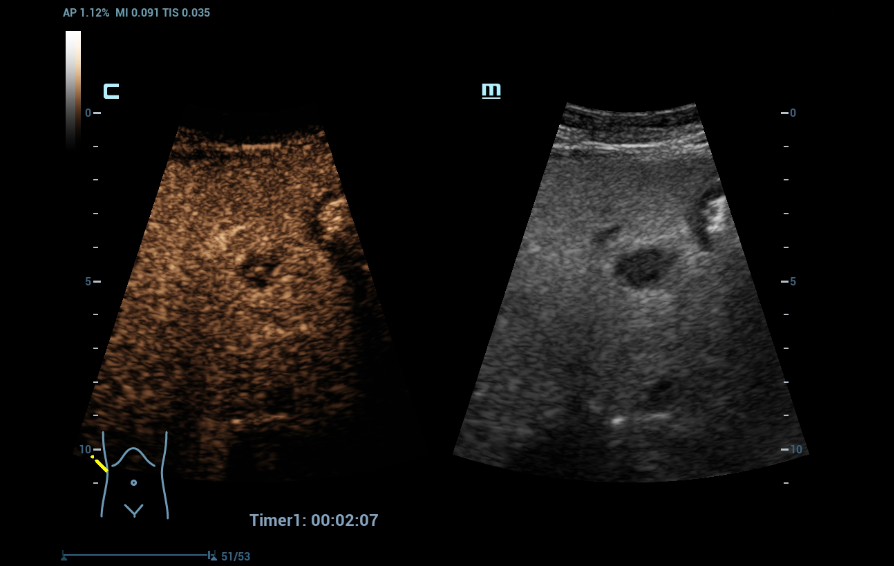
Contrast-enhanced ultrasound (CEUS) is already recognized as having a high diagnostic value in the examination of the liver. Recent technological advances promise to further improve the image quality of CEUS, with the potential to provide performance characteristics equivalent to other imaging modalities such as CT or MRI. Such an advance is the new high-frame rate CEUS (HiFR-CEUS) technique.
Mindray is excited to share an insightful interview conducted by Guido Gebhardt with two notable medical experts, Professor Christian Stroszczynski and Professor Ernst Michael Jung. Professor Stroszczynski serves as the Director of the Institute of Diagnostic Radiology, while Professor Jung is the Radiological Director of the Interdisciplinary Ultrasound Center at the University Hospital Regensburg in Germany.
