Three routine laboratory tests

Blood, urine and feces analysis are the three common tests in clinical laboratories. Among them, blood testing is the most important way to keep track of one’s overall physical well-being.
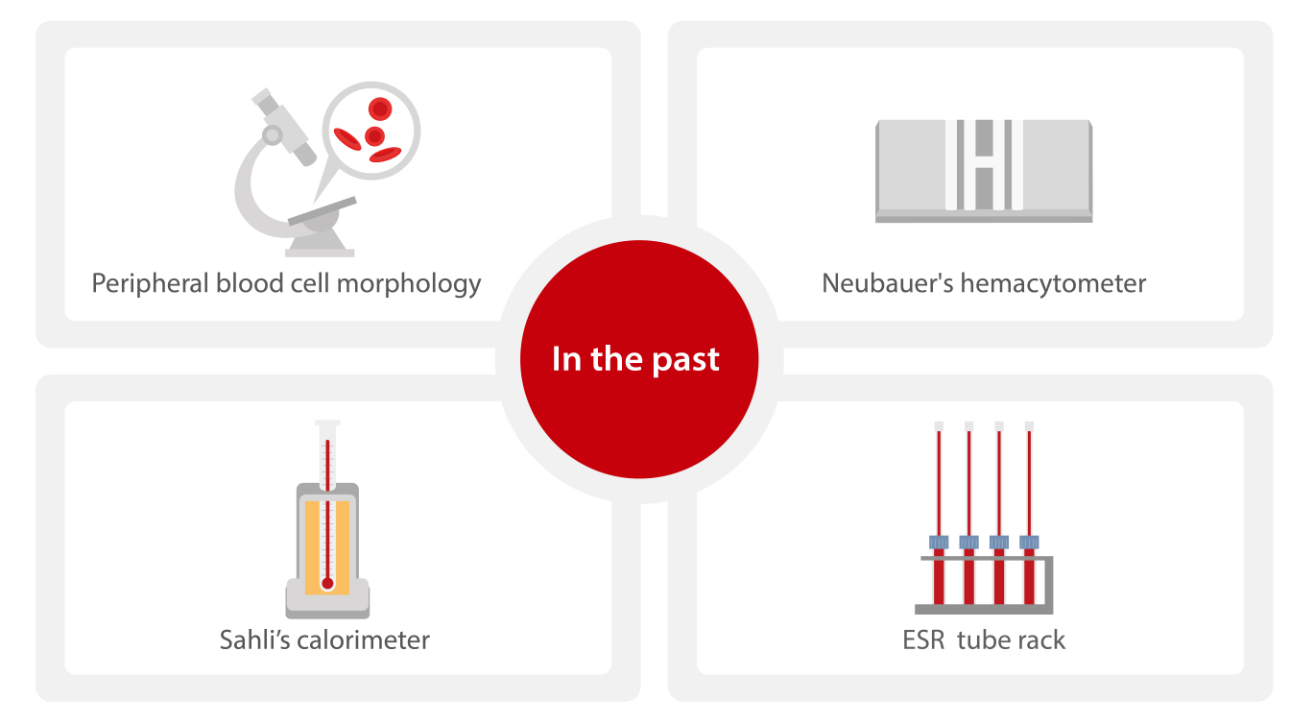
In the past, routine blood tests were performed manually on a microscope, Neubauer's hemacytometer, Sahli’s colorimeter and ESR tube rack.
