Ultrasound Journal 5: A Hidden World Under the Mucosa
A Case Report of Ectopic Pancreas in the Stomach Wall by Ultrasonography
2022-06-09
Special thanks to Dr. Liu Xun, Fifth Central Hospital of Tianjin.
Key points
- Contrast-enhanced ultrasound through the gastric window after oral administration of gastrointestinal contrast agent, reveals the clear anatomical structures and morphological characteristics of the lesions in all layers of the gastric wall
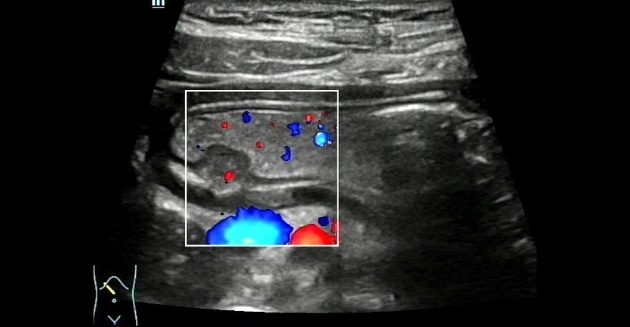
- Color Doppler can be used to demonstrate blood flow into an ectopic pancreas
Case Description:
A 32-year-old female presented to the hospital with intermittent epigastric discomfort for more than 1 year. She was previously in good health, with a history of gastrointestinal malignancy in her paternal line and no abnormalities in any laboratory tests.
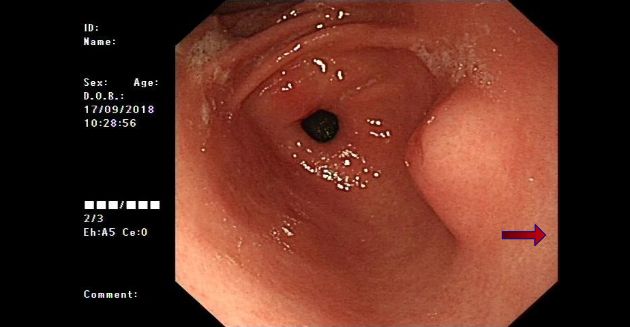
In 2018, she was diagnosed with chronic gastritis and a submucosal bulging mass on the lesser curvature of the gastric antrum by gastroscopy (Figure 1).
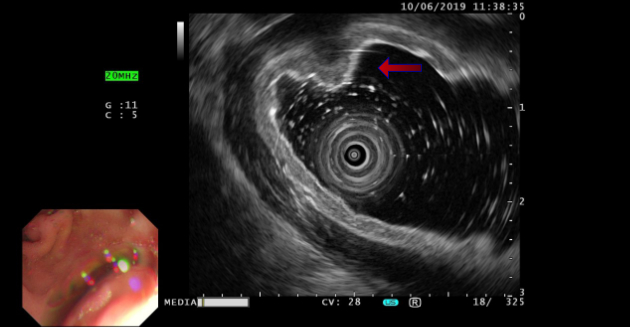
In 2019, ultrasound endoscopy still indicated a submucosal bulging mass on the lesser curvature of the gastric antrum, and submucosal ectopic pancreas was considered. (Figure 2).
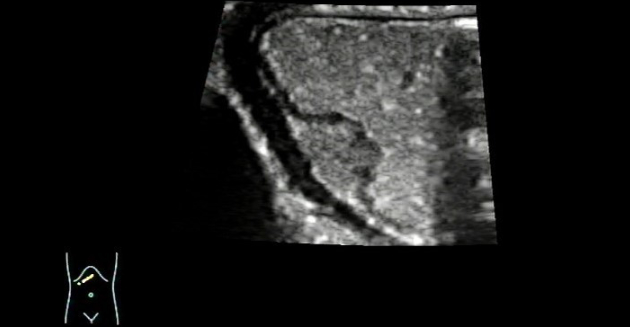
Contrast-enhanced ultrasound imaging of the gastric window:
The patient underwent ultrasound examination after drinking 500 mL of contrast agent (instant gastrointestinal ultrasound aid) in a fasted state. The gastric wall featured a clear well-layered structure and a lack of mucosal smoothness, and a moderately hypoechoic mass of about 1.36 cm × 0.87 cm in size was detected in the submucosal layer of the lesser curvature of the gastric antrum. The mass was ovoid with clear margins, a broad base, and a continuous mucosal surface.
Moreover, a shallow depression was spotted in the center of the mass, with uneven echogenicity inside the mass (Figure 3).
