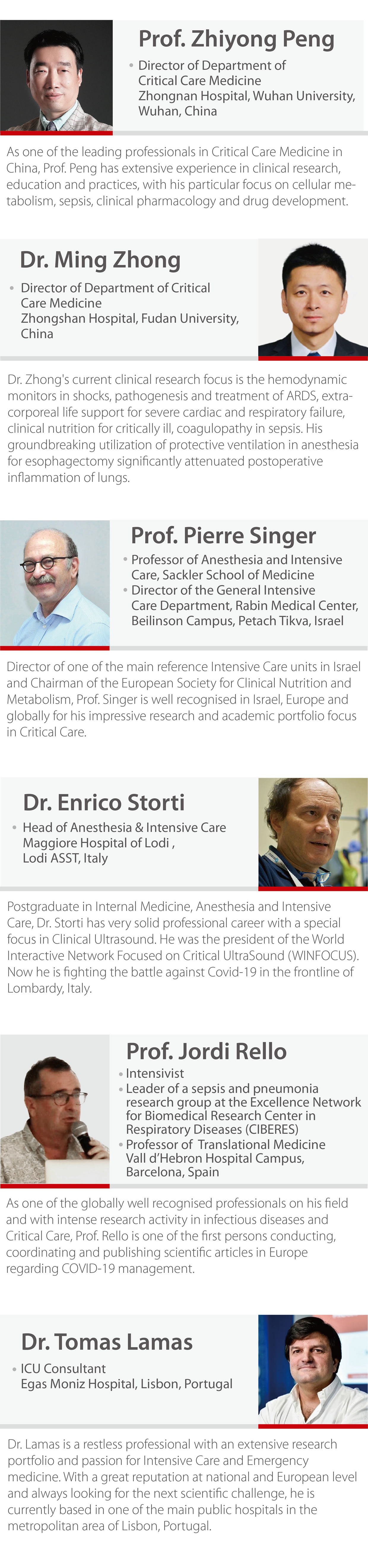
Q (Prof. Singer): What do you think about the comorbidities and the age of the patients in the treatment of COVID-19? Is the mortality higher in elderly patients as it is reported from recent papers?
A (Prof. Peng): If the patient has comorbidities, they can be easily infected by COVID-19 and are likely to become severe cases. Regarding the treatment, I am not aware of any specific treatment for this kind of patients.
Q (Prof. Singer): Regarding the organization and protection of the teams, what are your recommendations?
A (Prof. Peng): For the personal protection, implementing “airborne precautions” is crucial: N95 face masks, protective shoes, goggles and face shields when working in the ICU. This right protection for clinical staff is crucial.
Q (Prof. Singer): How many professionals have been infected?
A (Prof. Peng): Most of the professionals were infected at the early stage because we didn’t realize the transmission was so high. Another issue was that we didn’t have enough Personal Protective Equipment (PPE) at the beginning, but the government ordered many companies’ quick production of equipment. Right now everything is ok. During the last month I didn’t even hear about any case of professionals infected by COVID-19.
A (Prof. Storti): Regarding the questions from Prof. Singer, yes,
we have higher mortality among the elderly in Italy. Our experience is
limited to only three weeks and I don’t have clear figures, so please
don’t take this as truth. On the other hand, we are starting to see
younger patients severely ill with ARDS that, unfortunately, have to be
admitted in the ICU while, in the very beginning, we saw more elderly
patients.
How to protect our team is an issue. To give you a rough idea, we have
increased our ICU beds from 12 to 24. At the beginning, there was only
25% or less of our team members working because of a quite consistent
number of professionals out of duty as they were found to be positive
for COVID-19.
With smaller teams we are forced to cope with this situation by working
very heavy long shifts. Also, it is an issue to do extra shifts and when
you are deeply involved in a scenario which is totally unexpected and
unknown. I have seen many experts, ICU physicians and professionals
crying after their shifts.
To protect our professionals, we used N95 masks, goggles, hats, double
pairs of gloves and protective aprons. We, of course, also cover
shoes.
We ask our ID doctors to supervise our procedures in the “filter zone”
before the main entrance of the ICU. This “filter zone” was newly built
as it was not present before, all thanks to our technical guys.
A (Prof. Zhong): I was shocked by the number of critically ill
patients when I arrived in Jinyintan Hospital in Wuhan, the first
designated hospital to receive COVID-19 patients. They presented with
severe hypoxemia and Multiple Organ Dysfunction Syndrome (MODS).