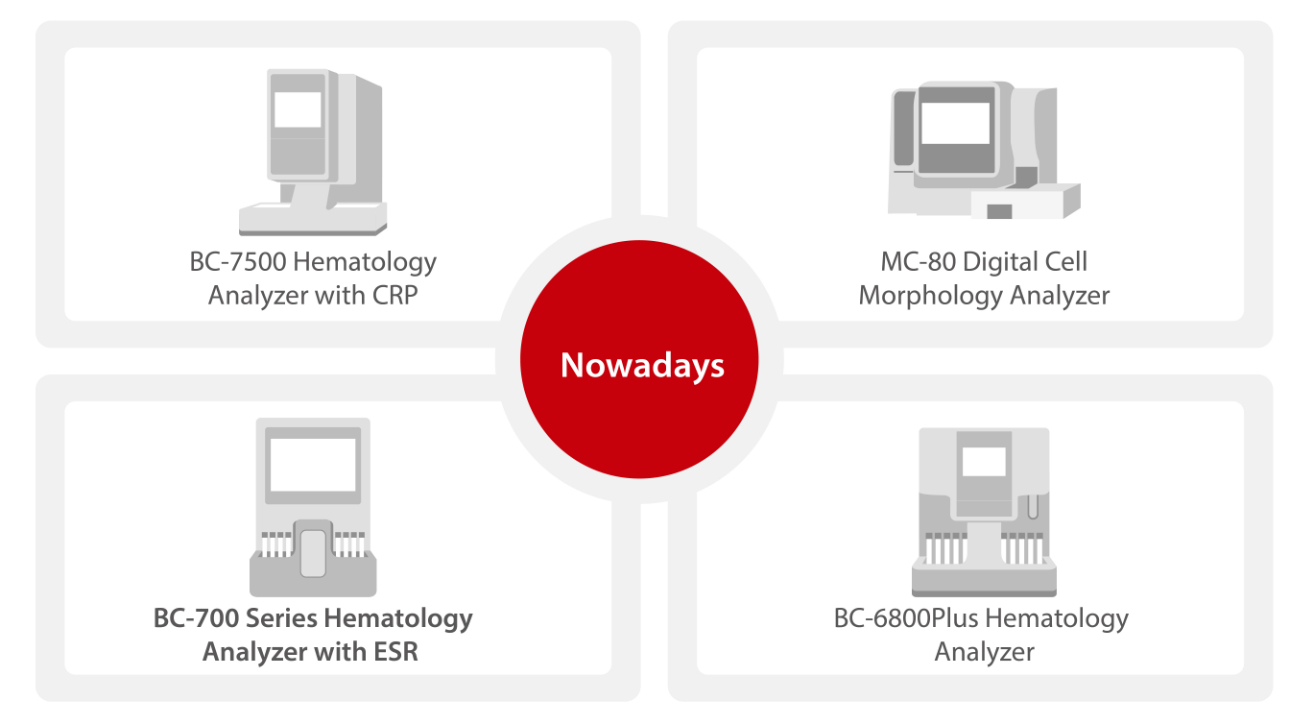
In addition to complete blood count (CBC) and white blood cell differential (DIFF) count which have become fully automated, other simple but time-consuming blood tests like ESR and CRP also transform from manual methods to automated analysis. Integrated systems have been developed for easier operation.

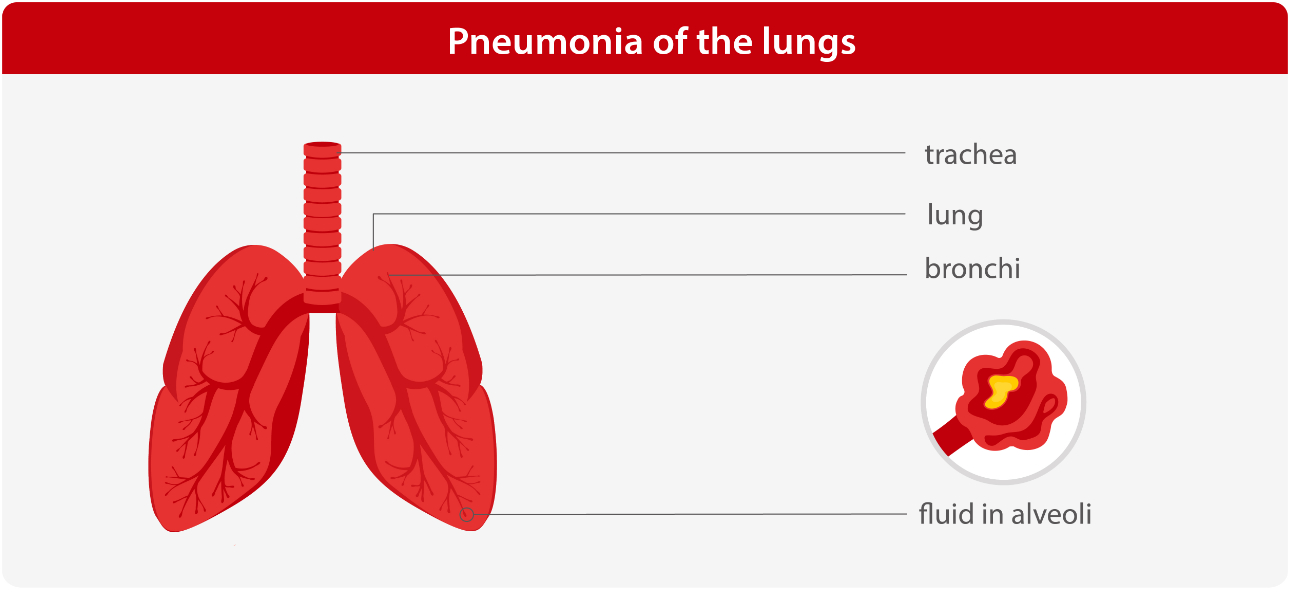
Diagnosis of pulmonary diseases
Study A
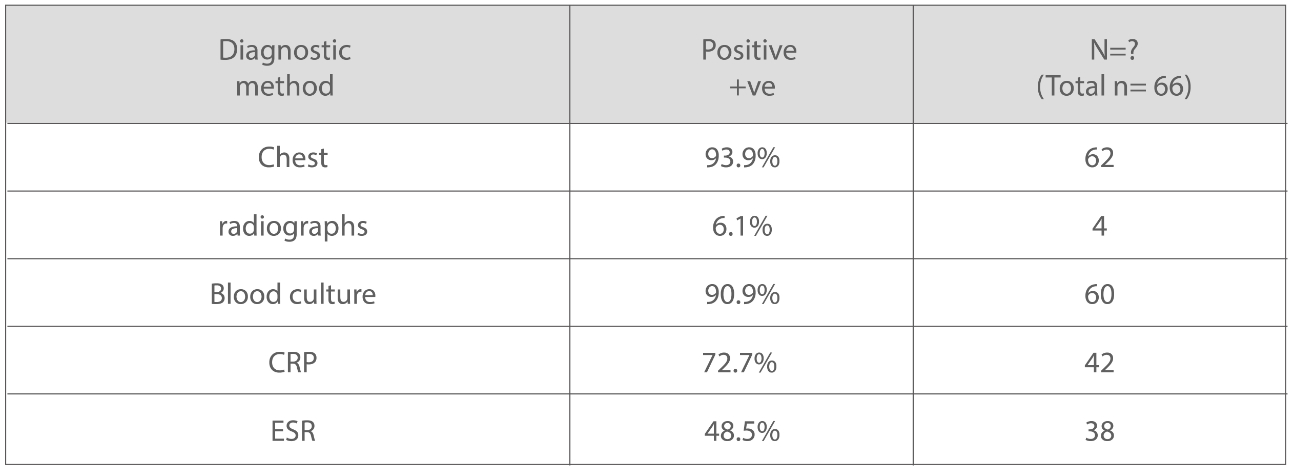
A comparison of different investigations in their sensitivities for the diagnosis of Community Acquired Pneumonia (CAP)
Age group
Diagnostic methods
Results
Conclusion
