Special thanks to: Ru Yanhui, Sheng Xuan, Yin Hong, Department of Ultrasound of Shandong Maternal and Child Health Hospital, Medical Imaging Center of Shandong Maternal and Child Health Hospital.
The levator ani muscle is believed to be an important support for lower urinary tract function and pelvic organ. In recent studies, it is shown that major levator trauma happens in 15–35% of vaginally parous women, when using Magnetic Resonance Imaging (MRI) and transperineal ultrasound for the diagnosis[1,2]. The main methods of clinical assessment of levator trauma include transvaginal palpation, MRI, and pelvic floor ultrasound. Generally speaking, MRI has limitations such as cost and accessibility, and the fact that the imaging is static, not dynamic [3]. Pelvic floor ultrasound, on the contrary, has the advantages of shorter examination time, more economic, real-time display, intuitive and multi-plane display of the levator trauma location, etc. It has become an increasingly important method to assess levator trauma.
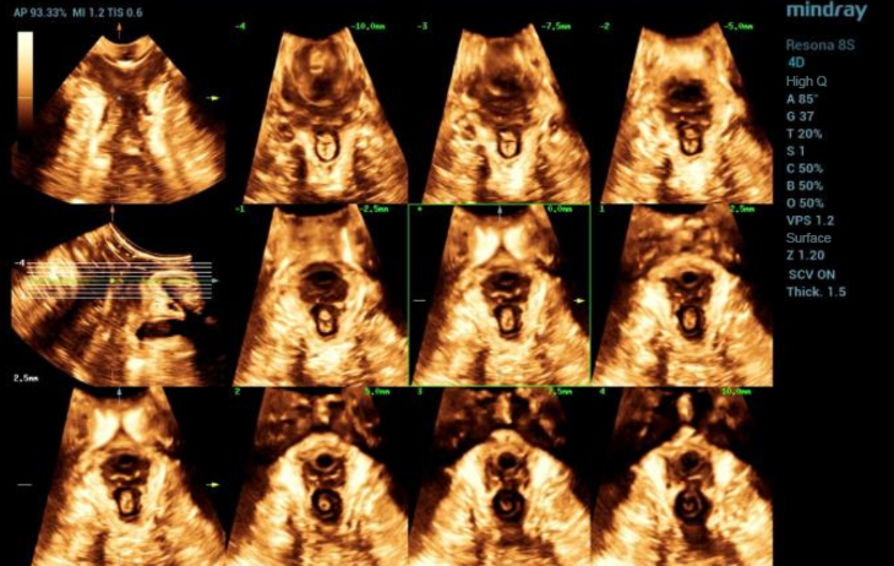
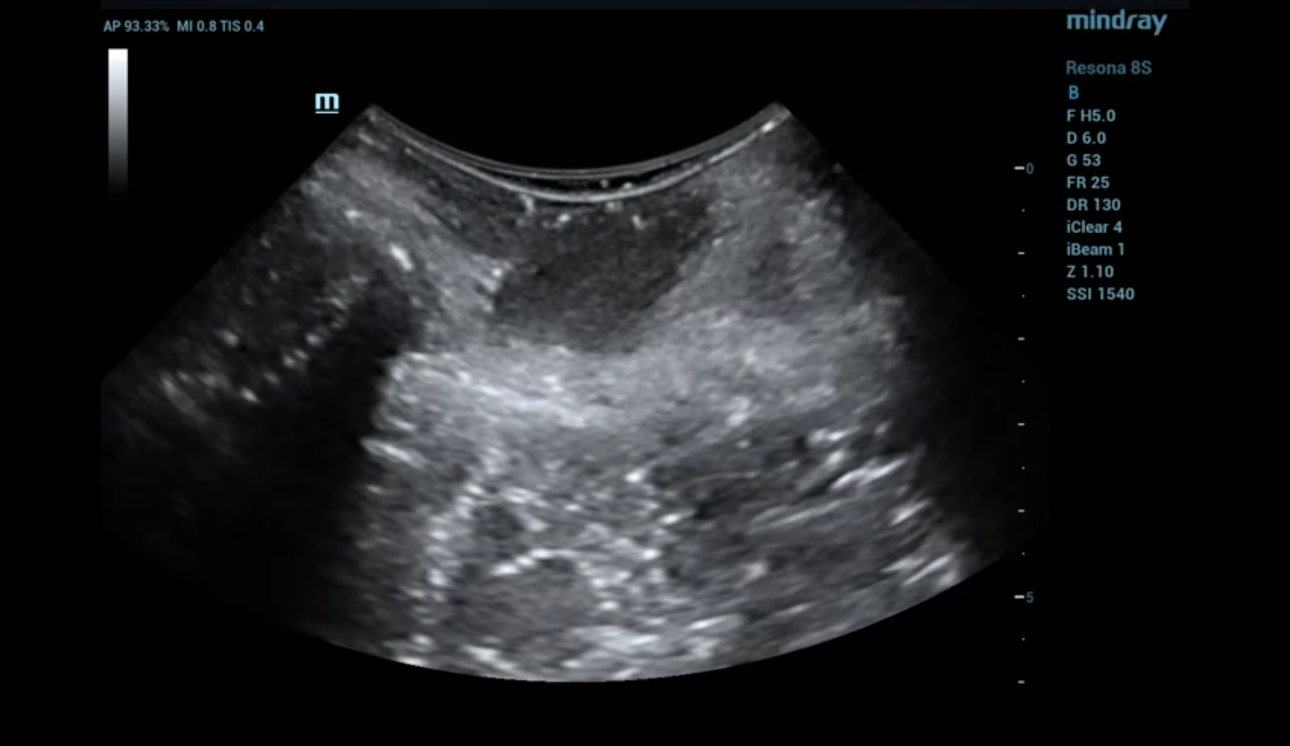
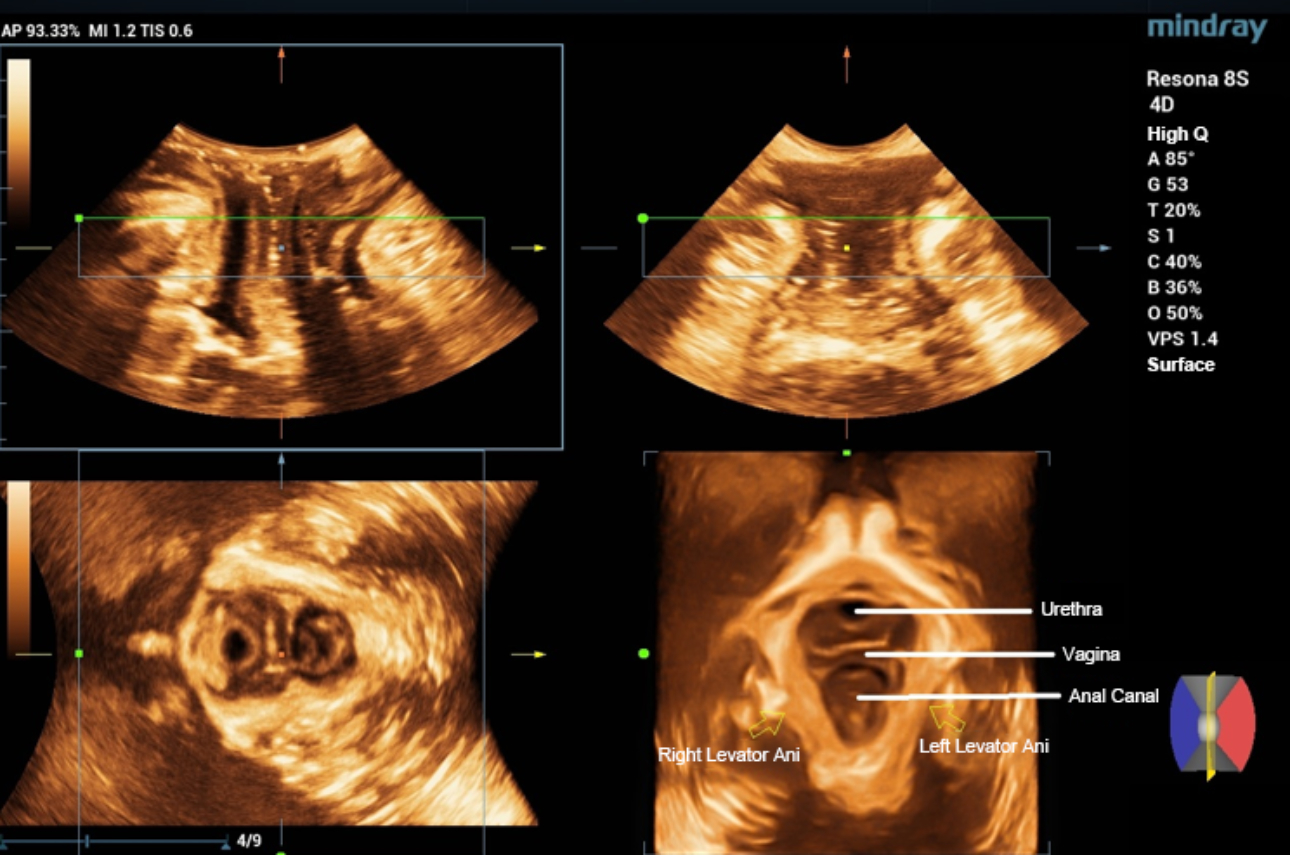
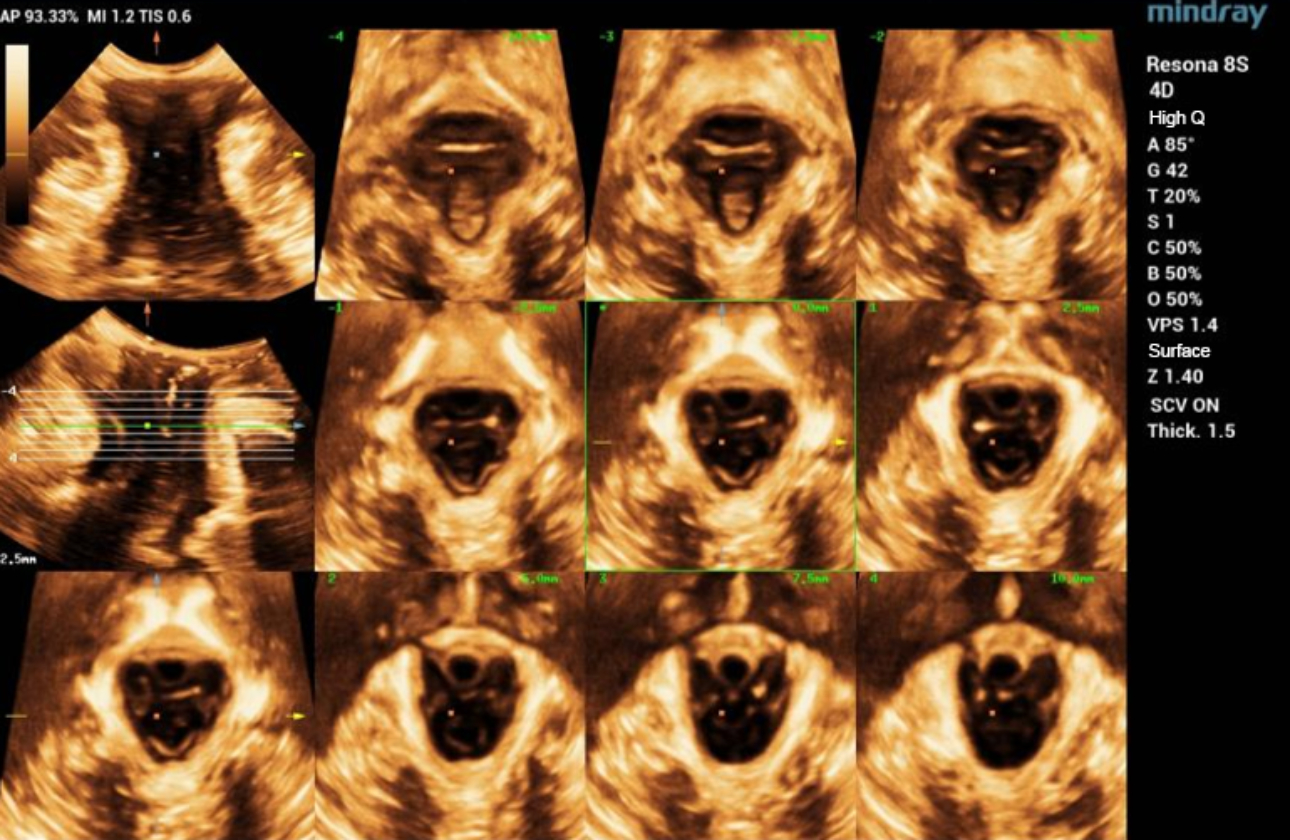