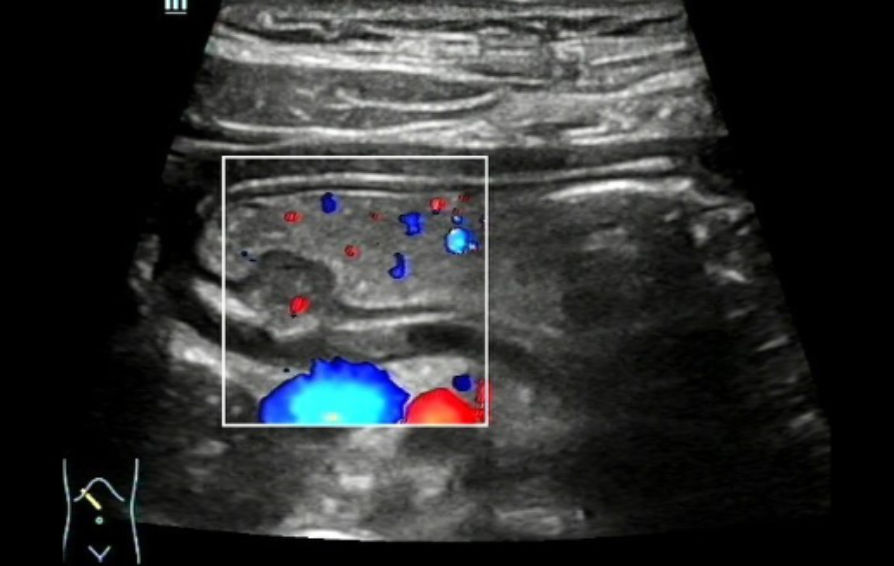
Color Doppler Flow Imaging (CDFI) revealed that a signal indicative of a thin stream of blood flow could be identified near the base of the mass. (Figure 4). Ultrasound indicated a submucosal occupying lesion in the stomach, and ectopic pancreas was suspected.
Procedure:
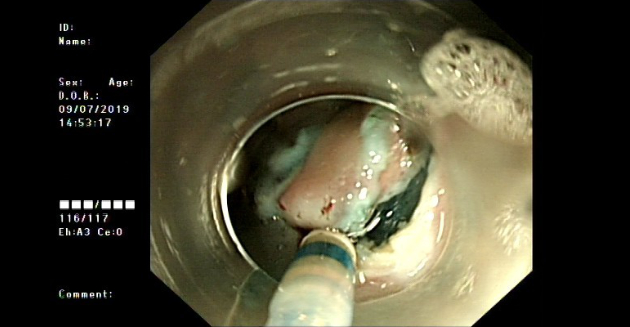
The patient had no contraindication to surgery for the examinations and endoscopic submucosal dissection (ESD) was performed. (Figure 5)
Postoperative diagnosis:
Pathology diagnosed chronic inflammation of the gastric mucosa with visible ectopic pancreatic tissue under the mucosa.
Discussion:
Ectopic pancreas, also known as the aberrant pancreas or the accessory pancreas, is a congenital anomaly. About 90% of ectopic pancreas cases are found in the upper gastrointestinal tract, but they have also been seen in the jejunum, ileum, Meckel diverticulum, gallbladder, bile duct, and other sites. Most lesions of ectopic pancreas are solitary, primarily arising in submucosa and rarely in the muscular layer. They most often form a local disc-shaped mass with unclear margins, protruding from the mucosal surface into the gastric cavity, and are generally less than 2.0 cm in diameter, but have also been reported as polypoid.
The imaging manifestations of ectopic pancreas vary depending on the composition of the acini and pancreatic ducts. Most lesions are isoechoic, with a few being hypoechoic. The sonogram features a medium- or hypo-echoic substantial mass arising from the submucosa of the stomach, mostly with local thickening, uneven internal echogenicity, and a clear well-layered structure of the gastric wall around the mass. Ectopic pancreas occurring in the submucosa often has an umbilical depression on the surface due to the central-duct opening in the digestive tract.
Ultrasound findings revealed no abnormal changes in the mucosal layer, mucosal muscle layer, muscle layer, or serosal layer on the surface of the mass in this case. The mass was hypoechoic in the wide base of the submucosal layer with a mild central depression at the top, but there was no sound attenuation behind the mass, whose slow movement with the gastric peristaltic wave could be easily confused with the peripheral thick mucosal folds. Therefore, the clinician should wait patiently for the peristaltic wave to subside and the mass contour to stabilize before making a thorough diagnosis of suspicious lesions in the gastric wall. As contrasted with previous studies reporting no blood flow signal in ectopic pancreatic tissue, Color Doppler ultrasound (CDUS) in this case demonstrated a thin stream of blood flow at the base of the mass, thereby expanding our understanding of blood supply to the gastric ectopic pancreas and demonstrating that a blood flow can exist at the base of the ectopic pancreas.
This disease should be differentiated from gastric leiomyoma and mesenchymoma, since all of them are submucosal lesions. After oral administration of gastrointestinal contrast agent, contrast-enhanced ultrasound through the gastric window can reveal the clear anatomical structures and morphological characteristics of the lesions in all layers of the gastric wall, thus facilitating the differential diagnosis of the above diseases.