Introduction
Occult stress urinary incontinence (SUI) – In women without symptoms of SUI, occult SUI describes the finding of SUI that is apparent only during clinical or urodynamic urinary function testing when the prolapse is reduced (ie, stress testing with reduction of prolapsed structures). Occult stress incontinence is also referred to as latent, hidden, iatrogenic, or potential. There are inconsistent definitions of occult SUI in the medical literature. While some authors use the term to describe only incontinence that has been demonstrated on urinary function testing (as in this topic review), others use the term occult incontinence to highlight the possibility that SUI will occur after prolapse repair.
Mechanism
Occult SUI occurs because, in women with significant anterior or apical prolapse (usually prolapse past the vaginal introitus), the bladder neck is displaced posteriorly, and the urethra is relatively kinked, resulting in some degree of urethral obstruction. The urethral kinking then becomes the mechanism of continence. When the prolapsed structures are replaced (approximating normal anatomy) during prolapse reduction testing in women with urethral obstruction due to advanced POP, the urethra is unblocked, and SUI often becomes evident when a urinary stress test is performed (ie, occult SUI). By contrast, women with stage I POP are unlikely to have urethral kinking and resultant occult SUI.
A 49-year-old patient, G4P2, complained of a sensation of a foreign body in the perineum area during long walking, physical exertion, difficulties with urination (frequent small portions, feeling of incomplete emptying of the bladder), intermittent urinary incontinence. These complaints have been bothering for 6 years.
Consulted by the Center's surgeon, sent for further examination to resolve the issue of surgical treatment.
- From the anamnesis: 2 vaginal deliveries, in both cases, taking a Crystal, a protracted 2 period of labor. The weight of newborns is 3430 g and 3910 g.
- Menstrual cycle is irregular, cycle delay up to 3-5 months in the last 2 years.
- Objective during the inspection: height 164 cm, Weight 73 kg, BMI 27 kg/m2
- Valsalva test – negative, cough – negative.
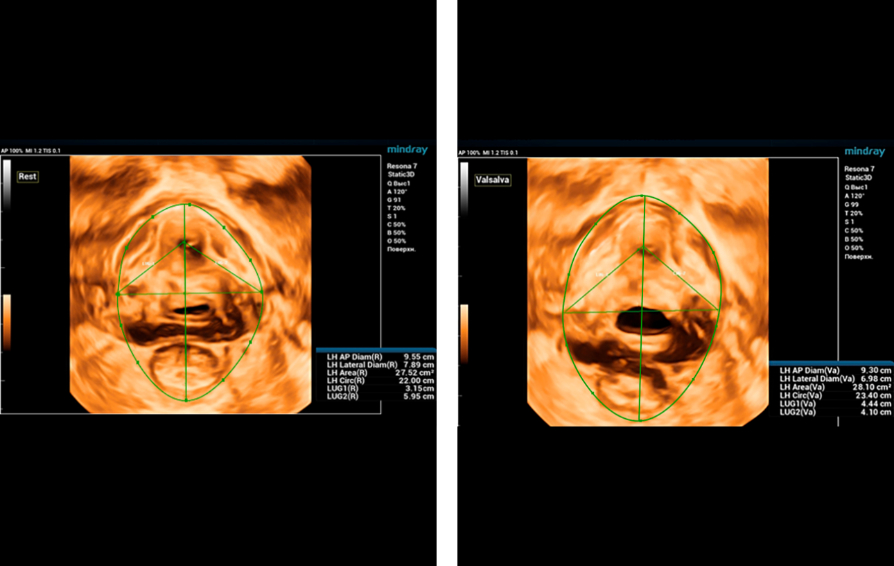
