reliable for doctors to use to make clinical decisions.
References
[1] IDF DIABETES ATLAS 2019. https://www.diabetesatlas.org/en/
[2] Pippitt, K. & Li, M. Diabetes Mellitus: Screening and Diagnosis. Diabetes Mellitus 93, 7 (2016).
[3] American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020. Diabetes
Care 43, S14 (2020).
[4] Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and
American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2017 executive summary.
Endocr Pract 2017; 23(1): 207-38.
[5] American Diabetes Association. Glycemic Targets: Standards of Medical Care in Diabetes—2020. Dia Care 43, S66–S76 (2020).
[6] HbA1c Testing Frequency: A Review of the Clinical Evidence and Guidelines [Internet]. Ottawa (ON): Canadian Agency for Drugs
and Technologies in Health; 2014 Sep 26.
[7] United Kingdom Prospective Diabetes Study Group: Intensive blood-glucose control with sulphonylureas or insulin compared
with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352: 837–853, 1998
[8] Stratton IM, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35):
prospective observational study. BMJ 321:405–412, 2000