The interview primarily discusses the significance of HiFR-CEUS in diagnosing liver lesions, its potential for improving diagnostic safety, and future advancements in ultrasound technology.
Can you tell us about a case in which HiFR CEUS was particularly useful in diagnosing a patient's condition?
Stroszczynski: The case I can describe to you is a patient whose CT scan showed a primary tumor and another lesion. The subsequent MRI scan with a liver-specific contrast agent revealed four additional lesions besides the primary tumor, which had to be resected.
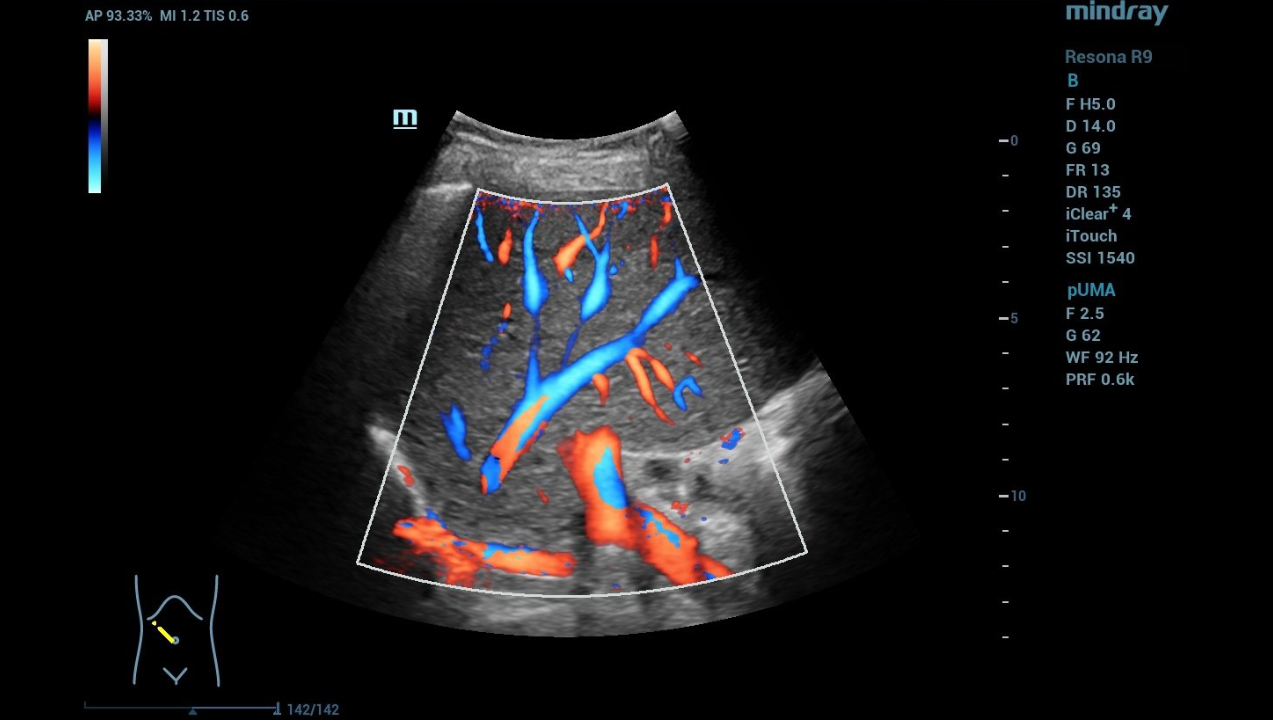
Jung: The first tumor signs are that the vessels in the surrounding area are changing. UMA ensures that I can also beam the probe from any angle also vertically and assess the morphology of the liver.
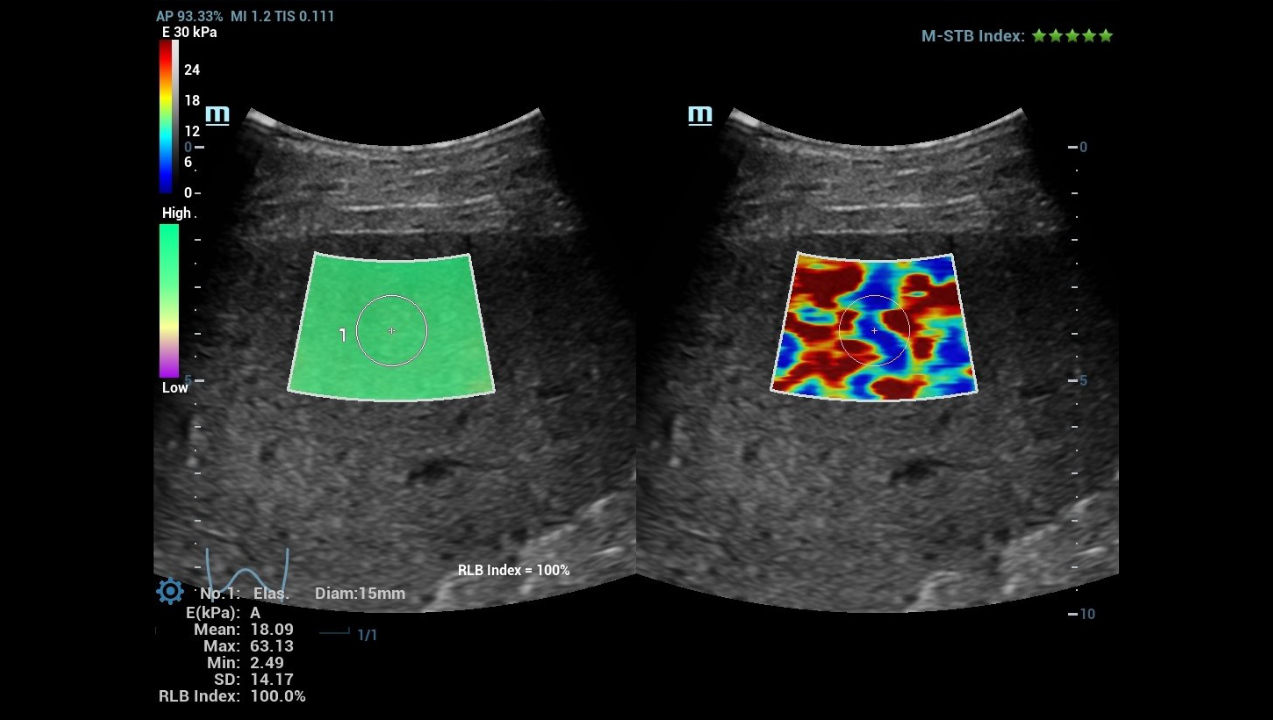
What is the significance of the Mindray zone technique ZST+ in the convex array probe and how high is the frame rate compared to the conventional CEUS?