During ultrasound examination using Endocavity volume convex array transducer (DE10-3WU, Resona 7, Mindray), tearing of both levator ani muscles on the right and left is visualized, thinning of the tendon center of the perineum to 3-4 mm, the distance LH (levator hiatus) is increased – 6.13 cm, LUG1 ( One side of the levator-urethra gap) – 2.95 cm and LUG2 – 3.15 cm (normally less than 2.5 cm)
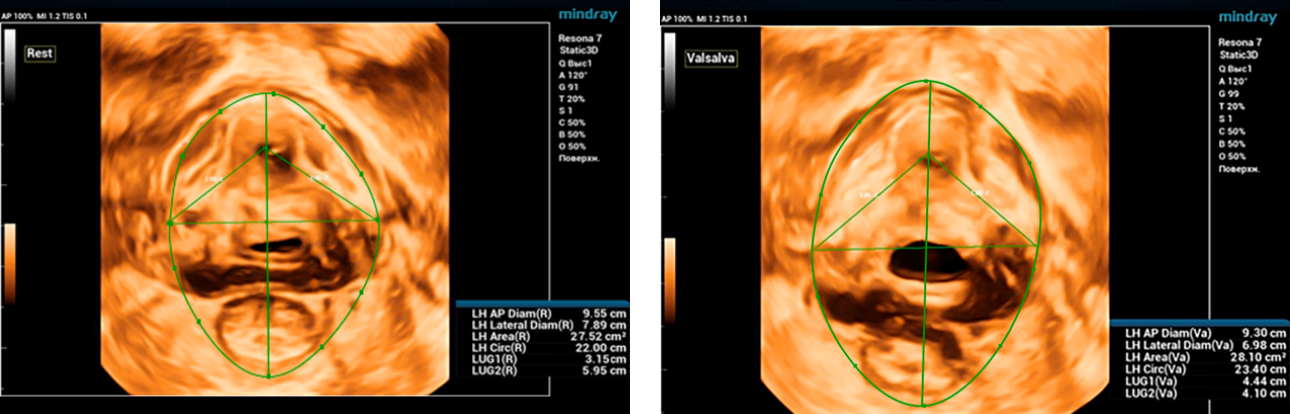
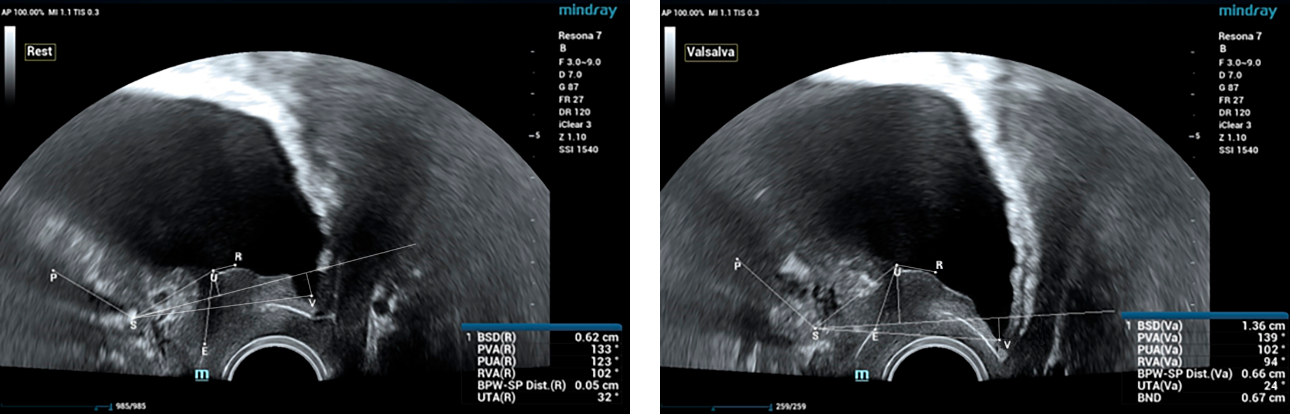
One of the important causes of stress urinary incontinence is hypermobility of the urethra, for the diagnosis of which, during ultrasound of the pelvic floor, functional tests (Valsalva and / or cough) are required. In this clinical case, the PVA, RVA and PUA indicators will be rejected by more than 20°. In this clinical case, PVA – 134°, RVA – 82° and PUA – 119°.
The anatomical length of the urethra is determined at rest and with a Valsalva test. Normally, this indicator can vary from 30 mm to 42 mm. In addition, with hypermobility of the urethra, the expansion of the proximal and middle urethra at rest and during straining can be determined. In this patient R. at rest, the width of the urethra in the proximal part is 7 mm, when strained – 8 mm.
Thus, thanks to the ultrasound of the pelvic floor, latent stress urinary incontinence in the patient was revealed. In such cases, it is recommended to perform surgical operations: colpoperineography, levatoroplasty and sling urethropexy (TVT-O). Otherwise, after plastic surgery only to correct prolapse due to changes in the urethro-vesical angle, this woman would be worried about the symptoms of stress urinary incontinence.
Conclusion
All women with genital prolapse before surgical treatment are shown additional examination to detect latent urinary incontinence. The generally accepted tactic allows you to do this examination using the invasive method of CUDI (complex urodynamic examination), a trial test with a pessary (it takes about 7 days to wear a pessary for a long time). Ultrasound of the pelvic floor with 3D reconstruction and functional tests has a significant advantage, because it is a dynamic non-invasive method of examination, which significantly accelerates and clarifies the method of surgical treatment of the patient.