A New Approach for Patient Ventilation at Salford Royal

A New Approach for Patient Ventilation at Salford Royal
In 2023, Salford Royal Hospital procured a new fleet of non-invasive ventilators to improve the speed and quality of ventilation outside of the respiratory support unit (RSU). The RSU was set up in response to the second wave of the COVID-19 pandemic. It combines the specialties of Acute Medicine and Respiratory Medicine so enhanced respiratory support can be safely delivered outside of the critical care environment. In the UK COPD exacerbations are the second most common cause of emergency hospital admissions, accounting for 1 in 8 UK hospital admissions. A 40% increase in COPD prevalence is projected and an annual cost to the NHS of £2.5 billion by 2030 is predicted. [1]
On top of dealing with the usual flow of referrals for specialist respiratory care, the RSU’s outreach team spent a lot of time supporting set-up of the ventilators in other departments and troubleshooting user errors. This meant treatment was sometimes delayed and made staff reluctant to ventilate, instead, referring patients to the specialists at the RSU. The Trust wanted to make it easier for other departments to provide NIV independently so patients received the right ventilation care as quickly as possible, especially as a new trauma unit was about to increase capacity.
The next step in collaboration
Salford has been working with Mindray since 2017 when the modular BeneVision N Series monitors were installed. This provided continuous patient monitoring during transport and brought the Trust one step closer to paperless working. Since then, the Trust has been standardising with Mindray, including the use of M-Connect for large-scale connectivity projects on the horizon.
Salford Royal Hospital is one of four hospitals within the Northern Care Alliance NHS Foundation Trust, providing care services to the City of Salford and specialist services to Greater Manchester and beyond. Today it has 9,000 dedicated staff and more than 700+ in-patient beds including a 40-bed ICU, and 25 operating theatres. In 2024 the hospital opened a brand-new dedicated trauma centre that aims to receive 90% of all major trauma patients in Greater Manchester.
Why NIV?
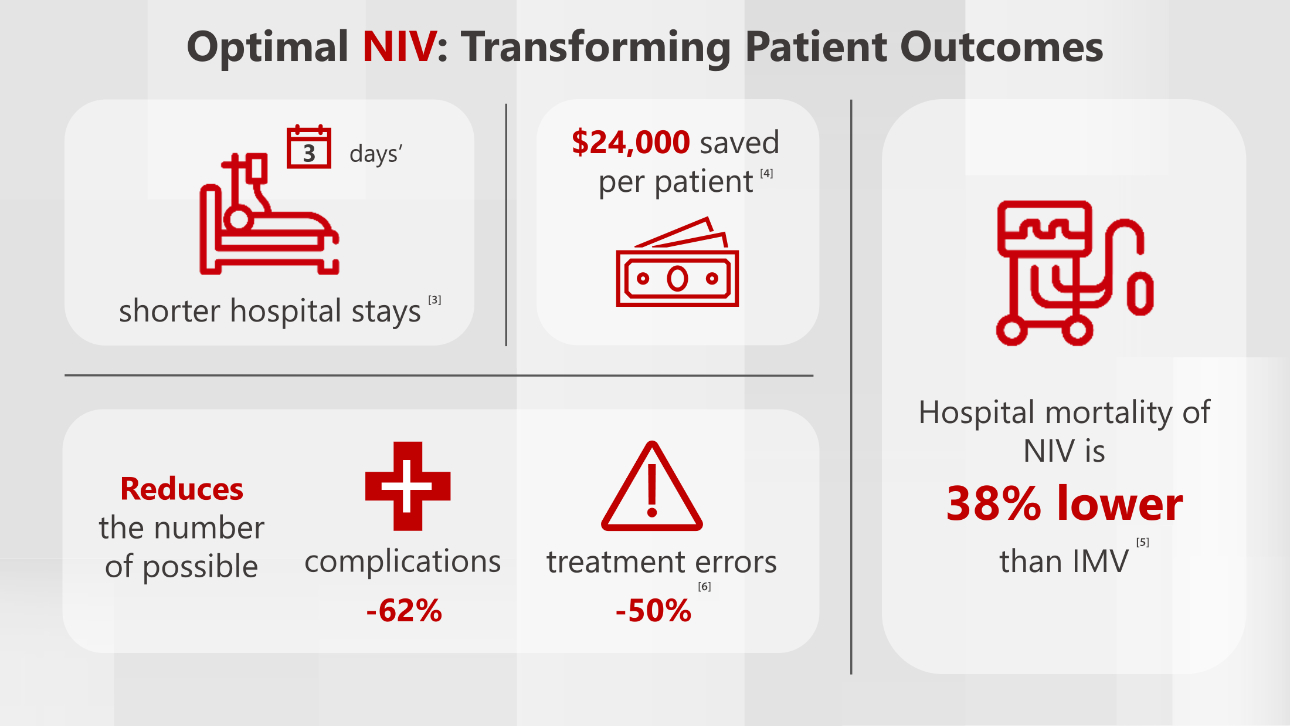
Non-invasive ventilation (NIV) has gained popularity because it provides ventilation to the patient without using an artificial airway and does not bypass the upper airway. [2]
NIV has become a common treatment for acute and chronic respiratory failure, especially in patients with chronic obstructive pulmonary disease (COPD). In comparison with invasive ventilation, NIV tends to reduce the rate of intermittent mechanical ventilation (IMV), procedural complications, and mortality.
In cases of acute respiratory distress syndrome (ARDS), using NIV could help avoid complications associated with IMV such as ventilator-associated pneumonia and barotrauma.

Challenges