Also, there was a lack of medical staff and we didn’t know whether our
personal protection was enough to keep us safe. The situation got better
when the physicians from all over China came to Wuhan to help local
professionals.
Q (Prof. Singer): Did you protect your teams by doing shifts? If somebody was infected and quarantined, how did you manage?
A (Prof. Peng): Of course anyone tested positive (abnormal chest
CT or typical symptoms) should leave the team and have a rest, and we
would recruit a new professional as other colleagues would be in risk to
be infected, even though they did not fear of the infected patients.
.
A (Prof. Zhong): There is a rotation (shift): one team every four
weeks and after that they have to leave and another new team will take
over. The professionals need, at least, one-week rest as working under
such pressure is exhausting. We needed more people for these shifts.
Q (Prof. Rello): What is the rotation of these shifts, 12 hours?
A (Prof. Peng): Yes, for physicians one shift is 12 hours.
Usually, in my team, we assign three physicians to each shift. In the
morning they need to stay on duty for 4 hours, then they can go out to
have lunch and some rest (even when not all of them will do it) and then
they rotate so there is always, at least, one physician keeping an eye
on the patients in the ICU.
A (Prof. Zhong): In the beginning, for the nurses one shift was
eight hours, but later we found that eight hours was too exhausting
because workload is much higher than standard, therefore they could not
keep working so long. Then, we shortened their shifts to 6 or 5 hours
with a higher rotation of shifts.
Q (Dr. Lamas): I have one question about the nurse shifts. After working for 5 or 6 hours, do they go back home and come next day, or they work 5 hours in the morning and then 5 hours in the evening? How do you manage these nursing shifts? We find very difficult to manage so many rotations.
A (Prof. Zhong): In our ICU, if the nurses have a 5-hour shift in the day time on the first day, on the second day they will have a 5-hour shift in the afternoon, and on the third day they will work at night. After that, they get a whole day to rest.
Q (Dr. Lamas): During the 5-hour shift, do you use the complete protective dress and equipment?
A (Prof. Zhong): To be honest, in the very beginning we were not very sure of what was the right protection working in such an isolation ICU, but we had the N95 masks, face shields and double gloves. For almost two months, no staff got infected.
A (Prof. Peng): I remember that the medical staff had to spend, at least, 4 hours in the ICU before going to the resting room to have some food or drink water. When they went back to the ICU, they must change and dress a whole new set of protective equipment. Therefore, in order not to waste protective equipment, they had to stay in the ICU for at least 4 hours before coming out.
Q (Dr. Lamas): What is the nurse-bed ratio and doctor-bed ratio in your ICU?
A (Prof. Zhong): My ICU was a temporary ICU. The former ICU had only 16 beds which were not enough and the temporary one expanded to 26 beds. During the first month, we had 50 nurses and 12 physicians. Now, we have 80 nurses and 15 physicians.
Q (Prof. Singer): About the equipment, having an increased number of patients who need mechanical ventilation, I guess you didn’t only have sophisticated ventilators but maybe also some simple ventilators? Are you using them?
A (Prof. Zhong): In our temporary ICU, every bed has a medicalized ventilator. We did not use home-use ventilators such as BiPAP. No matter whether they are for non-invasive or invasive ventilation, we all use the same ventilators.
Q (Moderator): We have a question from the audience. When the doctors and nurses finish their shifts, do they go home or stay at hospitals or any places nearby?
A (Prof. Zhong): At the hospital I support now, most medical staff come from other parts of China and don’t live in Wuhan, so the physicians and nurses will stay in hotels near the hospital between shifts. Even for the local professionals, most of them do not go back home after shifts. For those going home, they isolate themselves from their families.
A (Dr. Storti): In Italy, there are a number of physicians and
nurses who prefer being provided with some areas to stay rather than
return with their families. Personally, I haven’t seen my family for a
long while because we are deeply involved in an environment which is
highly infective.
We are dealing with two kinds of population. One group, of course, is
the ICU patients who may have ARDS or are on invasive mechanical
ventilation and we also take care of patients in a new Step-Down Unit
(SDU) of about 20 beds.
We arrange separate areas for the emergency department, and we are
weaning a large number of patients because we don’t have enough ICU
beds. We are trying to keep these patients alive and provide NIV for
them, but this kind of CPAP ventilation creates a scenario which is not
positive from the infection spread point of view.
