Diabetic Dyslipidemia - Things You Need to Know
Mindray 2021-03-23
Diabetic dyslipidemia
It is estimated that 415 million people are living with diabetes in the world, which is estimated to be 1 in 11 of the world’s adult population. 46% of people with diabetes mellitus are undiagnosed.
Diabetes mellitus is associated with a cluster of interrelated plasma lipid and lipoprotein abnormalities; this common condition is called diabetic dyslipidemia. Diabetic dyslipidemia means that the lipid profile is going in the wrong direction. It is a deadly combination that puts patients at risk for coronary heart disease and atherosclerosis.
Cardiovascular disease could be the most common cause of death in diabetic patients. And the major proportion of CVDs are attributed to the occurrence of atherogenic dyslipidemia.
Diabetic dyslipidemia prevalence
Diabetic dyslipidemia is extremely common in type 2 diabetes (T2DM) affecting around 70% of patients.[1]
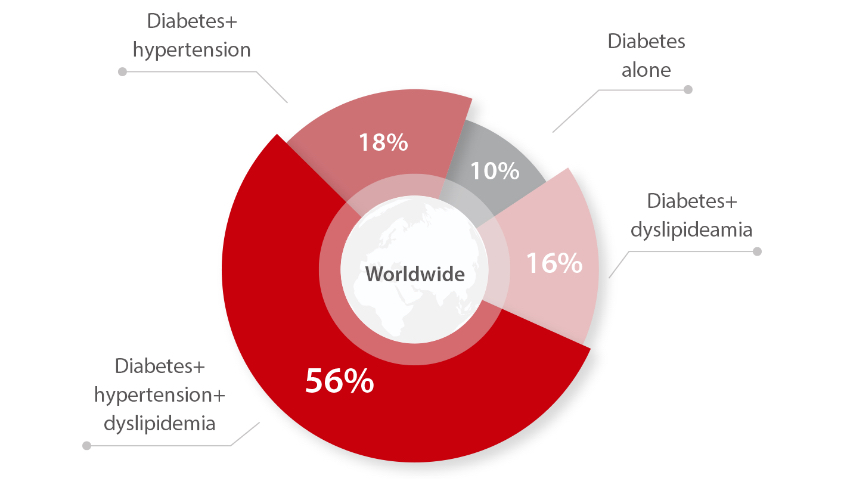
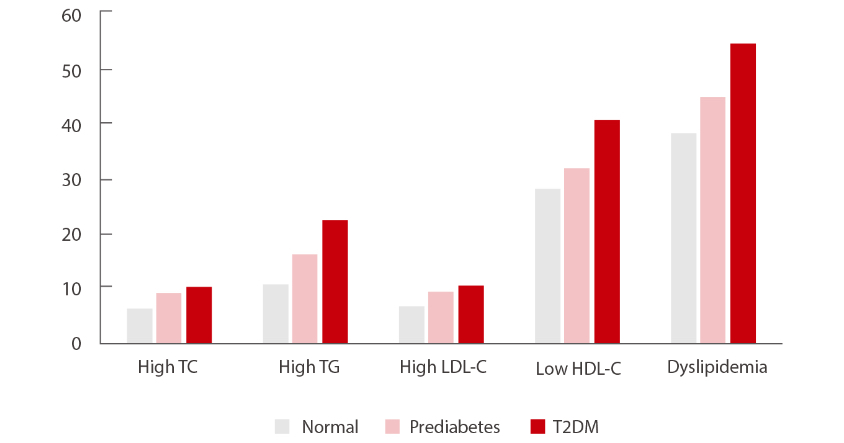
A Chinese study shows that the prevalence of dyslipidemia was 39.9%, 46.8%, and 59.3% respectively in Chinese participants with normal glucose, prediabetes, and type 2 diabetes mellitus (T2DM).[2]
Causes of dyslipidemia in diabetes
Insulin plays a central role in the regulation of lipid metabolism. Studies show a link between insulin resistance, which is a precursor to type 2 diabetes, and diabetic dyslipidemia, atherosclerosis, and blood vessel disease. Moreover, this dyslipidemia is often found in prediabetics, patients with insulin resistance but normal plasma glucose.
