In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
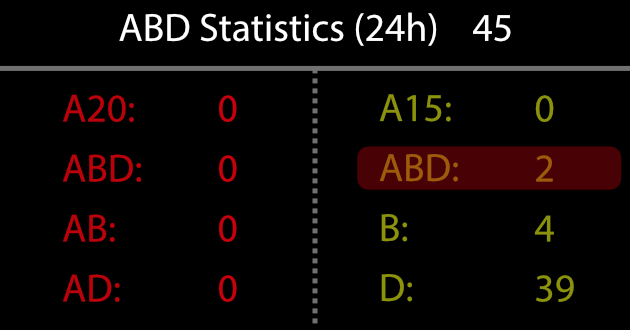
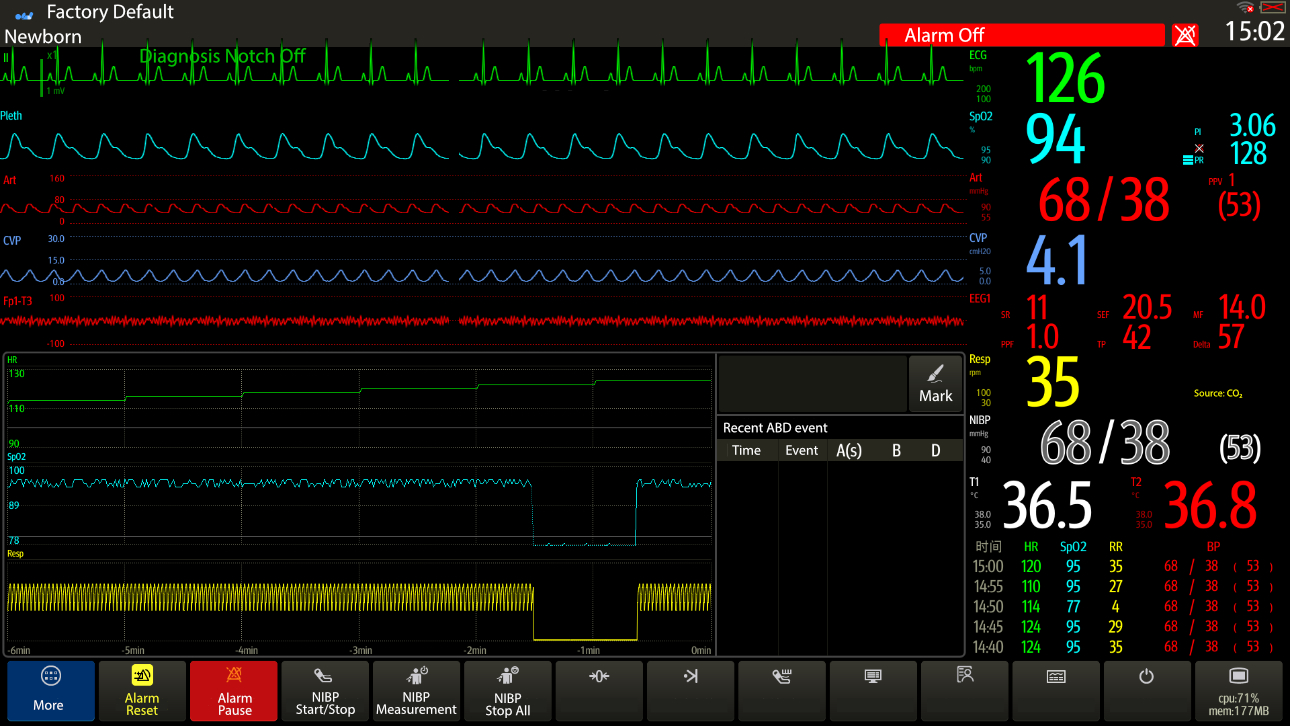
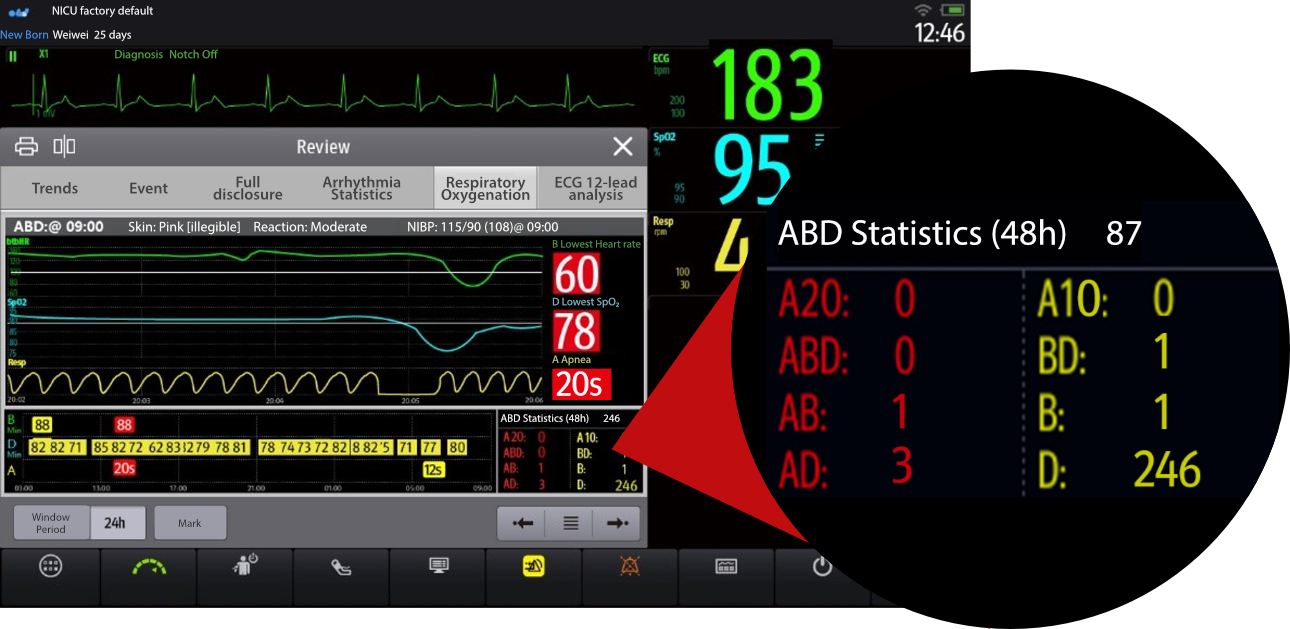
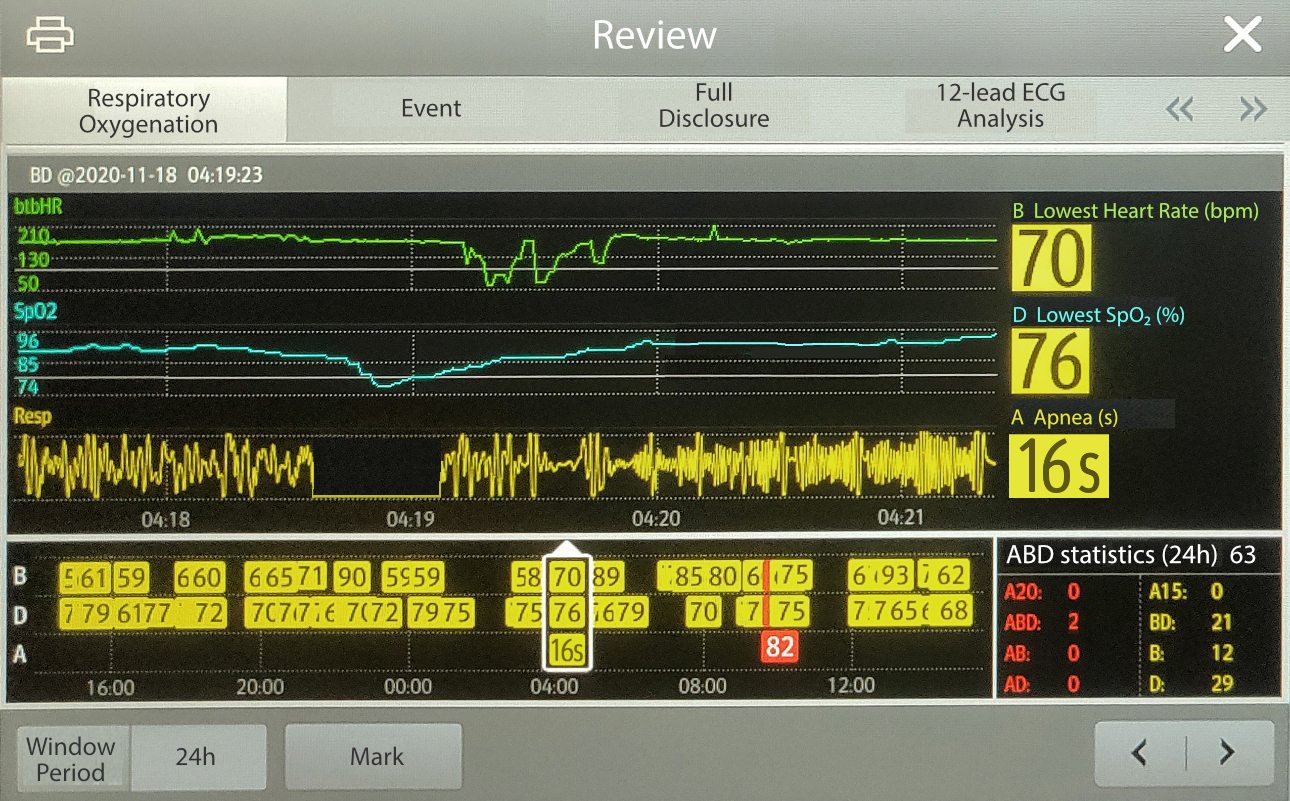
Preterm infants are extremely prone to hypoxia, while apnea and bradycardia are usually accompanied by hypoxia. Doctors need to determine the cause of hypoxia, such as distinguishing cardiogenic hypoxia and respiratory hypoxia, so as to provide targeted treatment regimens. Respiratory oxygenation chart function (ABD A: Apnea ≥10 s; B: Bradycardia <100 bpm; D: Desaturation, i.e.
SpO2 <80%) can assist in the analysis of changes and frequency of other parameters that accompany hypoxia in patients. If the patient