Finally, we found another sort of worse scenarios with the huge
disproportion between resources and number of patients in the emergency
department, some of them very sick and demanding ventilation and
advanced monitoring and we can’t ventilate them properly because most of
the ICU ventilators are already on use.
Q (Dr. Lamas): I understand that using HFNC is very risky for the healthcare workers because there is a dissemination of virus in the air but, when you don’t have any available ventilators, then HFNC may the only option for these patients. Are you using it?
A (Dr. Storti): We do it. We try to ventilate and provide oxygen
to all patients, but it is not easy. Just a rough idea, we have
increased our oxygen consumption, in terms of source, too close to
“oxygen crash”, because the total amount of oxygen consumption is huge.
All the ventilators in ICU, SDU, and a large portion of medical beds,
every single patient, if not ventilated, is having any oxygen therapy.
Considering that, we have asked our technical guys to install twenty
220V oxygen sockets in the ER because there are not enough oxygen points
to connect to the patients.
To keep our patients alive, CPAP is useful in the ER while waiting for
SDU or ICU admission. It is not a gold standard, but that is the only
way to keep them alive and that is the reason why we are even more
committed to protect our staff, because they are still working in an
unsafe environment.
In the very beginning we tried to keep separate tracks for positive and
negative patients for COVID-19, but because of the outbreak, it has
become very difficult to achieve.
Q (Dr. Lamas): And how about in China, do you used high flow oxygen therapy?
A (Prof. Peng): Actually, we have similar issues. If most patients are on HFNC, the hospital will run off oxygen supply and we are also concerned about the airborne generated from the infected patients. Actually, we monitored the virus presence and concentration near patients in different environments of 2 ICUs: One ICU had its windows open, while the second ICU was equipped with negative pressure. We detected a higher virus concentration in the air on the first ICU, whereas on the ICU equipped with negative pressure, the virus concentration in the air was ok, so this ICU equipped with negative pressure was safer for professionals providing HFNC to their patients. Therefore I highly recommend that, if you want to use HFNC, do it in an ICU with negative pressure. This is better for healthcare professionals.
Q (Prof. Rello): Do you use any pharmacological prophylaxis to protect the healthcare workers?
A (Prof. Peng): There is no pharmacological prophylaxis. We just have PPE, hand hygiene and avoid cross-contact. These are all the important measurements for the professionals’ protection.
Q (Prof. Rello): If the healthcare workers become infected and cured, will they get infected again by the same virus?
A (Prof. Zhong): A: We observed some patients who were discharged
from the hospital having a negative test and some weeks later, they came
back to the hospital to be tested positive again. We don’t know whether
these patients got a second infection, reactivation or they just weren’t
completely cured after the first admission, but it is also important to
mention that we have seen some false negative tests.
We took samples from the mouth and throat, which were not deep, so we
were unsure whether it was because of the sample obtention that we had
false negative tests.
Q (Prof. Rello): The Lancet just published a very nice paper on mortality, It indicated and association of high Procalcitonin (PCT) and mortality. Does it mean that a high PCT would be criteria for prognosis?
A (Prof. Zhong): A: We are aware of the paper in the Lancet and, in my experience, we observed nearly 100 patients, and we did not observe the same association between the PCT and the outcomes. So, I don’t know if there is a relationship between PCT and the mortality due to COVID-19.
A (Prof. Peng): We also found that a high count of neutrophils and low count of lymphocytes predicted poor outcomes. Increased PCT levels probably indicates the secondary infection of the patients from bacteria or fungus, especially in the late stage of the illness, because these patients are in immunocompromised situations and can easily develop secondary infections.
Q (Prof. Rello): Regarding ventilatory strategies, here in Spain, we identified two different phenotypes: Some patients show a high pulmonary compliance, because they have a viral pneumonia and a severe hypoxemia. In the second phenotype, many patients were managed with delayed intubation, some of them with a high PCT that probably means over-infection, and the others were treated with delayed intubation like NIV. Do you document these two phenotypes in China and Italy? What are the implications of ventilatory management in these two phenotypes?
A (Prof. Peng): We observed that most of our patients had a low
pulmonary compliance. If the compliance level is less than 10 or 15
ml/cm H2O, it is not easy to wean them off the ventilators and it also
corelates to poor outcomes. For this type of patients, the lower
compliance, the poorer outcome.