Both CRP and ESR analysis can be used as an alternative test to the chest radiographs at peripheral centres, where X-ray machines are not available.
Study B
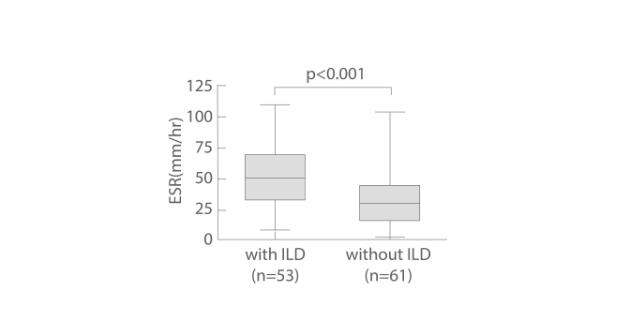
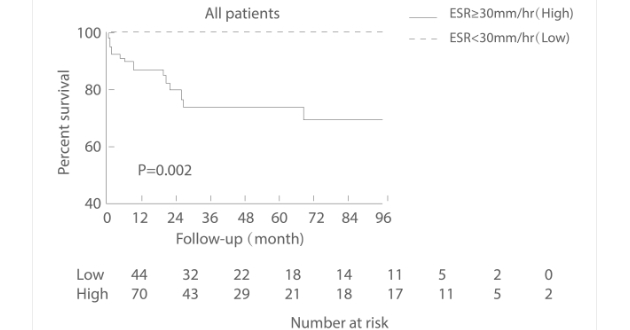
Elevated Erythrocyte Sedimentation Rate Is Predictive of Interstitial Lung Disease and Mortality in Dermatomyositis: A Korean Retrospective Cohort Study
Age group
Interstitial lung disease (ILD) is a major cause of death in patients with dermatomyositis (DM). This study was aimed to examine the utility of the erythrocyte sedimentation rate (ESR) as a predictor of ILD and prognostic marker of mortality in patients with DM.