- COPD prevalence – Respiratory disease affects one in five people and is the third biggest cause of death in England. [7] Salford deals with a higher proportion of COPD cases than the national average and ventilation is provided quickly. 26% of COPD patients received NIV within 2 hours of arrival, compared to the national average of 16% (2021-2022). [8]
- Managing workload – There has been sustained high demand on the RSU outreach team who want to continue seeing COPD patients quickly. In 2021-22, 86% of COPD patients were seen by a member of the respiratory team within 24hrs of admission compared to the national average of 60%. [9]
- Versatile ventilation – the ventilators would be used in a wide range of treatments in multiple departments so patients can be managed outside the RSU, where appropriate, to ensure spaces are used for the most critical cases.
Standardisation: the ventilators needed to be compatible for digital integration, and to streamline internal training.
Solutions
- Increasing capacity: Salford procured a new fleet of non-invasive ventilators to improve the speed and quality of ventilation outside of the respiratory support unit (RSU).
- NIV on demand: The SV70 is user friendly even for non-RSU staff who do not use ventilators every day. To reduce the risks of user error, the main menu has been configured to show the two most appropriate ventilation modes – ST (spontaneous timed) and CPAP (Continuous positive airway pressure).
- Faster treatment, greater comfort: Intuitive visualisation tools support faster treatment and reduce the number of manual interventions needed for patient comfort and treatment.
- More insights for safer decision-making: trend data is available on the SV70 ventilator for more comprehensive respiratory assessment. This is especially useful for assessing the levels of overnight machine breathing for neuro-patients in the morning when discussing cases with physios.
- Responsive Care: Compatibility with the Mindray Central Stations means the SV70 will fit into Salford’s digitalisation plans which will make patients’ pressure and oxygen stats available even when away from the bedside.
SV70 in the RSU
Gary Dawson is a Respiratory Nurse Specialist at Salford Royal Hospital. He was instrumental in expanding the hospital’s NIV provision.
“The SV70 is one of the easiest to use systems I’ve come across. When our staff need a ventilator, it’s the first device to get used on the ward.
“After covid, we wanted to get ventilators that were easier to use so clinicians working outside of the RSU could still deliver the right ventilation at the right time. We’ve seen more patients presenting with respiratory illnesses so it's critical we manage the in-flow effectively.
“The SV70 has worked well in a wide range of scenarios. For instance, we’ve seen a lot of motor-neurone disease (MND) patients recently and the ventilators have synchronised with them easily. On the other end, where we’ve had to use high pressure to flush out CO2 for smokers’ lung, intubation and synchronisation is just as easy.
"Patients are getting the right ventilation faster in departments like A&E, and the RSU team is receiving fewer alarms and call-outs due to user error.