I don't have any recommendations for ventilatory supports as any
ventilatory support may not work for this type of patients with very low
lung compliance.
Q (Prof. Rello): In Italy, did you see patients with high pulmonary compliance on viral pneumonia that require different ventilatory strategies? This is very important because, in the beginning, they are hypoxemic, and they get intubated very quickly but they don’t behave like ARDS but like a viral pneumonia. In my opinion, they need different ventilatory strategies like higher VT with lower PEEP and probably, prone position may not be required. What is your experience in Italy?
A (Dr. Storti): Though question. We received very ill patients
with hypoxemic blood gases that responded very well and quickly to
protective ventilation, meaning lower Tidal Volume and higher PEEP. The
PaO2/FiO2 improves quickly managing them with prone and supine
strategies, but the problem comes when you try to start the weaning
process. That is not so easy as they are still very weak, and present
all the problems associated to early weaning. I don’t know whether this
is a matter of ventilatory strategy or, as some colleagues believe,
during early ICU weaning after only one week, there is still a viral
burden still active in the alveoli and it takes longer to trigger the
inflammation response.
Sometimes, we also receive patients showing a clear ARDS pattern
confirmed by CT scan and lung ultrasound that we use extensively in the
ER and ICU as a bedside monitoring tool. Also sometimes we receive
hypoxic patients with not such ARDS patterns and, you are right, we need
to reshape a bit the ventilatory strategy according to this last
different pattern.
It is important to clarify that I am not so sure about all the details
of these patterns just because we have too many patients and it is
tricky to provide the same constant standards of care to 24 ARDS
patients together as it is an extremely time-consuming to focus on these
many patients at the same time.
I have no examples of these two patterns you mention for chest
compliance, lung compliance, but, obviously, the different patterns may
need to be ventilated in different ways. But again, in true ARDS, PEEP
shouldn’t be too high to protect them from pneumothorax. Anyhow when we
have scenarios where we are less experienced, we managed these patients
with the conventional protective ARDS strategy and maybe the compliance
you mentioned better correlates with what the CT scan tells us.
Q (Prof. Rello): In these patients with isolated viral pneumonia, with high pulmonary compliance and severe hypoxemia, probably the main finding is hypoxic vasoconstriction. In these patients, the major issue is indeed related to perfusion, as the lung is ventilated and increased PEEP may not help. Are these patients taking benefits from nitric oxide (NO)?
A (Prof. Peng): Actually, for this type of patients, if the lung compliance is less than 10 ml/cm H2O, it is not good. If the compliance is around 20 ml/cm H2O, we will try to help them by putting on prone position as soon as possible. Then we will proceed to very gentle lung recruitment manoeuvres that may improve lung compliance, just using a low PEEP, not higher than around 20 cm H2O, otherwise we can induce lung injury and pneumothorax. For the general settings we set the PEEP below 10 cm H2O for the lung-protective ventilation approach.
Q (Prof. Rello): Dr. Storti, any different comments on the use of NO to improve pulmonary perfusion?
A (Dr. Storti): Yes, we use it. Since we have more than doubled
our ICU beds, we also doubled the consumption of NO.
Sometimes we have a good clinical response, but sometimes they are
non-responders. But this is my personal approach, meaning that, when I
am not 90% or 100% sure, I always try to perform a NO trial and if I
manage to reduce FiO2, I’ll try to keep the NO on.
I am aware of the fact that the Chinese colleagues do not use NO because
we have discussed in the previous webinars
but I have a quite positive experiences with NO; if the patient
responds, I keep using it; if they do not respond, I suspend it.
Q (Moderator): We have a question from the audience about the NO use, since you are talking about it. What kind of patients do you think should be good responders to NO?
A (Dr. Storti): I don’t have an answer to that, anyhow the physiological
basics have been clearly described by Professor Rello and they seem
reasonable.
My questionable behaviour is very basic: when I see a high FiO2 that
already reached dangerous levels of pressure, I try to use NO in
addition. And then I try not to use high FiO2, but PEEP and driving
pressure to adjust the tidal volume to protect the lung.
Q (Dr. Lamas): We don’t have many ECMO machines, so how do you select patients for ECMO? And how do you manage the situation?
A (Dr. Storti): This is a tough question as in our hospital we
don’t perform ECMO, so we are forced to refer them to other hospitals.