experiences an ABD event simultaneously, the following judgment can be made based on the order in which the events occurred: If bradycardia is followed by desaturation, it may be a cardiogenic hypoxia event; if apnea occurs first, followed by a desaturation or bradycardia, apnea event caused by respiratory disease or a central disease may be considered. (As shown in Figure 1)
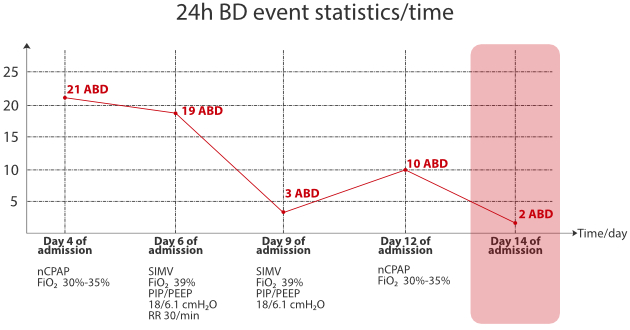
Secondly, the statistics of the number of corresponding events within 24hrs, such as the increase and decrease of the same combination of events within 24hrs, also play an important role in the assessment of the patient’s disease progression and treatment effect. (As shown in Figure 2)
Case Introduction
The patient was a boy born at a gestational age of 30 weeks to a gravida 5, para 2. He was admitted to the hospital due to “his mother’s severe preeclampsia, HELP syndrome, and scarred uterus, as well as two prenatal fetal monitoring, showed no response and fetal growth restriction”. His birth weight was 1,040g, the Apgar score was 9 points at 1 min, and 10 points at 5 mins and 10 mins, respectively. After birth, the patient groaned and had slight shortness of breath, and was given nCPAP assisted ventilation.
Initial assessment of the status of the patient after admission to the department
Under the assistance of non-invasive ventilator in the incubator (nCPAP mode, with the parameters of FiO2 30% and PEEP 6.0 cmH2O), the SpO2 fluctuated between 90-94%. The patient’s skin has mild yellowing and the shortness of breath was relieved. His
three-concave sign was weakly positive, the breath sounds in both lungs were symmetrical without rales. However, his muscle tone of all four limbs was relatively low.