Target group
Methods
Results
Association between elevation of the baseline ESR and pulmonary impairment in patients with DM.
Conclusion
Elevated ESR is associated with increased mortality in patients with DM due to respiratory failure. Thus, monitoring ESR should be an integral part of the clinical care of DM patients.
Applications in covid-19
Study C
Blood markers (percentage of lymophocytes, neutrophils, CRP and ESR can help prioritize RT-PCR testing in patients suspected of Covid-19 in countries with limited health resources.
Target group
Methods
Results
Lymphocytes % showed decrease to 9.2 (P-value=0.000) and significant increase inneutrophils to 83.05 (P-value=0.005), ESR to 65.54 (P-value=0.000) and CRP to 91.07 (P-value=0.000).
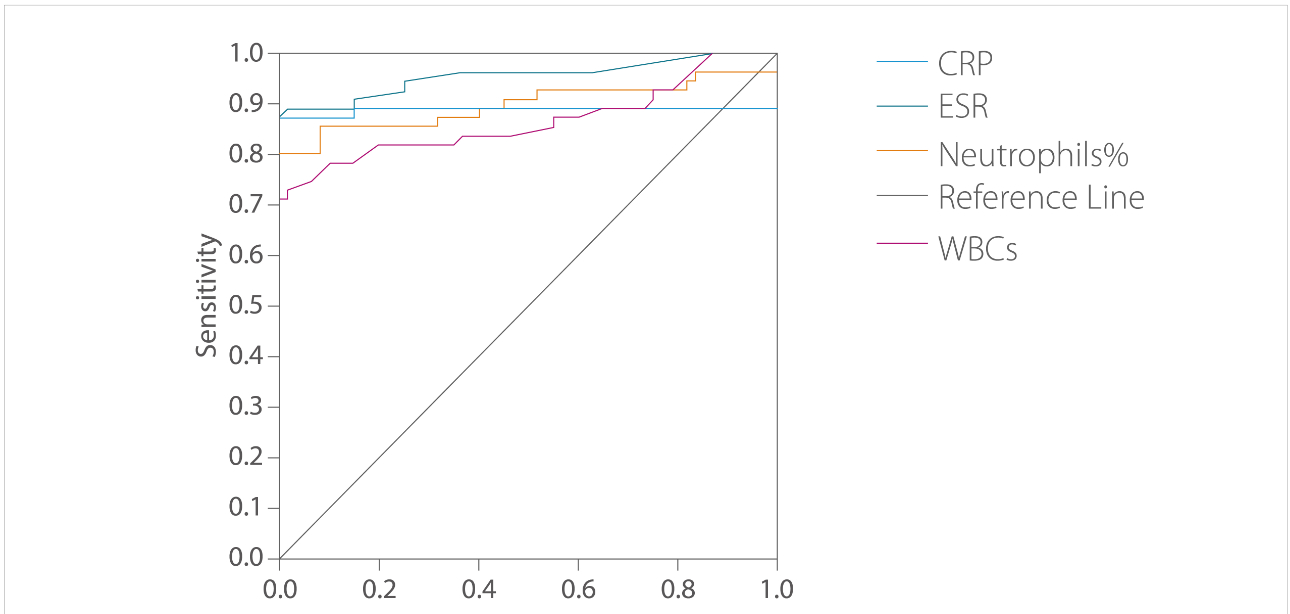
The receiver operating characteristic curve (ROC)/area under the curve (AUC) ensured the expellant result of lymphocytes % as a predictor with 92% area under the curve, neutrophils were 90% and ESR 95.8%.
The percent of detecting COVID-19 positive RT-PCR (98%) for suspected individuals using ROC showed best cutoff of ≤21.8 for lymphocytes %, ≥67.7 for neutrophils, ≥37.5 for ESR, ≥6.2 for CRP and ≥7.15 for WBCs.
Conclusion
Lymphocyte percentages, neutrophils, CRP and ESR can be used as markers for COVID-19, helping in prioritizing individuals for rRT-PCR tests.