From the beginning of this epidemic outbreak in the north of Italy, we
referred only a few patients for ECMO. Also, in some occasions we
proposed patients but, unfortunately, it was too late to bring them to
the ECMO network.
A (Prof. Rello): My personal opinion is that VA ECMO would be
very useful in a few patients who develop myocarditis. They would
benefit a lot. But we have a huge number of patients with hypoxemia and
it is not realistic to consider ECMO for all of them.
A (Dr. Storti): I do agree. If you are able to administer NO and
perform low-flow CO2 removal with CVVH, there should be a reduction of
patients in need for ECMO.
A (Prof. Peng): Actually, in my hospital we have already
performed ECMO on 15 patients, and the mortality is around 50%.
When and how to initiate ECMO is a very important step as, from our
experience, if a patient has a high CO2, it probably means that there is
also a severe lung injury and this kind of patients cannot be easily
weaned from the ECMO. So, if a patient is on severe hypercapnia, they
probably won’t be easy to wean from the ECMO. Also, the elderly and
those with several comorbidities will not be easy to be weaned from
ECMO.
As our experience is limited to only 15 ECMO, I don’t know if there are
any differences with other virus-induced pneumonias or ARDS and maybe
the mortality is similar or lower to other ARDS. Nowadays the survival
ratio of H1N1-induced ARDS should be around 60%, but I'm not sure if we
can extrapolate these results to COVID-19 as we only had 50% of
survivors after ECMO.
A (Prof. Zhong): In our centres, in the beginning, we didn’t have
enough nurses/physicians-bed ratio so, for some patients it is possible
that there was a delay to start ECMO. These patients had a long-time
mechanical ventilation before the ECMO. Anyhow we managed to stabilize
the vital signs but, as Prof. Peng mentioned, they were very hard to
wean from ECMO. In some cases, even the inflammation and pneumonia were
gone, but the lung compliance was still low, and these patients couldn’t
recover to a normal lung, even after more than one month on ECMO, and
they died due to the consequence of the ECMO support.
In my opinion, if we have not enough medical resources, we must select
patients for ECMO very cautiously avoiding those that have been on
mechanical ventilation for too long as well as the ones with many
comorbidities.
In conclusion, we have observed that ECMO effect is not as good for
COVID-19 patients as we expected based on previous experiences.
Q (Prof. Rello): Two additional questions with regards to specific populations: Pregnant women and children. In pregnant, do you manage it differently during the third trimester?
A (Prof. Peng): In my hospital, we admitted about 40 pregnant
women infected with the COVID-19 and most of them had mild to no
symptoms, even the chest CT showed just mild changes. From these, at
least 10 women delivered the baby already, and we didn't find any
evidence of vertical transmission from mother to foetus.
I also tried to understand what happens to pregnant women by comparing
them to non-pregnant women of the same age but, unfortunately, it is
difficult to find non-pregnant women on the same age who are ill from
COVID-19, only a few and most of them are nurses.
I tried to collect some data from the community of infected patients and
I couldn’t find anything relevant, but I still think that pregnant women
are vulnerable to the COVID-19, so I would recommend extra care even
they don’t show any symptoms.
Q (Prof. Rello): What about immunocompromised patients? And what about children? Because looking at the reports, initially the main target was elderly people, but later on younger people joined.
A (Prof. Peng): Actually, I haven't seen any children infected
with the COVID- 19 in my hospital, but perhaps they are in the
children’s hospital.
For immunocompromised patients such as organ transplantationor under
chemotherapy, radiotherapy, of course, they may be vulnerable to the
COVID-19. I saw some of them and the evolution depends on their clinical
story: if these patients are still at the early stage of the organ
transplantation or chemotherapy, they can become severely ill. Other
patients with an organ transplanted one or two years ago would be
alright or show mild symptoms.
Q (Moderator): I would like to ask something from the audience. Did you observe if these patients are more likely to get a nosocomial infection in the hospital?
A (Prof. Peng): I didn't find any differences from other patients. Maybe the nosocomial infection is more likely to happen in a more advanced stage, not in an early stage, especially if the patient stays in the hospital for a long time.
Q (Moderator): But you didn't notice a difference with other patients’ populations, right?
A (Prof. Peng): No, I didn't find any differences from other populations. The lymphocyte level and severe lymphopenia depend on their situation, as ICU patients are very ill but in the wards, they are less ill.
