In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Case Introduction
The patient is an 83-year-old male who complained of cough and asthenia for more than 20 days, which was aggravated and accompanied by drowsiness for one week. The patient had a medical history of chronic gastritis for 20 years, and did not undergo systemic treatment; had a medical history of hypertension for more than 8 years; had a medical history of lacunar infarction for 4 years, and did not undergo special treatment. He was admitted to the ICU on January 22, 2021.
Physical Examination at Admission
Physical examination at admission of the patient showed pulse rate 116 beats/minute, respiratory rate 30 breaths/minute, blood pressure 160/84 mmHg, and SpO2 93%. The patient was alert, with tachypnoea, on continuous ventilator-assisted breathing (SIMV mode); both pupils were equal and round in size, with a diameter of about 2 mm, reactive to light; supple neck, resonant sounds were heard in both lungs on percussion test, coarse breath sounds in both lungs, low breath sounds in the right lower lung, and moist rales in both lower lungs; no enlargement of the heart boundary on percussion, and regular heart rhythm. Muscle strength of four limbs was grade 4, and no significant edema was found in both lower limbs. CT of the head, chest and abdomen found that the patient had partial intracranial arteriosclerosis, multiple infections in both lungs, and a small amount of pleural effusion on both sides. Blood gas results showed low pO2 and decreased pH.
According to the medical history and examination, the patient was diagnosed with severe pneumonia, coronary heart disease, acute left heart failure and grade 3 hypertension.
Lung Infection Condition
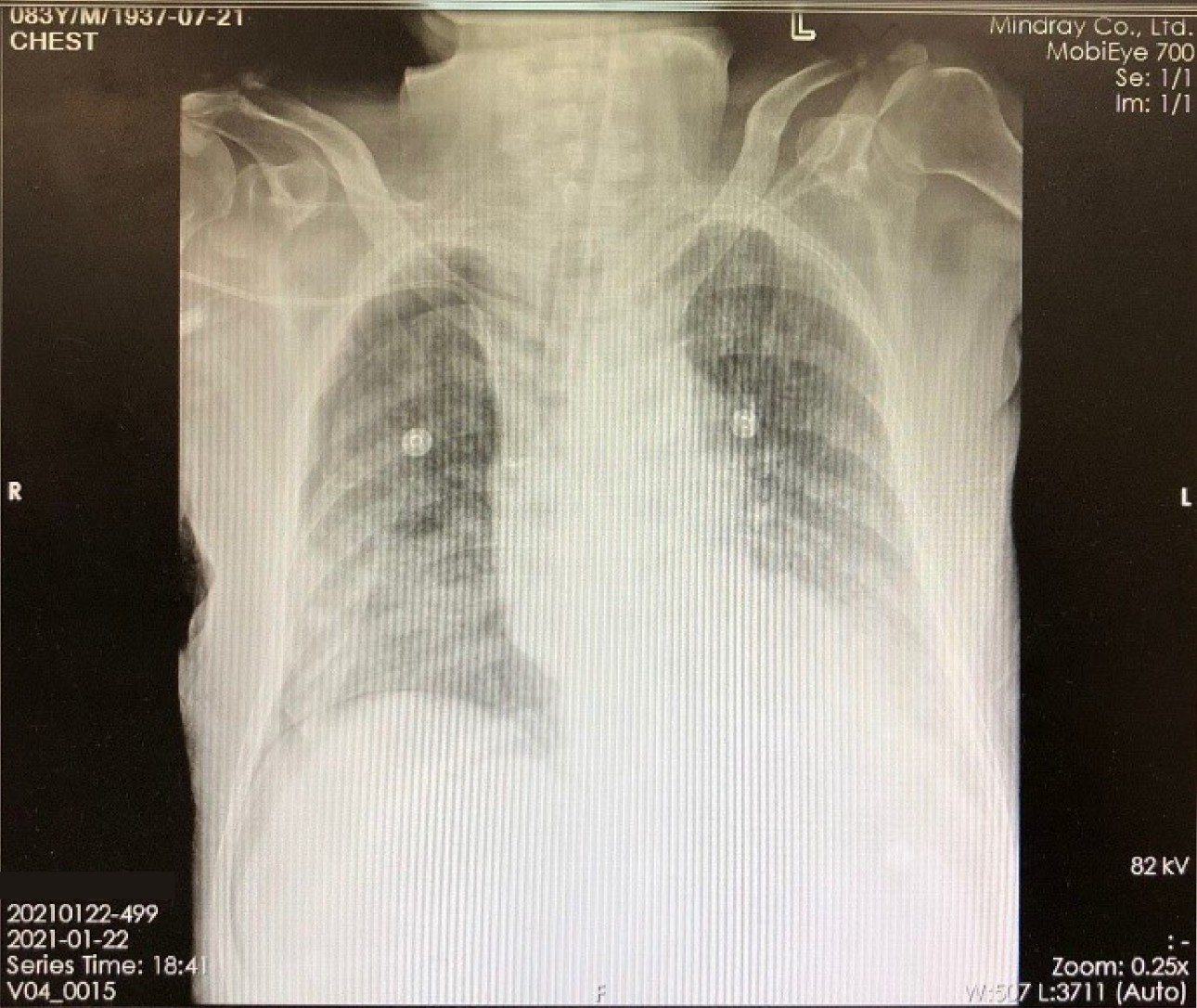
X-ray image (Figure 1) on January 22, 2021 showed about 30% compressing of the right lung, with multiple infections in both lungs. The CT examination results on January 25 also showed that the patient had infections in both lungs and a small amount of pleural effusion on the left side. On the same day, the aerobic culture + smear microscopy results of the lower respiratory tract specimen indicated the presence of Gram-negative bacilli and Gram-positive bacilli infections, and the results showed a large amount (>30/OIF).