Results of the first auxiliary examination after admission for the patient
Hematology test:
WBC 7.73*109/L; NEUT% 61.9%; LYM% 23.1%; HGB 183 g/L; HCT 60.6%; PLT 133*109/L; CRP 4.39 mg/L.
A bedside radiograph of the chest and abdomen showed:
The translucency of bilateral lungs decreased diffusely, and air bronchogram sign was observed.
Preliminary Diagnosis
- Preterm infant
- Neonatal respiratory distress syndrome (NRDS)
- Very low birth weight infant Small for gestational age
Progression
After nCPAP was given to assist ventilation, FiO2 was set to 24%, PEEP 6.0 H2O, and symptomatic and supportive treatments were given as well. The patient’s status was recorded for 11 consecutive days (i.e., Day 1 to Day 11 after birth) to track how the respiratory oxygenation function could assist in the assessment of the patient’s oxygenation status and treatment effect.
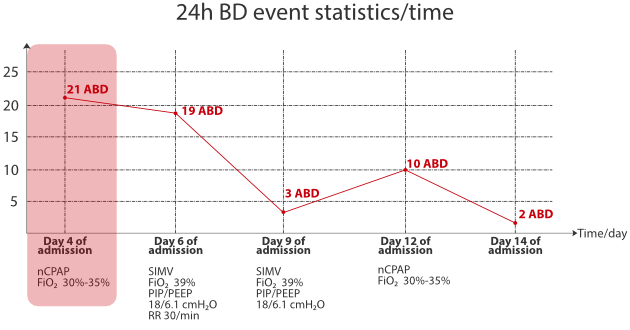
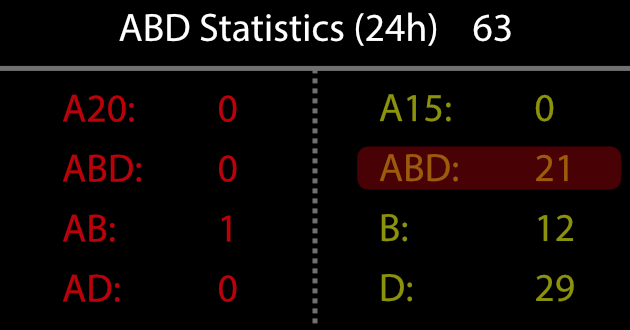
After treatment the patient’s condition gradually stabilized, and symptoms of dyspnea such as shortness of breath and three-concave sign was significantly relieved. The respiratory oxygenation function showed 6-8 ABD events occurred every day. On Day 4 of admission, the patient suddenly experienced frequent apneas, and the respiratory oxygenation chart function suggested that the patient experienced a total of 21 times of desaturation with bradycardia within 24hrs.
Through the respiratory oxygenation trend, it was shown that apnea is first accompanied by desaturation at the time of each ABD event, then followed by bradycardia. Considering that respiratory apnea causes ABD events to occur frequently, medical staff instruct nurses to increase inhaled oxygen concentration based on SpO2 (FiO2 30% increased to FiO2 39%), and the SpO2 was ultimately maintained between
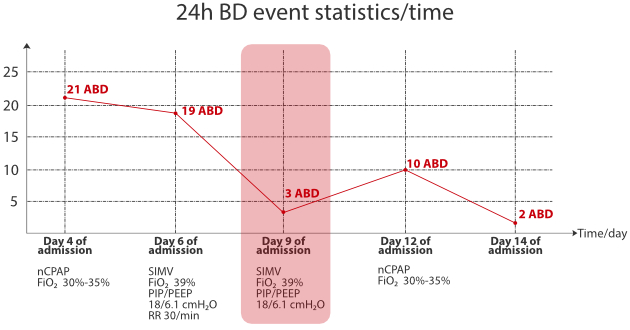
88%-95%. Given that the harmfulness of high-concentration oxygen therapy, the concentration of inhaled oxygen was not increased for the time being. Prior treatment was maintained, the changes in the patient’s condition were closely observed, and special attention was paid to the frequency of ABD events. (As shown in Figure 3)