Jung: The high-resolution convex array probes thus make a decisive contribution to advancing tumor localization and characterization.
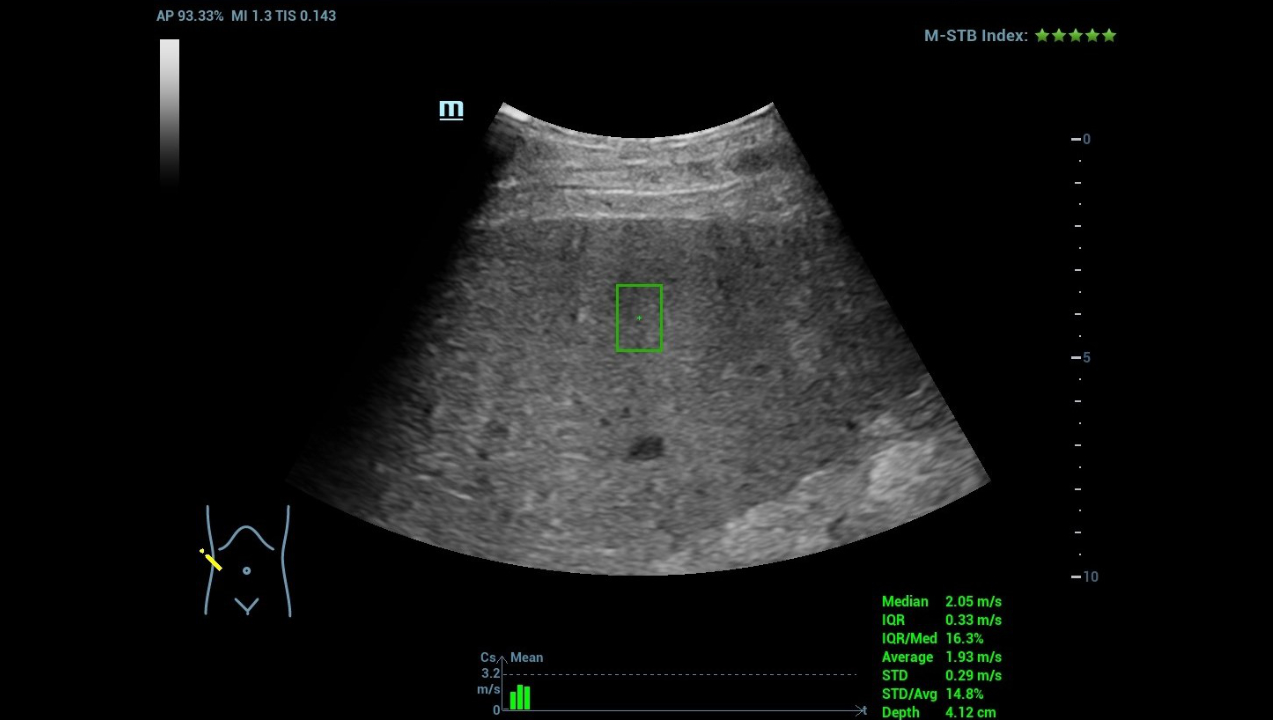
The frame rate of HIFR depends primarily on the depth of the tumor to be assessed. Close to the surface, one can expect ten times the frame rate; when depth is important, one achieves approximately three times the frame rate compared to conventional CEUS.
What is the significance of the resulting improvement in time resolution for better tracking the movement of microbubbles, which are an essential component of the sulfur hexafluoride contrast agent used in CEUS?