Disease Progression
At 01:49 a.m. on January 28, 2021, the patient’s condition suddenly aggravated and blood pressure dropped rapidly from 138/55 mmHg (MAP 92 mmHg) to 95/39 mmHg (MAP 65 mmHg). According to the baseline of the patient’s physiological parameters, the systolic pressure alarm limit of the bedside monitor was set to 90 mmHg, and the lowered blood pressure did not trigger the one-parameter threshold alarm.
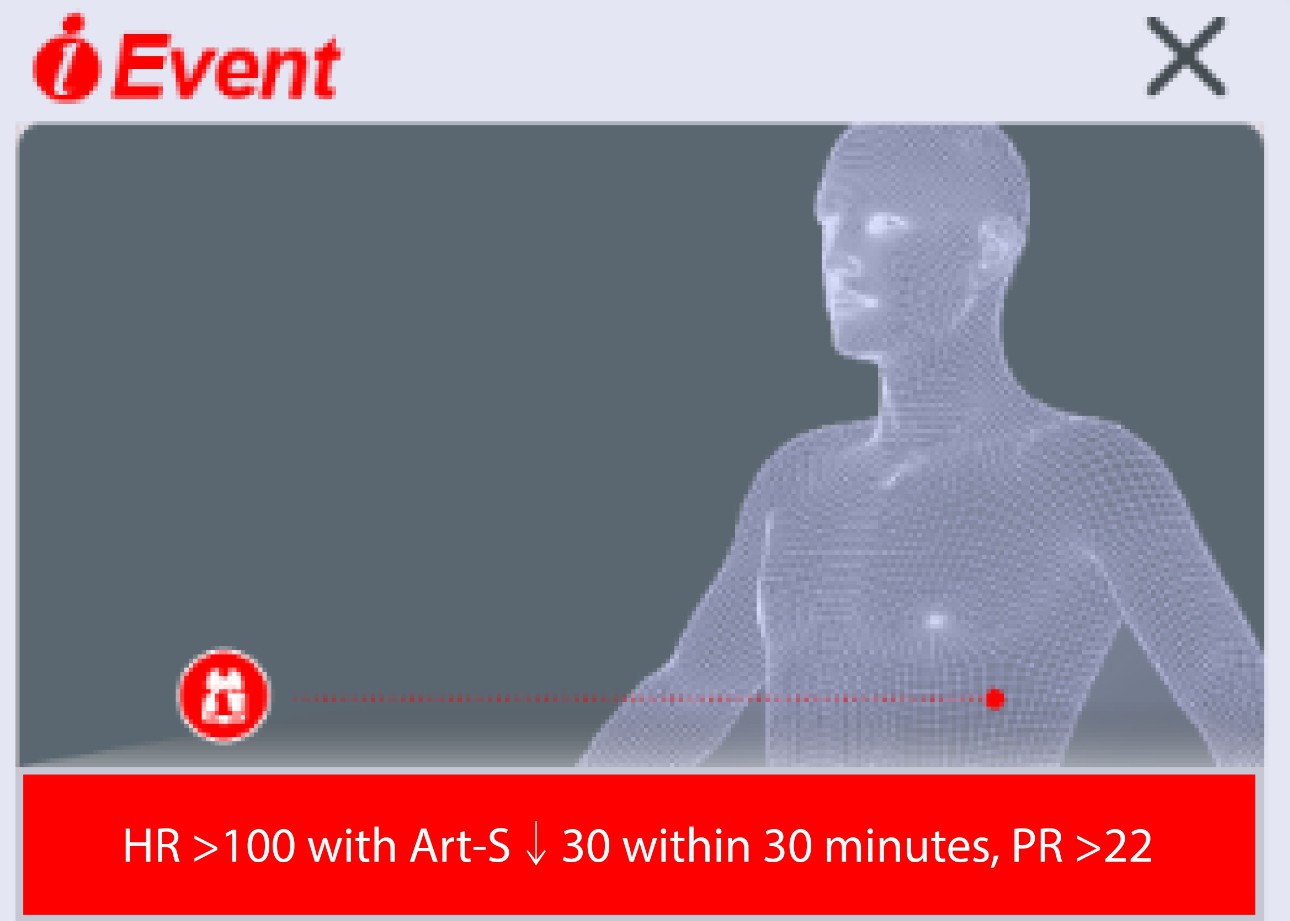
The Mindray monitor recognized the trend of sudden change in blood pressure of the patient through intelligent analysis in the backend. Through the prompt message showing “HR >100, with Art-S↓30 within 30 minutes, RR >22”, the monitor alerted medical staff to the exacerbation of the patient’s hemodynamic status, which might cause shock. At the same time, the unique patient status guide interface on the Mindray monitor (see the figure below) visually communicated this information to the clinical staff in the form of images. After seeing and confirming the accuracy of the alarm, the nurse called the physician immediately.