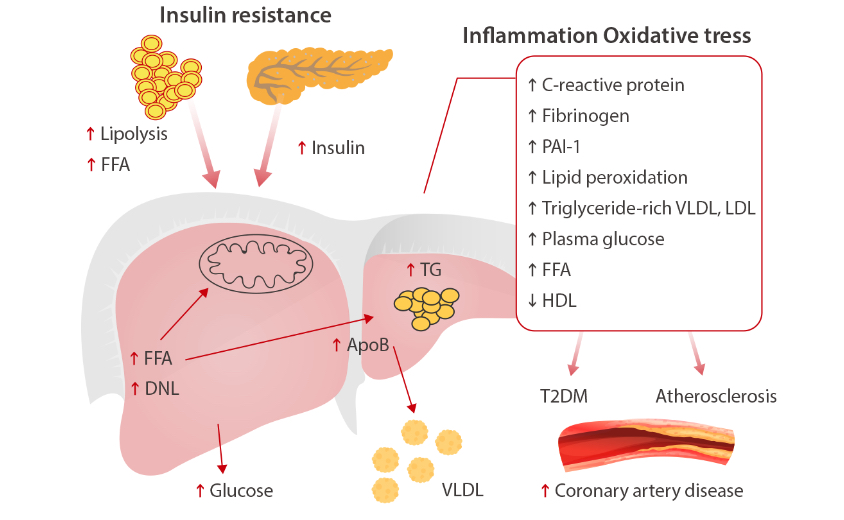
Insulin resistance is associated with an increase of free fatty acids (FFAs) flux that contributes to increased TG production that, in turn, stimulate assembly and secretion of VLDL in hepatocytes. Fat accumulation in the liver is associated with oxidative stress and lipid peroxidation. Furthermore, NAFLD subjects have increased secretion of inflammatory markers, plasma glucose, and a decrease in HDL concentration.[3]
In poorly controlled type 1 diabetes and even ketoacidosis, hypertriglyceridemia and reduced HDL commonly occur.[4]
Characteristics of diabetic dyslipidemia
Diabetic dyslipidemia comprises a complex group of potentially atherogenic lipid and lipoprotein abnormalities. It is characterized by reduced HDL cholesterol, a predominance of small dense LDL particles, and elevated triglycerides.[5]
Small dense LDL particles are a prominent feature of diabetic dyslipidemia and the number of these atherogenic particles is increased. It has been repeatedly confirmed that the concentration of plasma TG is the most important determinant of the size of LDL. On the other hand, the size of LDL decreases progressively as glucose tolerance worsens, until overt diabetes is achieved. This decrease is greater in women than in men.[6]
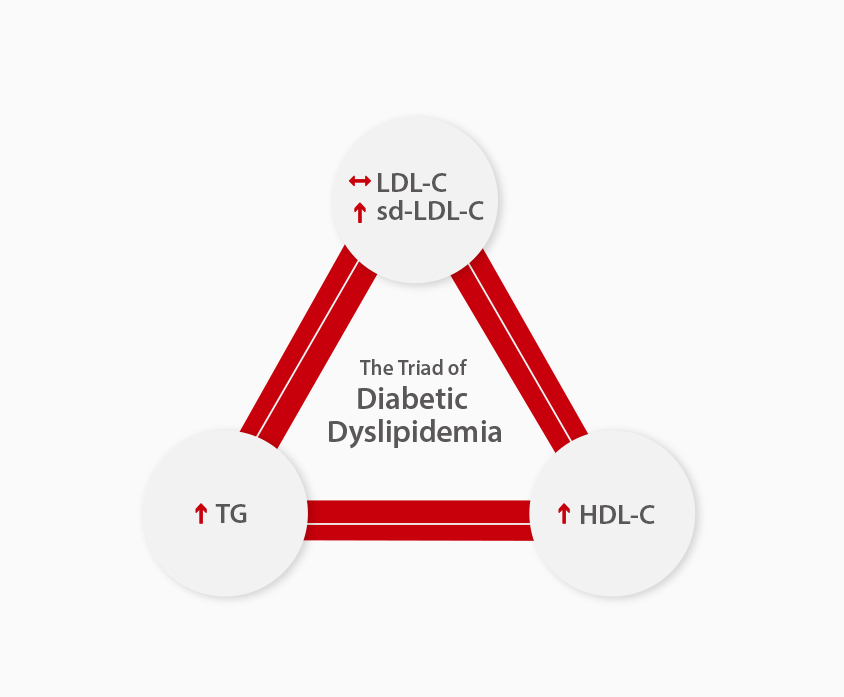
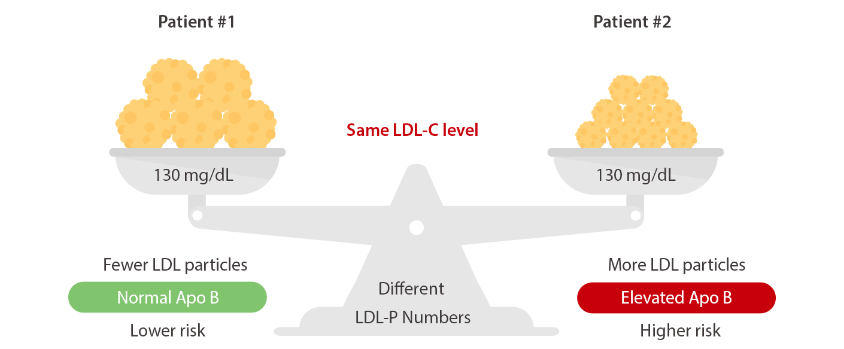
Monitoring of the conventional LDL-C may be misleading in diabetic patients; the level of LDLC is not necessarily proportional to the number of lipoprotein particles. It therefore requires specific monitoring for diabetic dyslipidemia patients.
