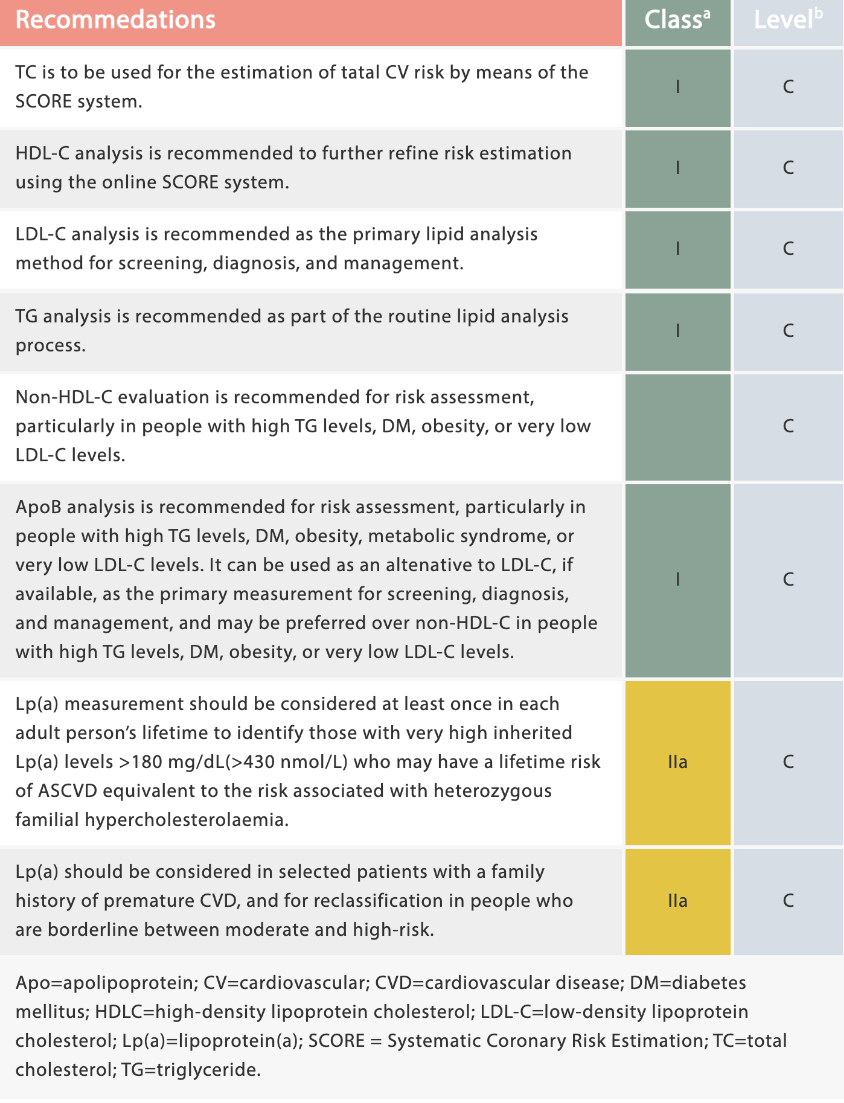
It is widely accepted that laboratory investigation of lipid metabolism is clinically significant for estimating the risk of atherosclerotic cardiovascular disease (ASCVD) and guiding therapeutic decision-making. As recommended by the 2019 ESC/EAS Guidelines for the management of dyslipidaemias, plasma lipid analysis (e.g. TG, TC, HDL-C, LDL-C, apo B, Lp(a), etc.) and proper treatment are meaningful ways of reducing the risk of ASCVD events.[1]
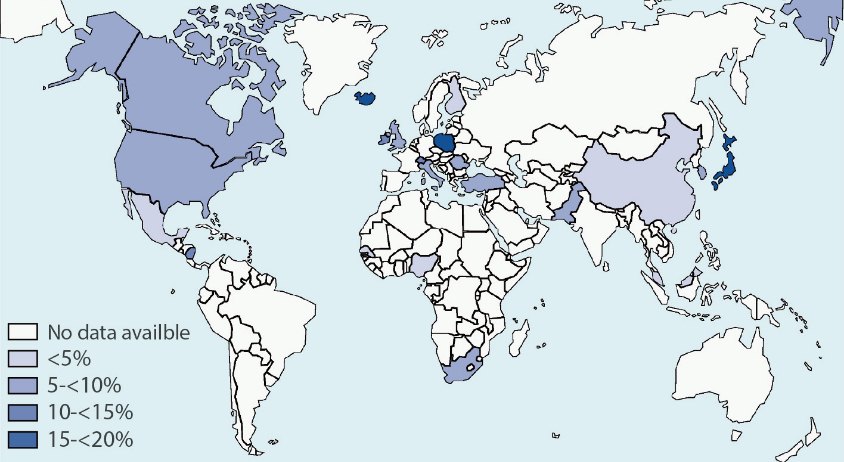
Chronic kidney disease (CKD) is one of the world’s leading health problems. The estimated prevalence of CKD is 13.4% (11.7%-15.1%), and it is estimated that there are between 4.9 million and 7.1 million patients with end-stage kidney disease needing renal replacement therapy worldwide.[2]
Most patients with CKD are at risk of accelerated cardiovascular disease and death, and many of the cardiovascular comorbidities could be related to dyslipidemia, even though there are significant differences in terms of population, the etiologies of renal damage, the stages of disease progression, and the therapeutic interventions. The level, composition, and quality of plasma lipids could be affected by the altered renal function. The characteristic lipid pattern in patients with CKD stage 3 or higher consists of hypertriglyceridemia, low levels of HDL cholesterol, low levels of Apo A1 and variable levels of LDL cholesterol and total cholesterol. Lp(a) levels could also increase in association with CKD.[1,4]
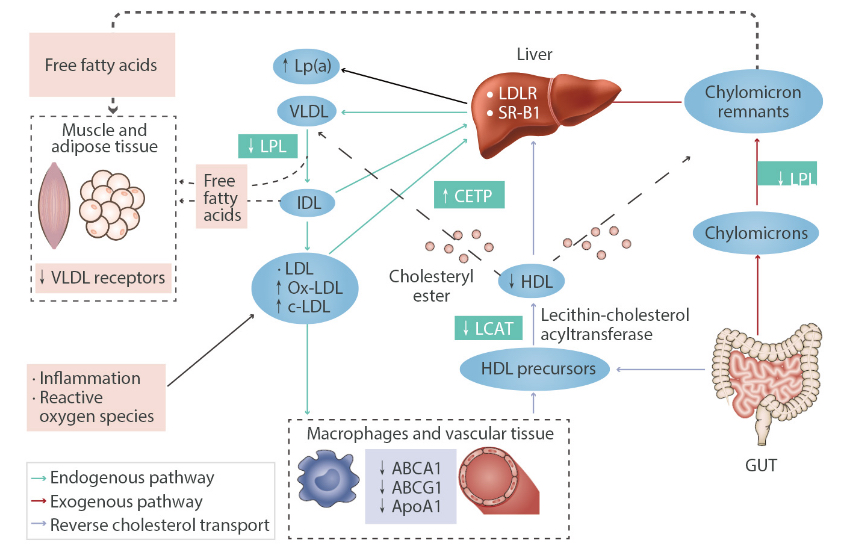
Hypertriglyceridemia in CKD results from the delayed catabolism of triglyceride-rich lipoproteins. Apo A1 synthesis is reduced in patients with CKD, and the activation of LCAT by Apo A1 is also decreased. The maturation of HDL precursors is consequently affected. Increased Lp(a) is caused by post-translation modification of lipoproteins related to CKD.
Consequently, because of the relationship between CKD and dyslipidemia, lipid evaluation is suggested to assist in managing the condition for many patients.
The Kidney Disease: Improving Global Outcomes (KDIGO) organization published its latest guidelines in 2013. As recommended in the clinical practice guidelines, all adults with newly identified CKD (including those treated with chronic dialysis or kidney transplantation) should be evaluated with a lipid profile (TG, TC, LDL-C, and HDL-C). Fasting lipid profile tests are suggested, especially for patients with known significant lipid abnormalities. Additionally, for some CKD patients under the age of 50, lipid analysis could help initiate statin therapy and identify any underlying secondary causes of severe hypercholesterolemia and/or hypertriglyceridemia.[5]