Q (Moderator): That takes me to other question from the audience related to these “less ill” patients: Is there any experience of treating them at home or a different place other than hospitals?
A (Prof. Peng): Asymptomatic patients are requested to stay at
home on quarantine but, unfortunately, in China now most of the
apartments have only two bedrooms and it is difficult for them to
maintain the quarantine and they easily infect other family members.
That was a big issue in early stage from Wuhan and that's why so many
people were infected, because they got it from their family.
We opened a temporary hospital because we had not enough space to put
those patients on quarantine, besides of the fact that I am not sure
they would follow or obey the physicians’ commands.
So, no treatment for the mild and asymptomatic patients, just stay at
home, hotel or the temporary hospital.
Q (Moderator): Controversial question from the audience about the treatment. There is a new publication in NEJM about potential treatment with lopinavir and ritonavir. What is your experience with that? Do you think this is something that may work?
A (Prof. Peng): Regarding the treatment, there's still not enough
evidence to show which kind of medication would work against the
COVID-19.I know the paper was just published yesterday for the lopinavir
and ritonavir, and it didn't show enough evidence of benefit from RCT.
Also, we need to be careful with lopinavir and ritonavir because it may
easily induce cardiac injury and bradycardia.
A (Prof. Rello): My personal opinion is that we need to
differentiate patients that show “influenza-like” illness, patients who
develop pneumonia, and patients who develop ARDS, and we need to be very
careful to avoid adverse events by doing things that are not based in
solid evidence. Also, for instance, these drugs have plenty of
interactions with drugs that we use in the ICU.
I fully understand that physicians want to try but we need to be
vigilant to avoid adverse events and pharmacological interactions that
make the patient’s management more difficult and even can put healthcare
workers in risk.
In line with other experts in Italy and the US, I believe that these
patients should be left quiet: SARS is not influenza, and SARS is not
ARDS! We need to avoid “doing too much” at any cost as it is of higher
benefit than “only doing nothing”. This is just my personal opinion; do
you support it after your experience in Italy?
A (Dr. Storti): First of all, I think that it is important to
exactly define what is the lung involvement and I think that CT scan
does the job as it is the gold standard. But also, lung ultrasounds are
very useful, especially if you compare it with a chest X-ray instead of
a CT scan. Ultrasounds can be useful in terms of looking at how the
lungs are moving, how the lungs are interacting with the ventilator and
how the lungs are changing with different PEEPs and ventilators’ set
up.
Regarding the therapy, I personally have no figures as we are generating
them now. We managed to be involved in in a trial which seems to be very
promising, but by now we have only a few cases so, statistically, they
don't mean anything.
I was asked to manage 45 patients, to date the largest population that
might be tested in Italy, but I still didn't receive the drug, so my
study is not feasible at the moment. Anyway, I think that to have clear
figures about treatment and drug effectivity, it is too early as there
isn’t strong evidence about what drug/-s we should choose?
A (Dr. Lamas): Regarding the PCR test to diagnose COVID-19, we
are having many false negatives even when we see some patients
presenting the typical symptoms and are highly suspicious because of the
CT scan images, their lymphopenia pattern and other evidences.
We had one patient that tested positive only on the 3rd PCR test when
all the evidence was clear, and this is very stressful as we don't know
if we can decrease the level of protection if this patient is on an ICU.
Therefore, my first question is how many PCRs on the same patient are
you performing to make sure about the correct result?
And the second question is if there is any useful blood test based in
Immunoglobulin M and Immunoglobulin G as we see many companies offering
them, but I am not any confident that using these tests is going to help
us to manage these patients.
A (Prof. Rello): Regarding the PCR tests, I think that we need to
adopt the same approach that we followed with influenza as this is a
virus that has a special affinity for lower respiratory tract. For
example, if you have a pregnant patient with a consistent presentation
of influenza pneumonia and the nasal swab is negative, you will not
change the approach and treat her for influenza pneumonia.
COVID-19 shows a very characteristic presentation with high C reactive
protein, low PCT, lymphocypenia and, in severe cases, intubation and
mechanical ventilation. When you take a nasal or throat swab from this
patient and the result is negative, that may happen because the viral
burden is low, because there may be a problem with the test, or a
problem when transferring the sample to the lab… and this is why I
believe that we have to follow the same approach we adopt for influenza
management and continue with the same management.