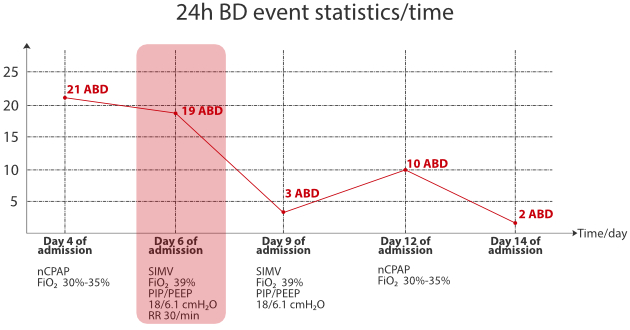
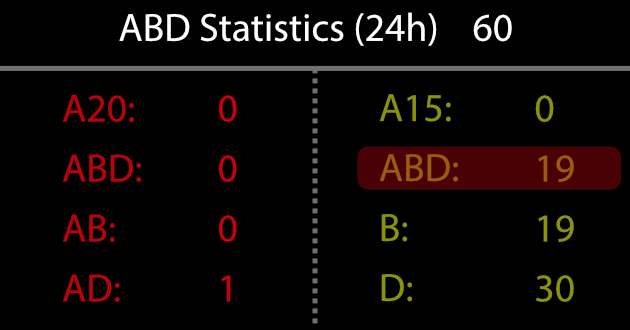
On Day 6 of admission, as the patient still experienced 19 ABD events and could only recover after skin irritation, meanwhile, another chest radiography was performed and revealed new patchy shadows. Upon combining with other laboratory indicators, the patient’s condition was considered aggravated. In this case, intubation was performed for invasive ventilation, and the parameters were set as SIMV mode, FiO2 39% PIP/PEEP 18/6.1 cmH2O, RR 30 breaths/min. Other treatment regimens were co-administered, and changes in the patient’s condition were closely observed.
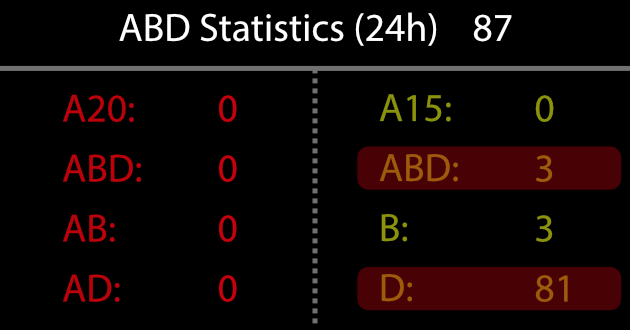
On Day 9 of admission, it was discovered through the respiratory oxygenation chart function that the number of desaturations with bradycardia events of the patient decreased significantly, and the number of ABD events was reduced from 19 times per 24hrs to 3 times per 24hrs, but the number of desaturation events was more than before (D event: 81 times within 24hrs and desaturation could recover spontaneously.)
The doctor analyzed that the ABD event was significantly reduced compared to before, suggesting that the patient’s condition was improved.
Although the number of independent desaturation events was increased, most of them were transient and could recover spontaneously. Combined with a comprehensive assessment of the patient’s manifestations and status, and considering that the treatment at that time was effective, in order to reduce the risk of complications caused by invasive ventilation, the existing ventilation mode was downgraded and switched back to nCPAP assisted ventilation.
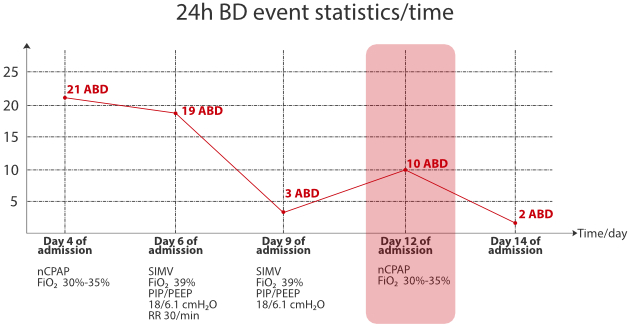
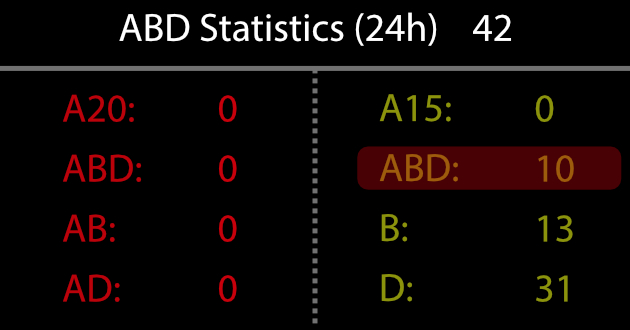
On Day 12 of admission, the number of ABD events was increased, and it occurred 10 times within 24hrs. Clinically, the reason for the increase in ABD events was actively investigated, and the time of weaning from mechanical ventilation was delayed.