The physician subsequently performed several emergency tests on the patient, including liver function + renal function + cardiac enzyme + E4A + serum electrolyte test, white blood cell classification + routine blood test, and blood gas analysis.
The main results were as follows: White blood cell count 20.3 ×109/L ↑;
Differential neutrophil count 18.4 × 109/L ↑; Neutrophil percentage 90.8% ↑;
pH 6.89 ↓;
pO2 13.0 mmHg ↓;
pCO2 63.0 mmHg ↑;
Lac 5.5 mmol/L ↑.
Based on the results of multiple emergency tests, the physician gave the diagnosis of septic shock with multiple organ failure. Subsequently, norepinephrine was immediately given via intravenous injection at a concentration of 0.12 mg/mL, 6 mg in total; esmolol was injected at the same time at a concentration of 0.01 g/mL, 0.5 g in total. The patient’s systolic pressure was briefly increased to 120 mmHg and then decreased to about 95 mmHg.
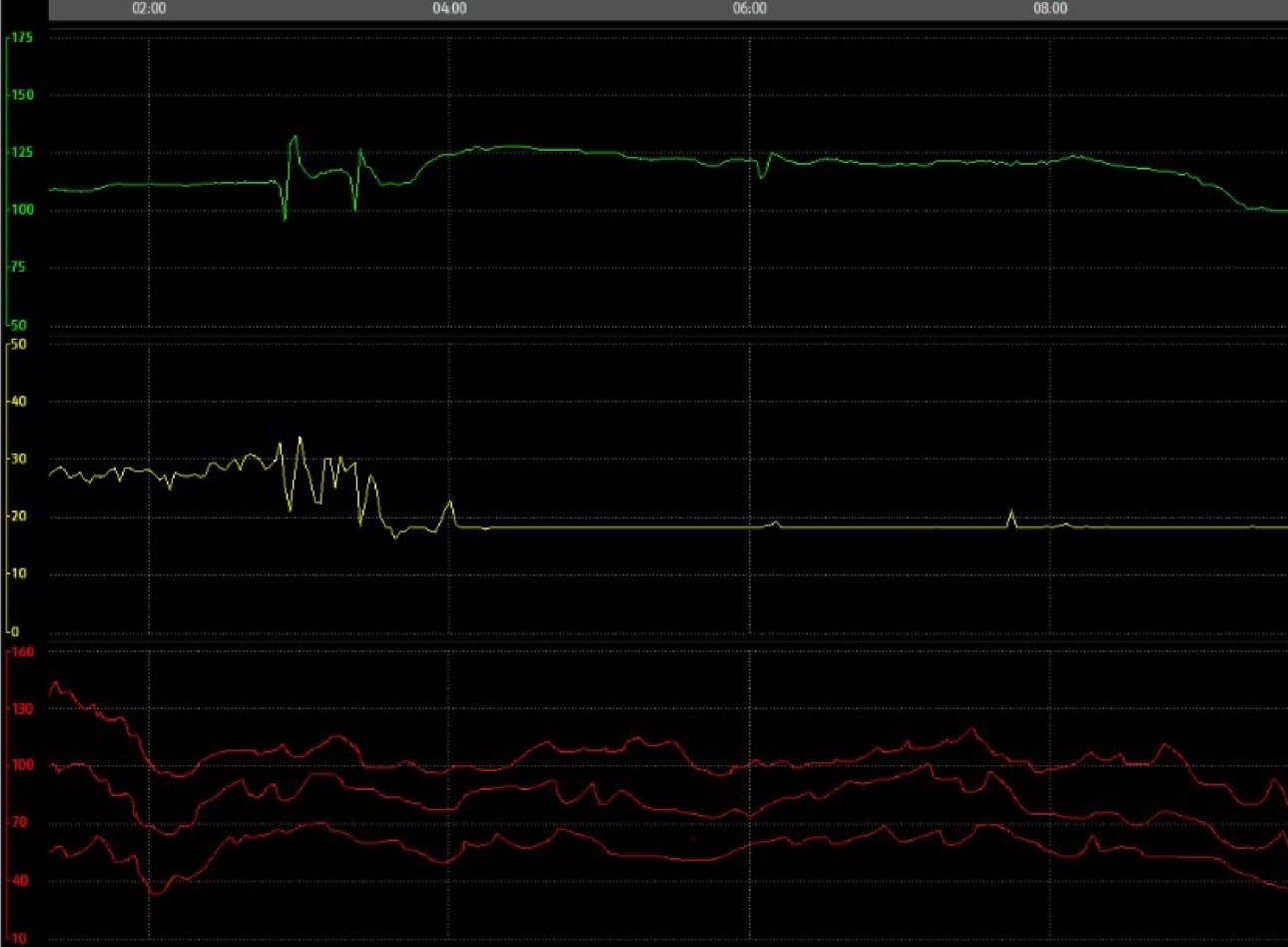
Subsequently, the patient’s condition continued to progress and blood pressure fluctuated. To maintain blood pressure and improve perfusion, the physician injected norepinephrine several times at 4:00 a.m., 5:00 a.m., and 6:00 a.m., respectively, with the dose being increased from 6 mg to 24 mg. At 5 o’clock, intravenous dobutamine was administered at a concentration of 3.6 mg/mL, 180 mg in total.
It can be found from the trend of patient’s parameters (see Figure 3) that because the abnormal status of the patient was promptly alerted, the medical staff paid more attention to the status of this patient, with close observation at the bedside. After more clinical treatment measures, the patient’s blood pressure was basically maintained within the normal range. Further exacerbation was avoided.
Case Analysis
The patient was diagnosed with multiple diseases at admission to the ICU, and the case type was extremely critical. There was a high probability of condition aggravation, such as occurrence of septic shock. For such patients, how to predict their exacerbation in the early stage for early intervention is still the focus in clinical practice.