Jung: Contrast agent sonography can be modified based on acoustic energy. For example, to make the bubbles vibrate better it is possible to change the mechanical index (MI). Lower energy, or a low MI, allows the bubbles to vibrate longer, resulting in better image quality.
By tracking the microbubbles and changing the MI, it is possible to image the blood flow in the liver even in the capillary region. We can really see the smallest vessels and achieve up to ten times higher resolution based on the high frame rate, depending on the depth.
What is the advantage of improved observation of details of microvascular perfusion, e.g. in liver lesions, with rich blood supply and small focal liver lesions?
Jung: In an initial pilot study, we saw that in tumors, neovascularization starts at a size of 1 to 1.5 centimeter.
Can you tell us something about the details of the study?
Jung: To make a statistically significant statement, you need at least 100 cases for a study. Our goal is to combine the cases of several institutes in the planned multi-center study in order to achieve a significantly higher number of cases. The basic requirement for the evaluation of liver lesions will be that both a CT and an MRI scan with liver-specific contrast agent have been performed.
The practical approach will be to start with a B-mode scan, followed by CEUS and HiFR CEUS with UMA to gradually determine what improvements the different techniques and the convex array probe bring.
Stroszczynski: From experience, the contrast protocol depends on the examination conditions. Under optimal conditions in a 70 kg-heavy patient and with an optimal examiner, a maximum of 1.5 ml of ultrasound contrast agent can be expected. This also corresponds to the dose with which we would start the study, subsequently reducing the amount of contrast agent to 1 ml.
This is because our previous experience has already shown that 1 ml injected quickly as a bolus is sufficient to achieve good image quality, even when scanning through the abdominal wall. In a patient weighing 100 kg, about 2.4 ml is needed. Even in our heaviest patient to date -170 kg -, we reliably found the tumor.
It can be assumed that with HIFR CEUS a significant reduction in contrast agent can be expected, which of course also means lower costs.
How good is the ability of HiFR CEUS to identify and characterize focal liver lesions?
Stroszczynski: With the planned study, we want to confirm the advantages of HiFR CEUS that are already apparent. This is because our experience with CEUS to date shows that about a third of cases have low examination quality, another third has satisfactory quality, and the rest of cases have good to very good quality. The goal of the study is to show that we have created a 100 percent robust procedure with HiFR CEUS. This means that all the examinations should be of satisfactory to very good quality.
Jung: As already mentioned, up to ten times higher resolution can be achieved with the help of HiFR, depending on the depth. DEGUM studies in which we were involved have shown that a diagnostic certainty of 50-60% can be achieved with standard ultrasound. With CEUS, we are already at 70-80 %. With the new study, we would like to show that further improvement is possible with HiFR CEUS.
How do you assess the potential of HiFR CEUS and what could be the next steps in the practical development of the technology?
Jung: As the preliminary study has already shown, HiFR CEUS suggests additional potential for improvement. Of particular clinical relevance is that we can view the entire liver in a representative manner. The ultrasound examinations become reproducible and reliable. This is especially important in patients who are undergoing follow-up.
Stroszczynski: In the future, these follow-up examinations of patients with liver metastases should be performed with CEUS. Those examinations are still predominantly performed with computed tomography, although cytostatic drugs often significantly impair the CT contrast due to changes in the liver structure. This doesn’t apply to CEUS, and in cases of doubt, magnetic resonance imaging could then confirm the findings. We anticipate that this new approach will significantly improve the precision of the important follow-up assessment of chemotherapy or antibody therapy. Among other things, this would avoid unnecessary chemotherapy and surgery.
Furthermore, we would like to know what is possible in soft tissue lesions. There is also great interest in breast diagnostics and how good we can be in assessing lymph node metastases. We are also interested in moving from the millimeter to the sub-millimeter range with HiFR CEUS. That would be a huge innovation boost.
What other ultrasound innovations are you interested in?
Jung: First and foremost, we are interested in making the devices capable of learning. In addition, we are already looking at using automated application tools to make ultrasound systems even easier to use.
Stroszczynski: We are also concerned with improving therapeutic procedures. In this respect, we can look quite confidently to the future, as preliminary evaluations over the last few years have showed that our patients would probably benefit from a significantly higher survival rate.