For patients who have undergone kidney transplantation, dyslipidemias could be very common, which would put them at high risk of ASCVD and transplant arterial vasculopathy. It is recommended that these patients are assessed for their the risk of developing ASCVD, and a full lipid analysis is helpful. If the lipid profile moves back to a more normal pattern and such changes are sustained, the risk of ASCVD could be significantly reduced.[6,7]
Conversely, unlike the LDL-C surveillance involved in managing most patients’ treatment, lipid level monitoring is not suggested by the KDIGO work group (2013) in CKD patients with decreased GFR due to the lack of direct evidence. As low GFR is an independent risk factor to ASCVD, strict lipid-lowering therapy would not change medical management or reduce the risk of major cardiovascular events.[5]
However, some trials have revealed that lowering LDL-C is of benefit, as it reduces the cardiovascular risk of CKD patients not requiring dialysis (including kidney transplant recipients), while other guidelines do suggest lipid monitoring to ensure the cholesterol reduction target is met.[4] Therefore, lipid analysis has great potential in the management of CKD patients: in assessing adherence to statin treatment, changes in the renal replacement therapy modality, or concerns about the presence of a new secondary cause of dyslipidemia, and even assessing the 10-year cardiovascular risk in patients aged < 50 years and not currently receiving a statin.[5]
To sum up, lipid analysis plays a crucial role in the reduction of ASCVD risks, although lipid testing is quite complicated in patients with CKD, a common medical condition worldwide. All patients with newly identified CKD should undergo lipid analysis, and many of said patients could benefit from medical intervention based on lipid monitoring.

References:
[1] François Mach, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. European Heart Journal, 2020(1)41, 111–188, https://doi.org/10.1093/eurheartj/ehz455
[2] Lv JC, Zhang LX. Prevalence and Disease Burden of Chronic Kidney Disease. Adv Exp Med Biol. 2019; 1165:3-15. doi: 10.1007/978-981-13-8871-2_1
[3] Webster, A., Nagler, E., Morton, R. et al. Chronic kidney disease.The Lancet. 2017; 389: 1238-1252. https://doi.org/10.1016/S0140-6736(16)32064-5
[4] Ferro, C.J., Mark, P.B., Kanbay, M. et al. Lipid management in patients with chronic kidney disease.Nat Rev Nephrol. 14, 727–749 (2018). https://doi.org/10.1038/s41581-018-0072-9
[5] Wanner C, Tonelli M, et al. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014 Jun;85(6):1303-9. doi: 10.1038/ki.2014.31
[6] JJennifer L Larsen, et al. Lipid Status After Pancreas-Kidney Transplantation. Diabetes Care Jan. 1992, 15 (1) 35-42; DOI: 10.2337/diacare.15.1.35
[7] Claudio Ponticelli, et al. Treatment of dyslipidemia in kidney transplantation. Expert Opinion on Drug Safety. (2020) 19 :3, 257-267, DOI: 10.1080/14740338.2020.1732921