Gary Dawson
Respiratory Nurse Specialist at Salford Royal Hospital
The trend data from the SV70 gives us valuable insight that we haven’t had before. We can pick up average pressures and review patient breathing through the night which is extremely useful for neuro-patients where we want to see how much breathing has been done by the machine. The SV70 provides the advanced data that specialists need, but it’s equally as easy for a nurse to quickly check things like SpO2, EPAC, PEEP and plateau pressure.”
Elevating Care for High Acuity Patients
- Higher throughput: the RSU team have been able to cope with a higher number of patient referrals to the RSU within the last year. Although Summary Hospital-level Mortality Indicator (SHMI) data is not a direct indicator of quality of care, it shows that during June 23 – May 24 there were fewer deaths across the Northern Care Alliance for COPD, bronchitis and respiratory failure, than for the previous period. [10]
- The right treatment, faster: ventilators are being used far more frequently outside of critical care, especially in A&E. Patients get the right treatment faster before going to the RSU.
- Fewer errors: the RSU outreach team have had fewer callouts to support ventilator set-up and correct user error, making more effective use of their time.
- Streamlined care: Standardising with Mindray has simplified training, and staff have found the SV70 easy to use. Nurses feel confident to change pressures or adjust masks if needed, delivering responsive care even outside the RSU.
Fit for the Future
Following sustained pressure on respiratory services, Salford Royal Hospital have used the SV70 to administer NIV more effectively outside of the RSU. Clinical staff have found the device easy to use, while specialists have easier access to historic ventilation data to better inform clinical decision making.
To advance healthcare even further, Salford is developing integrated wireless interoperability. This would allow patient data to be collected from multiple bedside devices, such as the SV70 ventilator and N Series monitors, and automatically updated on nurses’ stations and electronic patient records (EPRs). This will reduce administration and allow clinicians to see the latest patient data no matter where they are for fast and confident clinical decision-making.
References:
[1] https://transform.england.nhs.uk/key-tools-and-info/digital-playbooks/respiratory-digital-playbook/digital-service-to-manage-high-risk-chronic-obstructive-pulmonary-disease-copd-patients/
[2] Bello G., De Pascale G., Antonelli M. Noninvasive ventilation. Clin Chest Med. 2016;37(4):711–721. [PubMed] [Google Scholar]
[3] Hamadziripi N, Gale N, Hopkinson JB. Experiences of noninvasive ventilation in adults with hypercapnic respiratory failure: a review of evidence.Eur Respir Rev. 2016;25(142):451-471. doi:10.1183/16000617.0002-2016
Warren DK, et al. Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical center. Crit Care Med. 2003; 31(5):1312-7. (PubMed)
[4] Costs of Ventilation Options Derived from nThrive® Database – Retrospective Database Analysis Journal of Trauma and Critical Care, Issue 3, page 4 https://www.alliedacademies.org/articles/costs-of-ventilation-options-derived-from-nthrive-database--retrospective-database-analysis.pdf
[5] Crit Care Expl 2020; 2:e0128
[6] Ferrer M, et al. Non-invasive Ventilation during Persistent Weaning Failure. Am. J. Respir. Crit. Care Med. 2003; Vol. 168, No. 1:70–76. (PubMed)
[7] https://www.england.nhs.uk/ourwork/clinical-policy/respiratory-disease/
[8] (Source: https://ncab.hqip.org.uk/reports/list/units/rm301/all/)
[9] (Source: https://ncab.hqip.org.uk/reports/list/units/rm301/all/) Data covering April 2021 - March 2022; from the Drawing Breath report 2023 published 12/01/2023. National aggregate for England & Wales. More up to date data may be available at: https://www.nrap.org.uk/
[10] https://digital.nhs.uk/data-and-information/publications/statistical/shmi/2024-10 / 2023-2024 data, p6: https://app.powerbi.com/view?r=eyJrIjoiZGNlMDgwMGEtNGZlNi00ZjJlLWI5MzItNWYyZDFiYTI0ZDAyIiwidCI6IjM3YzM1NGIyLTg1YjAtNDdmNS1iMjIyLTA3YjQ4ZDc3NGVlMyJ9