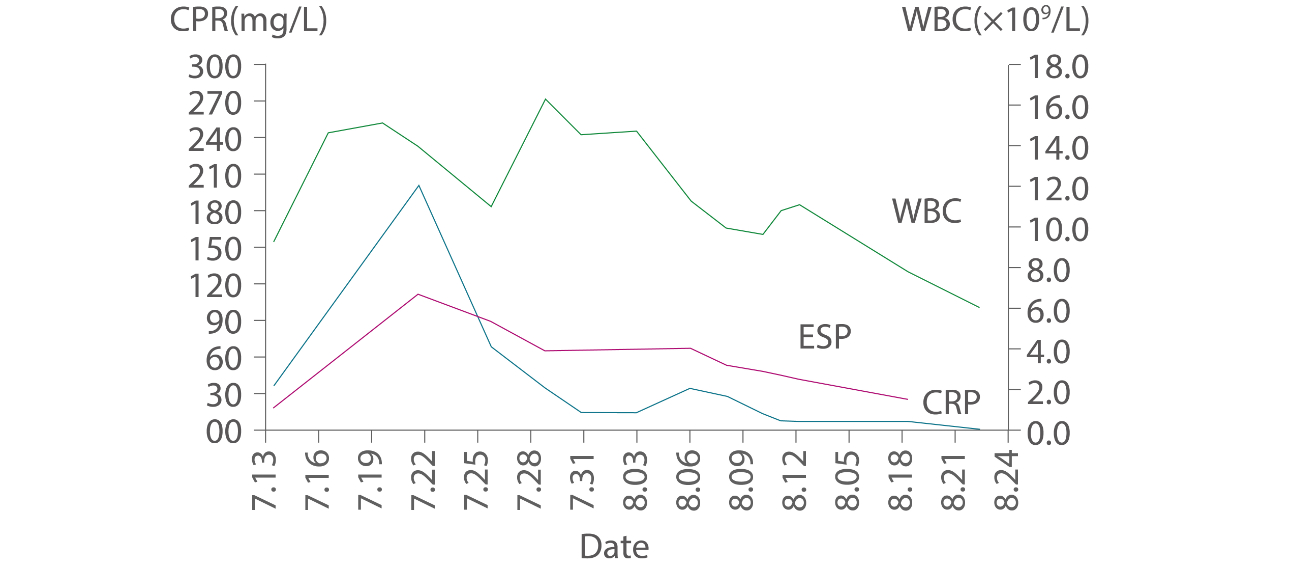
Diagnostic value of combined ESR and WBC tests for inflammation
- ESR and CRP are traditional biomarkers of inflammation.
- Elevated levels only indicate that there is a focus of inflammation somewhere in the body, but the tests cannot pinpoint the exact location of inflammation.
- ESR and CRP can be used as routine aides to detect inflammation and monitor treatment effectiveness.
- After high levels are detected, the patient should undergo reexamination every 1 to 3 months to help determine whether the treatment is successful in reducing inflammation.
Mindray is going to launch a new hematology series that incorporates both CBC and ESR analysis. Stay tuned for our global launch lunch event on March 2!
Register to the BC-700 Series Hematology AnalyzerVirtual Launch Event
References
[1] Sections 1–4, Chapter Two in Volume I of Clinical Laboratory Medicine Foundation (Version 2), China Medical Science and Technology Press
[2] Section I FBC Tests in Chapter 2 of Manual for Clinical Laboratory Diagnosis, People’s Military Medical Press
[3] Routine Blood Tests in User Manual for Tests (Version 2), Peking University Shenzhen Hospital
[4] Lakhani D, Muley P. The association of positive chest radiograph and laboratory parameters with community acquired pneumonia in children. Journal of Clinical and Diagnostic Research. 2013; 7(8):1629-1631
[5] Dhairya L, Prasad M. The Association of Positive Chest Radiograph and Laboratory Parameters with Community Acquired Pneumonia in Children.Journal of diagnostic research. 7(8): 1629–1631. DOI : 10.7860/JCDR/2013/5132.3222, 2013
[6] Dong J, Eun Y. Elevated Erythrocyte Sedimentation Rate Is Predictive of Interstitial Lung Disease and Mortality in Dermatomyositis: a Korean RetrospectiveCohort Study. J Korean Med Sci. 2016; 31(3): 389–396. doi: 10.3346/jkms.2016.31.3.389