Also, and despite inconsistent test results, I wouldn't recommend to
perform bronchoalveolar lavage (BAL) as we have to give priority to the
healthcare workers safety.
A (Prof. Peng): I totally agree with you. The PCR sensitivity is
only 40% to 50%, which is not good enough, anyhow you can try
consecutive times.
On the other hand, just imagine that you could detect the antibodies in
a blood test. That would be the best way to help you detect whether the
patient is infected or not. If the patient’s antibody levels are high
then, definitely the patient is positive in the COVID-19, therefore you
can combine these two tests.
If your patient shows the typical symptoms, the typical chest CT scan
and also the elective flu tests, then we set the clinical diagnosis to
COVID-19, even without the positive virus PCR test.
A (Prof. Zhong): I agree with Professor Peng and maybe the
antibody test may help to diagnose these patients.
If we have a patient that was negative for PCR test, but positive for
the antibody test as well as for the IgM and IgG, it gets very difficult
to explain why the PCR is negative. Maybe its sensitivity is not enough
for a relative low amount of virus? So, we must be very cautious with
these negative results as we don't know whether these patients, upon
hospital discharge, will spread the infection. Maybe the antibodies test
would help.
A (Dr. Storti): We experienced that here, in the north of Italy,
some hospitals ended up fully collapsed just because they were waiting
for swab determination kits, which are showing a very poor sensitivity,
especially with the “negative” results as they don't mean anything. I
can support this idea because some of my physicians presented fever,
coughing and the typical symptoms, and after two negative PCR tests and
10 hours, they got a highly “susceptible” positive CT scan.
It is an issue to adopt this as the determination test in Italy as there
could be several problems when obtaining the sample, as for example,
those associated to the operator management and sample manipulation.
Also, in our ICU community in Italy, to confirm a negative test, we rely
on sample aspiration from the lower respiratory track rather than just
the nasal and throat swabs.
Also, following our Chinese colleagues’ advice, we will start tomorrow
the IgG and IgM determination in combination with the other tests.
Anyhow, my opinion is not to combine but select a different system, but
unfortunately, this is not easy because what our government and health
care system are requesting is not to use IgG and IgM determinations to
confirm tests.
A (Dr. Lamas): By combining IgM and IgG determinations, perhaps
we can increase diagnosis’ sensitivity together with CT scan and
lymphopenia and then the picture would make more sense for us. It is
quite difficult to manage low resources when trying to separate
COVID-negative from COVID-positive patients to manage them, and that's
why, as a doctor, I don’t feel very confident about negative tests as we
always keep some suspicion of having false negative results.
Q (Moderator): It is great that we had discussed quite a lot about healthcare professionals’ safety and protection during this meeting and, in line with that we have another question from the audience: are there already any available figures of COVID-19 mortality within the healthcare professionals?
A (Dr. Storti): I think that the mortality in Italy now is pretty
high, but I'm not sure that an accurate calculation would be feasible
now, as I do not fully rely on the swab tests and I am sure that we are
underestimating the positive population, therefore the mortality is
difficult to be calculated.
Here, I heard that at least two healthcare professionals died: one was
in the pre-hospital emergency services and the other one was a hospital
nurse, but luckily, the number among professionals is very small.
Q (Moderator): I forward this question now to our Chinese participants, what is your experience regarding to mortality within the healthcare professionals?
A (Prof. Peng): Currently we really don't know the mortality
figures among medical professionals. I just know that some physicians
and nurses died during this outbreak, but I don't know the official
number. Also, I am not aware of the total number of healthcare
professional infected.
A (Prof. Zhong): Neither am I aware of these figures. I think
there should be some publications about the results and maybe we can see
the mortality in these papers, but I am not sure.
In different kinds of population groups, they present different
mortality rates. As said before and in my experience in the ICU, when
the more ill patients progressed to a very severe situation, the
mortality rate on this group is very high, even higher than ARDS
patients from other cause.
Also, we know that the asymptomatic, mild and moderate populations are
the larger proportion of the COVID-19 patients. Within this population I
have treated colleagues and the outcomes were good.
A (Prof. Rello): Mortality figures typically show up 18 days
after illness onset. So, in Europe we cannot still estimate that, at
least from Spain we cannot provide any reliable information.
The Expert Dialogues is initiated and organized by Mindray in the interest of the healthcare community to combat COVID-19. Thanks to the contribution of all the panelists who join in the discussion voluntarily with no conflict of interest.