In fact, many clinical studies have explored the prediction of the progress of shock status in patients, including heart rate[1, 2], respiratory rate[3] and arterial blood pressure[4]. Levi D. Procter, a well-known expert in the field of shock treatment and professor at the University of Kentucky College of Medicine, pointed out in the “MSD Manuals” that multiple indicators of patients should be analyzed in combination for shock diagnosis and prediction[5].
This patient experienced condition aggravation in the early morning, which was a period with fewer medical staff. Before the triggering of the prompt message, “HR >100, with Art-S ↓30 within 30 minutes, RR >22”, the patient’s blood pressure did not reach the single-parameter high-level alarm limit, so no high-level alarm was triggered, and only the single-parameter threshold of several respiratory rates reached the medium-level alarm that was triggered. But the occasional single-parameter medium-level alarm was considered by nurses to be fluctuating, which usually did not get enough attention from medical staff.
However, after the status prompt message was triggered, the prompt message was combined with the visualized monitor’s patient status guide interface, so that the clinical staff could quickly and accurately identify the aggravation of the patient’s status, and they could conduct clinical intervention for this patient in advance. The clinical value of bedside monitor alarms was maximized.
References
1. Chen, W.‐L. and Kuo, C.‐D. (2007), Characteris- tics of Heart Rate Variability Can Predict Impending Septic Shock in Emergency Department Patients with Sepsis. Academic Emergency Medicine, 14: 392-397.
2. Parker MM, Shelhamer JH, Natanson C, Alling DW, Parrillo JE. Serial cardiovascular variables in survivors and nonsurvivors of human septic shock: heart rate as an early predictor of prognosis. Critical Care Medicine. 1987 Oct;15(10):923-929.
3. Loughlin P C, Sebat F, Kellett J G. Respiratory Rate: The Forgotten Vital Sign—Make It Count![J]. Joint Commission journal on quality and patient safety, 2018, 44(8): 494-499.
4. Gernardin G, Pradier C, Tiger F, et al. Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock[J]. Intensive care medicine, 1996, 22(1):
17-25.
5. https://www.merckmanuals.com/profession- al/critical- care-medicine/shock-and-fluid-resusci- tation/shock

