Personalized and Continuous Hemodynamic Management
Optimum oxygen delivery as the goal:
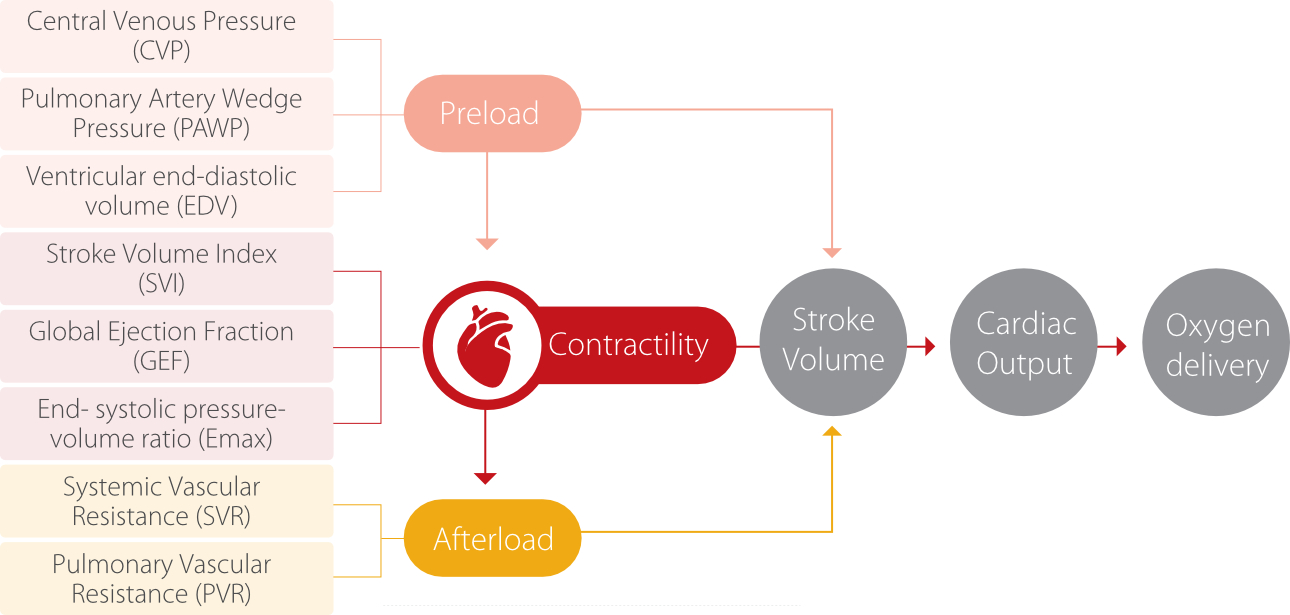
The purpose of hemodynamic monitoring is to maintain proper perfusion and oxygen delivery, and to assure oxygen supply-consumption balance by clinical intervention of hemodynamics [1].
Oxygen delivery is realized by blood movement within the circulatory system, and the main monitoring parameter is cardiac output (CO). The decisive elements of cardiac output are cardiac preload, cardiac afterload and myocardial contractility (Figure 1).
Personalized continuum of care:
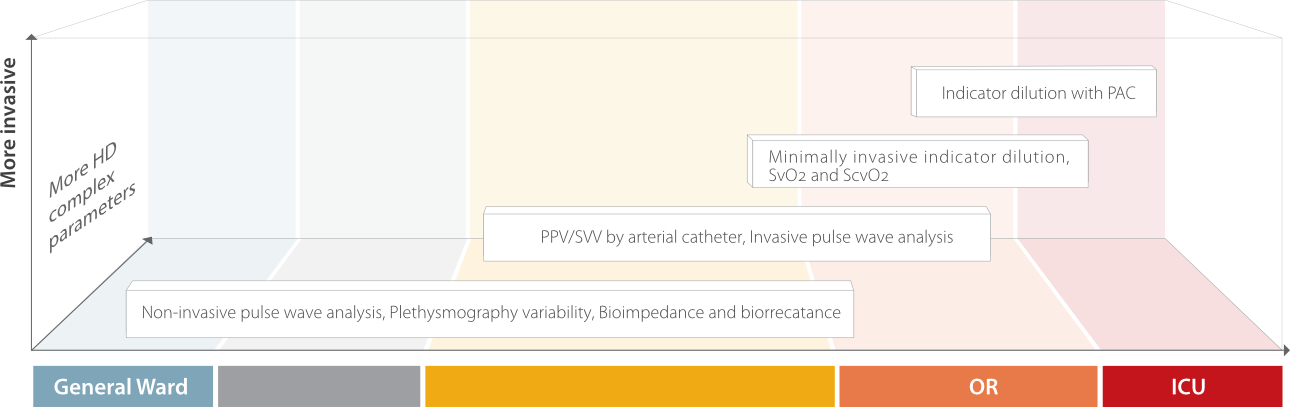
Now we know that mortality within 30 days after surgery is up to 1000 times higher than intraoperative mortality [3,4], and multiple solutions have been proposed to tackle the clinical and economic burden of postoperative complications which leads to death [5]. Among them, one of the most important components is the optimal fluid and hemodynamic management of patients undergoing major surgery. In different stages of hemodynamic therapy, the monitoring method and intensity may differ according to the dynamic status of the patient (Figure 2). This is why personalized hemodynamic management of the patient at every stage of the perioperative process (not only intraoperative) may lead to better outcomes [4,5].
As the technology develops, hemodynamic monitoring is not only useful to reflect patient’ s hemodynamic status, but also to find the initial causes and/or disease outcomes by analysing the groups of related hemodynamic parameters that enable practitioners to understand more details of the patient care process [6].Therefore, an adequate management guided by effective and timely hemodynamic monitoring can help reduce the risk of complications and thus potentially improve outcomes along the care
pathway for each different patient [6,7].
Patients’ diversity, levels of care and hemodynamic monitoring methods:
When it comes to hemodynamic monitoring, there are now many different systems available, and caregivers need to choose among multiple possibilities according to their demands. These systems can be listed in the order of degree of invasiveness, from the highly invasive pulmonary arterial catheter (PAC) to less invasive transpulmonary thermodilution and pulse contour analysis, and completely non-invasive bioimpedance/bioreactance technology.
Decisions of using which method and when to use it are usually based on two main factors: 1. invasiveness of the monitoring procedure
and its associated risk; 2. the required accuracy level of the obtained hemodynamic parameters.
In order to obtain comprehensive clinical information, a certain level of invasiveness may be considered. On top of that, there is an increasing demand to minimize the risks entailed, so deciding how invasive the monitoring procedure is should be challenging in certain settings (e.g. perioperative). Therefore, it is important to understand the measurement principles and indications of the invasive, minimally invasive, and non-invasive methods available for hemodynamic monitoring, so that the optimal cardiac output monitoring method can be chosen for the individual critically ill or surgical patient [8].
Combining and integrating parameters from various hemodynamic monitoring systems may help improve the understanding of hemodynamic status [9]. For example, a hypotensive patient with a low cardiac output will present different diagnoses, and correct treatment involves consideration of many factors (hypovolemia, decreased contractility or obstruction) and hence require different treatments to a hypotensive patient with a high cardiac output [9].