Since each particle of LDL contains a molecule of ApoB-100, the number of small, dense LDL is increased and, similarly, the concentration of ApoB-100 increases in direct relation. Consequently, ApoB concentrations are a marker of the number of atherogenic particles and hypertriglyceridaemia with hyper-ApoB-100 is a well-known feature of diabetic dyslipidemia and other conditions.
Diabetic dyslipidemia Management
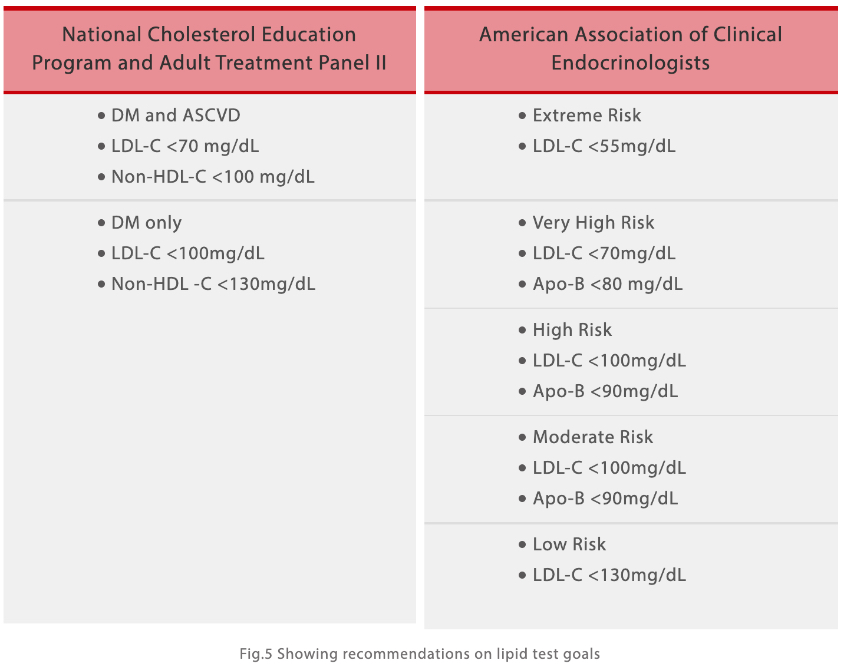
Because of frequent changes in glycemic control in patients with diabetes and the effects on levels of LDL, HDL, total cholesterol, and triglyceride, the American Diabetes Association (ADA) recommends that lipid levels should be measured every year in adult patients. If values are at low-risk levels (LDL <100 mg/dl, triglycerides <150 mg/dl, and HDL >50 mg/dl), assessment may be repeated every 2 years.[7]
Lipid goals: various guidelines have proposed different goals for LDL and HDL in diabetics. Each category with different risks should have different lipid test goals.[8]
Conclusion
Diabetes is a major public health problem; individuals with diabetes are at high risk for dyslipidemia, cardiovascular disease (CVD), and mortality. To identify and monitor those with lipid disorders, the American Diabetes Association recommends that all adults with diabetes receive a fasting lipid profile test at least annually.
References:
[1] Ishwarlal Jialal, Management of diabetic dyslipidemia: An update. World J Diabetes. 2019 May 15; 10(5): 280–290.
[2] Yaru Li,, The prevalence and risk factors of dyslipidemia in different diabetic progression stages among middle-aged and elderly populations in China. PLoS ONE 13(10): e0205709. https://doi.org/10.1371/journal.pone.0205709
[3] Melania Gaggini, etc. Non-Alcoholic Fatty Liver Disease (NAFLD) and Its Connection with Insulin Resistance, Dyslipidemia, Atherosclerosis and Coronary Heart Disease. Nutrients 2013, 5, 1544-1560.
[4] IRA J. GOLDBERG. CLINICAL REVIEW 124 Diabetic Dyslipidemia: Causes and Consequences. JCE & M, 2001 Vol. 86 No. 3
[5] RONALD M. KRAUSS, MD. Lipids and Lipoproteins in Patients With Type 2 Diabetes. Diabetes Care 2004 Jun; 27(6): 1496-1504.
[6] Iciar Martín-Timón, etc. Update on the Management of Diabetic Dyslipidaemia. EMJ Diabet. 2018;6[1]:53-61.
[7] American Diabetes Association, Dyslipidemia Management in Adults With Diabetes. Diabetes Care 2004 Jan; 27(suppl 1): s68-s71.
[8] DEBASISH CHAUDHURY. Diabetic Dyslipidemia: Current Concepts in Pathophysiology and Management. Journal of Clinical and Diagnostic Research. 2018 Jan, Vol-12(1): OE06-OE09.