The doctor on duty found that the desaturation with bradycardia was caused by acid reflux, so the breastfeeding method was changed to pumping.
It could be seen that on Day 14 of admission, after the feeding method was changed, the number of patient’s ABD events decreased to 2 times which was significantly improved than before, indicating the symptomatic treatment was effective.
After the patient was treated effectively and his condition remained stable, he was switched to high-flow nasal cannula therapy (Flow 4L/min, FiO2 21%-23%), and he was able to maintain stable SpO2 spontaneously and his condition was significantly better than before. No apnea and desaturation occurred again, and the patient was weaned from mechanical ventilation after three days of high-flow nasal cannula therapy. Discharge was arranged after the vital criterias were met after birth.
Summary
Newborns, especially preterm infants, suffer from frequently occurring desaturation due to undeveloped physiological systems or other pathophysiological reasons. Clinically, it is necessary to find out the correct cause of the disease, such as respiratory, central, and cardiogenic, in combination with changes in other physiological parameters and the time sequence of their occurrence when there is desaturation. At present, the clinical assessment of respiratory oxygenation events is mostly based on nursing records and the independent observation of the doctor in charge as the main method to assess changes in a patient’s condition. However, the current method is prone cause to problems such as incomplete manual recording, difficulty in reviewing information, and laborious statistical data, which greatly restricts the effective and accurate assessment of respiratory oxygenation events by medical staff.
Based on this clinical need, the Mindray Monitoring System provides a respiratory oxygenation chart function for the NICU department, and it automatically monitors the occurrence time and type of frequency of different types of events according to industry standards. It also provides a review function for each event to help medical staff to clearly and intuitively understand the respiratory oxygenation status of newborns, so as to make an accurate diagnosis and treatment decisions.
For example, in this case of the patient with NRDS, the occurrence of bradycardia secondary to respiratory hypoxia further affected the perfusion and oxygenation of the patient. Therefore, the doctor selected the ABD combination event as the assessment topic with the use of the Mindray Monitoring System's respiratory oxygenation chart function to regularly assess the condition and treatment efficacy of the patient (such as whether it is necessary to change the ventilation mode, ventilation parameter settings and weaning time selection, etc.), and good results were obtained.
Appendix
[1] Clinical Associations of Immature Breathing in Preterm Infants: Part 1: Central Apnea
Karen Fairchild, Mary Mohr, Alix Paget-Brown, Christa Tabacaru, Douglas Lake, John Delos, Joseph Randall Moorman and John Kattwinkel
Published in Pediatr Res 2016 Jul;80(1):21-7. doi: 10.1038/pr.2016.43. Epub 2016 Mar 9. PMID: 26959485 PMCID: PMC5015591 DOI: 10.1038/pr.2016.43
[2] Accurate Automated Apnea Analysis in Preterm Infants
Brooke D. Vergales, MD1, Alix O. Paget-Brown, MD1, Hoshik Lee, PhD2, Lauren E. Guin, BS3, Terri J. Smoot, RN3, Craig G. Rusin, PhD3,6, Matthew T. Clark, PhD4, John B. Delos, PhD2, Karen D. Fairchild, MD1, Douglas E. Lake, PhD3,5, Randall Moorman, MD3, and John Kattwinkel, MD1
1Division of Neonatology, Department of Pediatrics, University of Virginia, Charlottesville, Virginia
2Department of Physics, The College of William and Mary, Williamsburg, Virginia
3Department of Internal Medicine, University of Virginia, Charlottesville, Virginia
4Department of Chemical Engineering, University of Virginia, Charlottesville, Virginia
5Department of Statistics, University of Virginia, Charlottesville, Virginia
6Division of Cardiology, Department of Pediatrics, Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas
Published in final edited form as: Am J Perinatal. 2014 February; 31(2): 157–162. doi:10.1055/s-0033-1343769.