Specialized Applications of Ultrasound Machines
02-10-2026

Clinicians rely on ultrasound machines for diagnostics, monitoring treatment effectiveness, and assessing various conditions. Real-time sonography imaging is a powerful tool across specialties, ranging from women's health to cardiovascular care and beyond.
The Expanding Role of Ultrasound in Hospital Settings
Ultrasound imaging has become an integral part of healthcare settings, from doctors' offices to the Intensive Care Unit (ICU). While these machines are often associated with obstetrics, they play a much larger role in specialized medical diagnostics. Ultrasound machines have become more common across healthcare facilities for their notable benefits, such as:
- Safety: Ultrasound technology uses sound waves to generate real-time images and does so without contrast agents. This imaging technique removes the risk of radiation and eliminates allergic reactions to contrast dyes
- Noninvasive nature: Clinicians can perform ultrasound exams without breaking the skin, making it a preferable option for the patient. The acoustic transducers only need to make contact with the skin to generate images
- Simple to use: Ultrasound systems are often considered user-friendly, making them accessible for clinicians and quick to use during emergencies
- Detailed and dynamic imaging: Unlike X-rays and other imaging modalities, ultrasound imaging can capture soft tissue in great detail and in real-time. This characteristic makes them valuable for specific diagnostics, like assessing organs and musculature, or for procedural guidance
- Accessibility: Ultrasound systems are accessible for healthcare facilities and only involve one consumable product, the water-based gel
Key Specialized Ultrasound Applications
Ultrasound technology has many specialized use cases.
Women's Health
Women's health applications are among the most well-known use cases for ultrasound technology, particularly pregnancy. During fetal development, an ultrasound allows obstetricians to assess the fetus as it grows. While these images can be exciting for parents, they can also help clinicians monitor the blood flow and heart health of the baby.
Regular ultrasound exams can lead to early detection of childbirth issues, such as breech, allowing for timely intervention. Ultrasound imaging also supports estimations of delivery dates based on fetal development.
Beyond pregnancy, ultrasound technology is used in gynecology for routine pelvic exams, diagnosing gynecological conditions, and monitoring ovarian health. For example, 10 in 100 women have ovarian cysts, which can cause symptoms like abdominal pain and torsion that cuts off blood flow to the ovary. Ultrasound exams can identify the size and type of cyst to determine if surgical removal is necessary.
Ultrasound imaging can also be used in OB-GYN cases to evaluate fertility, assess for uterine and ovarian cancers, and help to identify endometrial cells.
Point of Care Ultrasound (POCUS)
Unlike traditional ultrasound modalities, POCUS brings the system to the patient and not the other way around. This differs from traditional ultrasound diagnostics where the imaging is interpreted at a later point by a radiologist, cardiologist, and the patient's healthcare provider. POCUS helps clinicians answer questions about a patient's condition, guide procedures, and rule out diagnoses. The point of care can be anywhere, including hospital beds in emergency rooms, on ambulances, at the site of an accident, and more.
A common application of POCUS is in the emergency department. If a patient comes in with trauma injuries, clinicians can use a POCUS machine to rapidly detect the presence of free fluid (most often blood) in key body cavities, including the peritoneal, pericardial, and pleural spaces (FAST exam). Clinicians assess POCUS imaging on the spot, so the technology is straightforward and designed for portability.
Musculoskeletal
Historically, conventional radiography (X-ray) was the first-line imaging modality for evaluating musculoskeletal (MSK) complaints — particularly cases of recurring or chronic pain that were not emergent. X-ray remains useful for detecting bone abnormalities such as fractures, joint dislocations, and degenerative changes, but its limited soft-tissue contrast often results in missed or inconclusive findings for muscle, tendon, and ligament injuries.
MRI has become the gold standard for assessing musculoskeletal damage due to the excellent soft-tissue contrast and multiplanar detail. However, the high cost and limited accessibility of MRI imaging make it unattainable for underinsured and uninsured patients.
Modern diagnostic ultrasound has transformed musculoskeletal imaging by providing real-time, high-resolution visualization of soft tissues. Clinicians use ultrasound imaging to evaluate tendon integrity, muscle tears, joint effusions, bursitis, and nerve entrapments. This technology can also be used for monitoring chronic inflammatory and degenerative conditions, such as rheumatoid arthritis.
Ultrasound technology can be a more accessible diagnostic tool for clinicians, and it plays a role in guiding therapeutic procedures, such as joint injections, aspirations, and soft-tissue interventions. These use cases support improving treatment outcomes.
Vascular and Cardiovascular
Ultrasound systems allow clinicians to assess the vascular system in real time. Imaging can reveal enlarged arteries, stenosis, blood clots, and the condition of varicose veins. From these ultrasound images, clinicians can determine when surgery is necessary and where medications may be needed to manage conditions, such as deep venous thrombosis. Ultrasound imaging can also be used to assess blood flow to the brain to identify tumors, aneurysms, and hemorrhages.
In cardiovascular cases, ultrasound imaging has become a critical player in evaluating heart health at the point of care and for at-risk patients. Symptoms such as shortness of breath and chest pain can indicate a heart attack, but not always. An ultrasound of the heart offers more diagnostic specificity to determine the root of these symptoms. For example, a cardiovascular ultrasound can help clinicians diagnose global cardiac dysfunction, cardiac tamponade, and pulmonary embolism.
Early detection of conditions like pulmonary embolism enables clinical teams to prevent cardiac arrest, which can be fatal. In the event of cardiac arrest, ultrasound systems can also guide resuscitation and compressions with the measurement of cardiac activity.
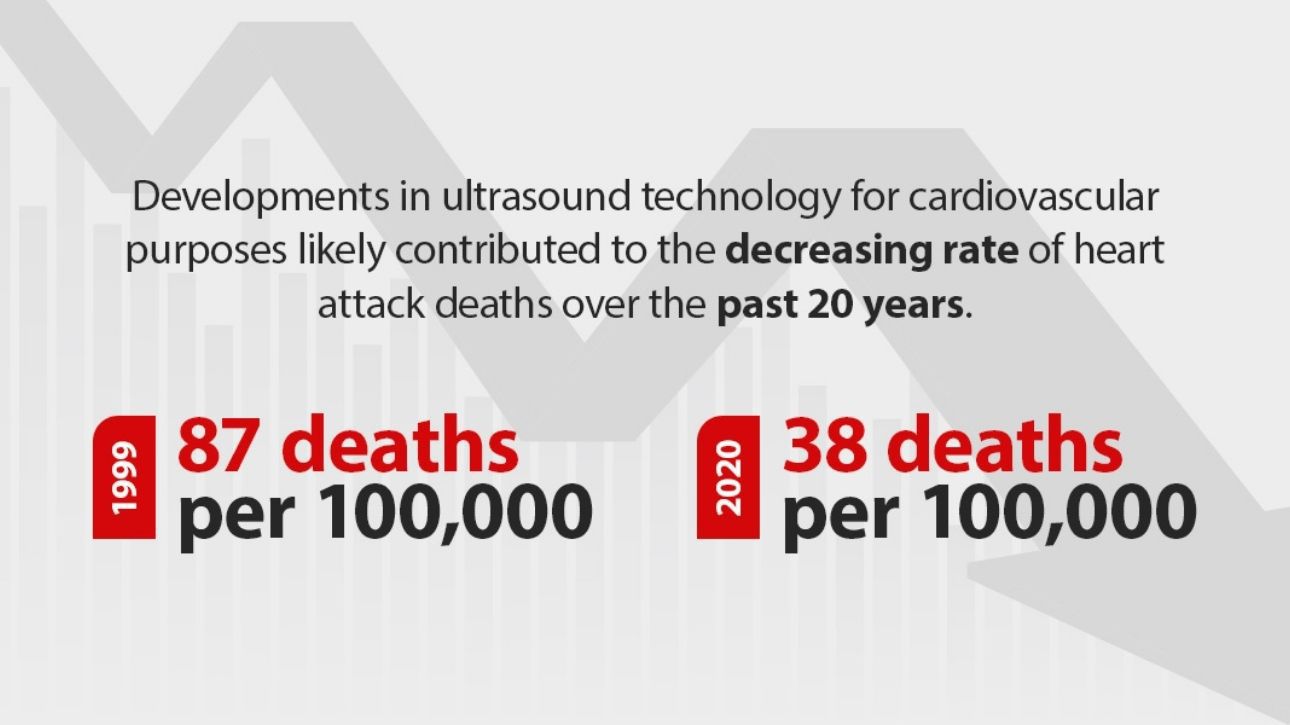
Developments in ultrasound technology for cardiovascular purposes likely contributed to the decreasing rate of heart attack deaths over the past 20 years. According to the American College of Cardiology, heart attack deaths dropped from 87 deaths per 100,000 people in 1999 to 38 deaths per 100,000 people in 2020.
Liver and Kidney Care
Ultrasound machines excel at visualizing soft tissue structures, making them invaluable tools in both liver and kidney care. In hepatic applications, ultrasound enables clinicians to assess and monitor conditions such as hepatitis, fibrosis, steatotic liver disease, and focal lesions with precision and without radiation exposure. Similarly, renal ultrasound is used to detect injuries, identify kidney stones, evaluate blood flow, and monitor urinary tract health — providing a safe, efficient, and noninvasive method for ongoing diagnosis and management.
Advancing Technology for Ultrasound Diagnostics
The rise of ultrasound technology in healthcare requires advancements in technology for user-friendliness and tools designed for clinical efficiency and confidence. At Mindray North America, some of our core advancements include:
- AI integration: Modern ultrasound systems account for the increasingly complex clinical environment with AI tools. Smart technology integrated in systems like the TE X Ultrasound System can support fast nerve identification, precise fluid management, seamless fetal heart rate calculations, and more
- Portability for POCUS: As more clinicians rely on POCUS in emergency departments and beyond, ultrasound machines incorporate simple designs and portability. The TE Air Wireless Handheld Ultrasound System is pocket-sized and can be brought to a patient almost anywhere outside the hospital. Other systems, like the TE7 Max Ultrasound System, are designed for greater maneuverability to easily reach the patient's bedside.
- Enhanced imaging: Advanced imaging technology strengthens resolution quality and tissue uniformity. The Resona A20 Ultrasound System is the future of radiology, featuring Acoustic Intelligence Technology (AIT)™ for consistently sharp, diagnostic-quality images.