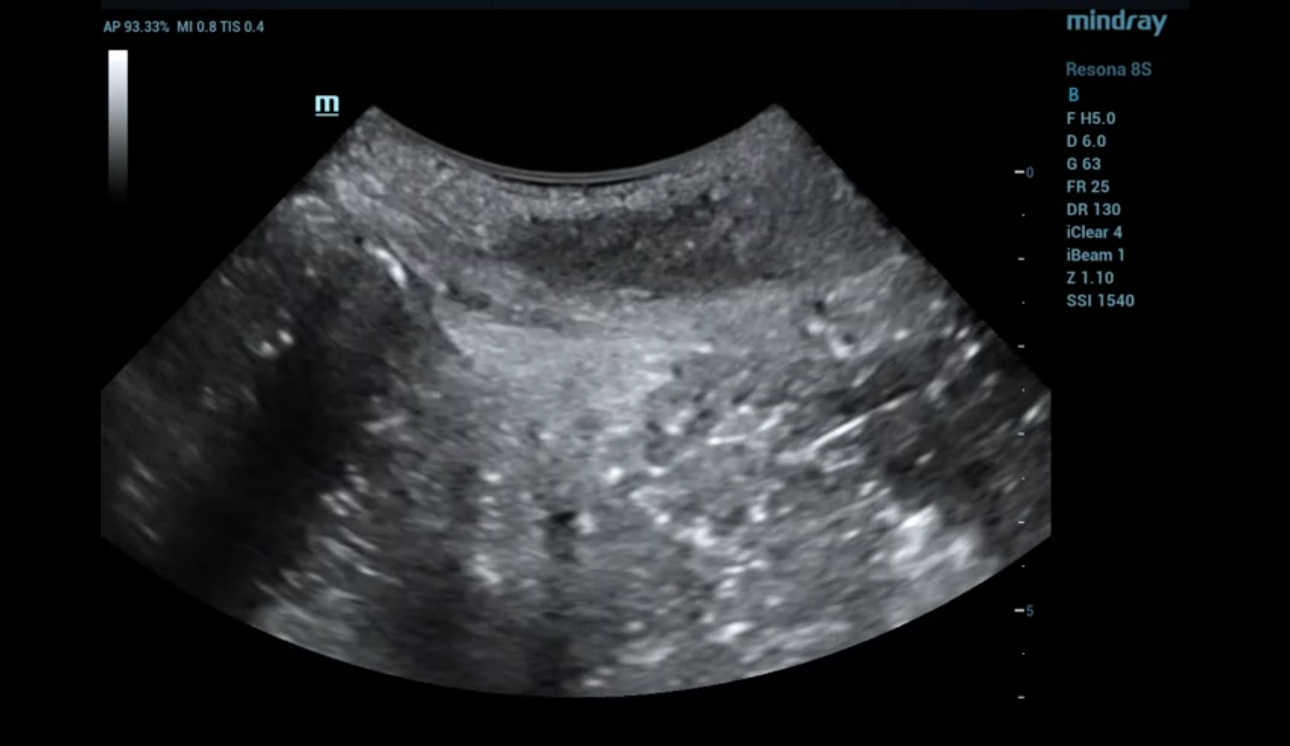
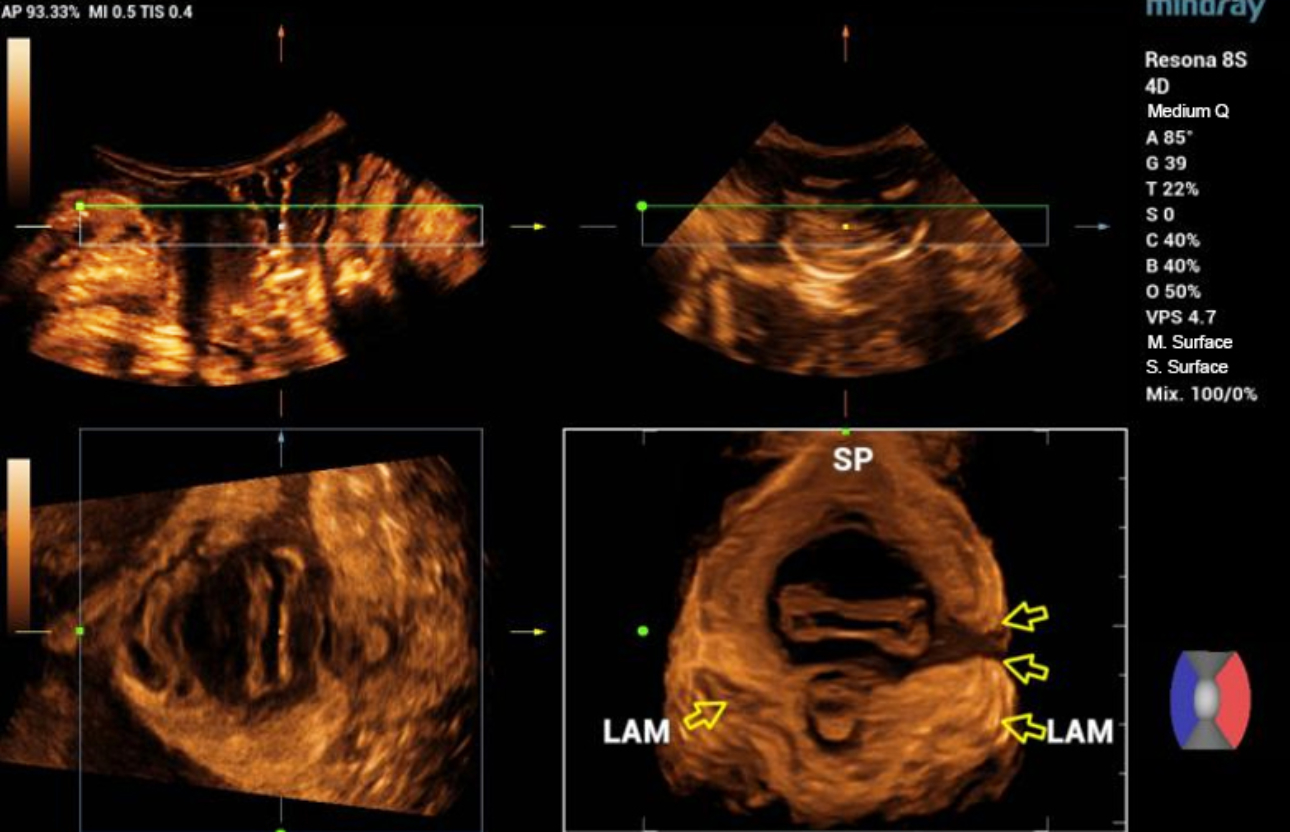
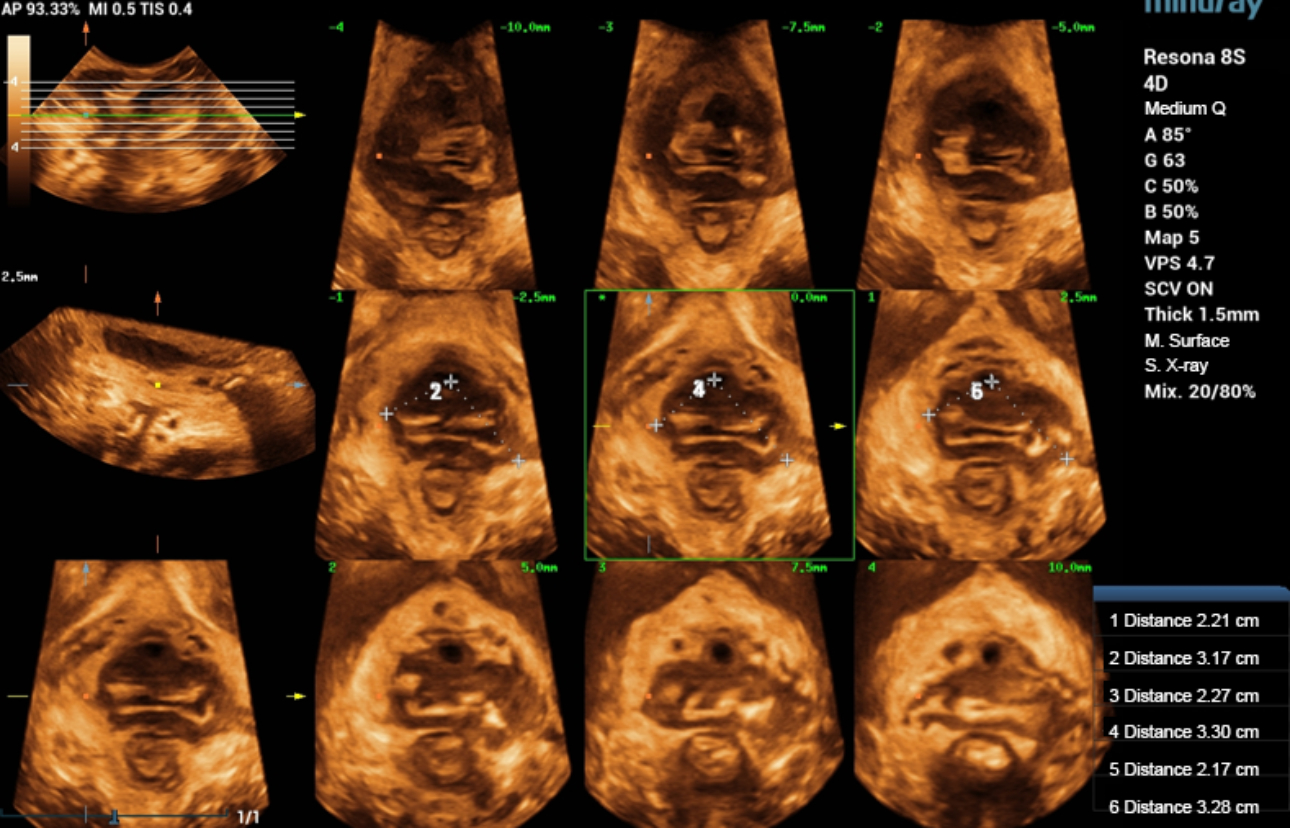
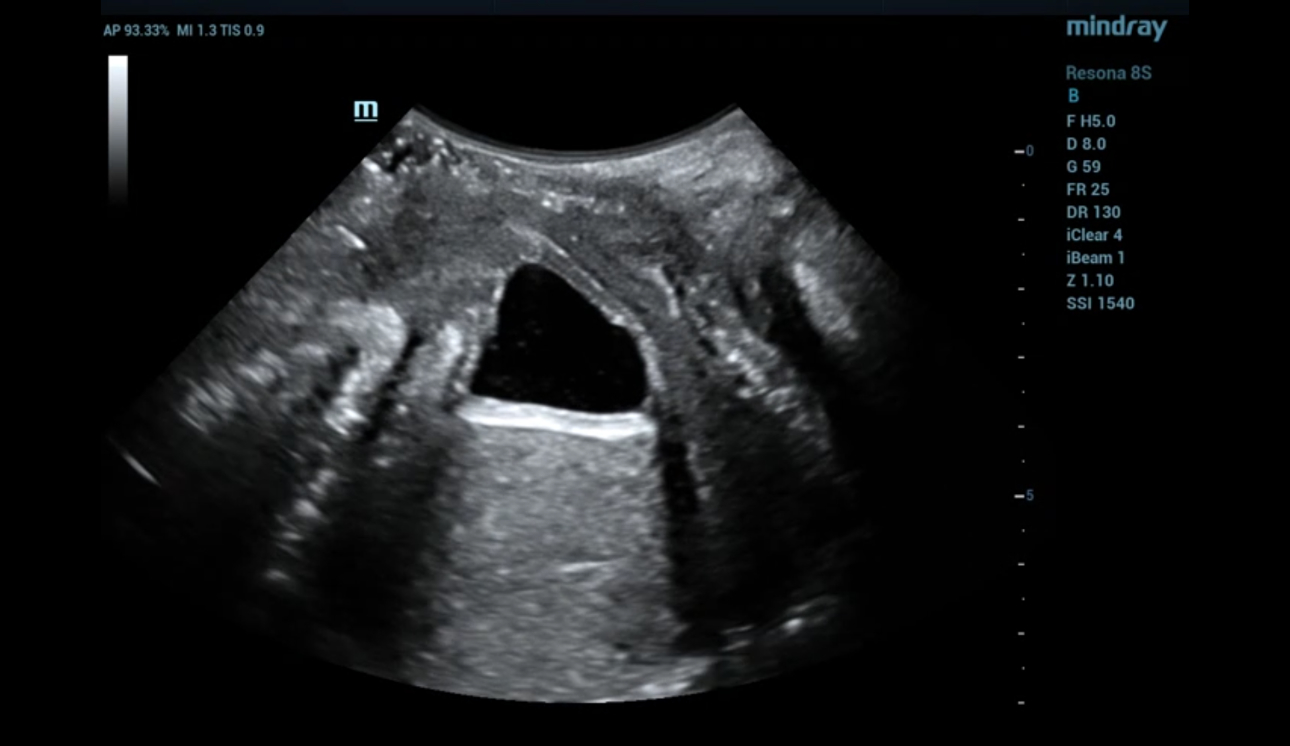
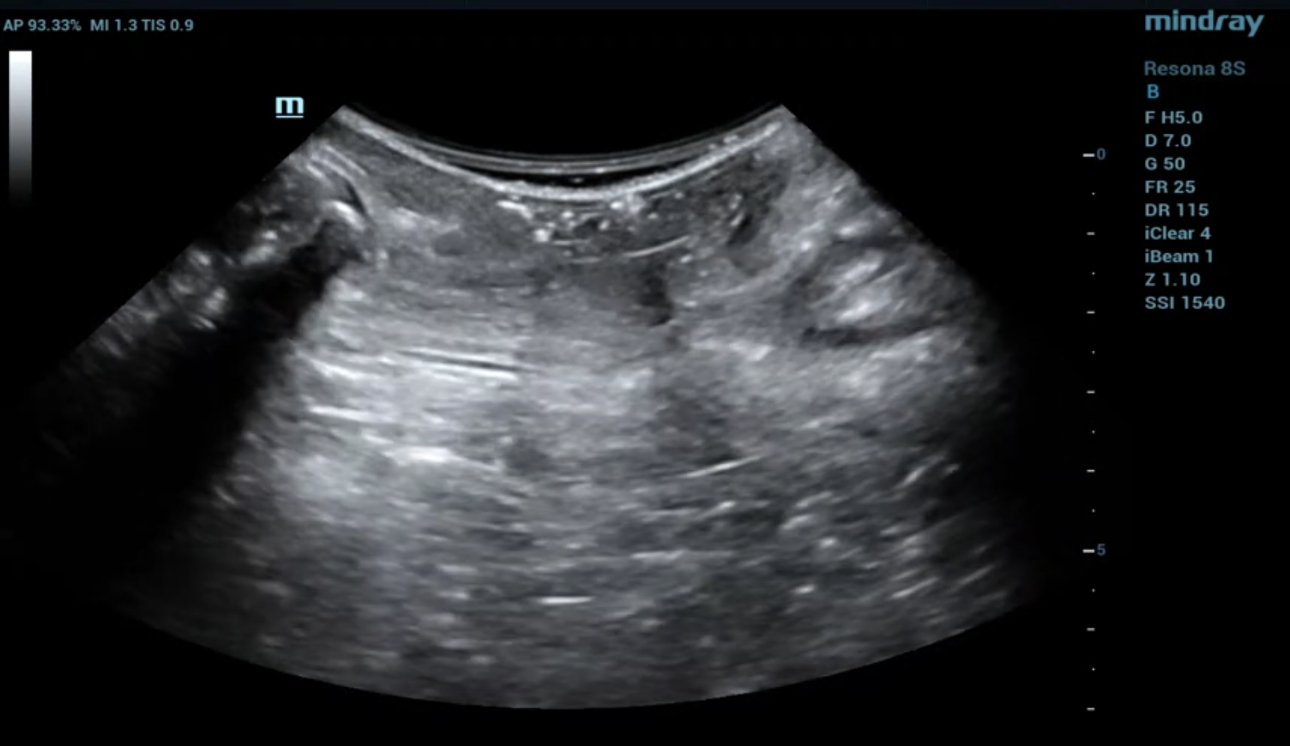
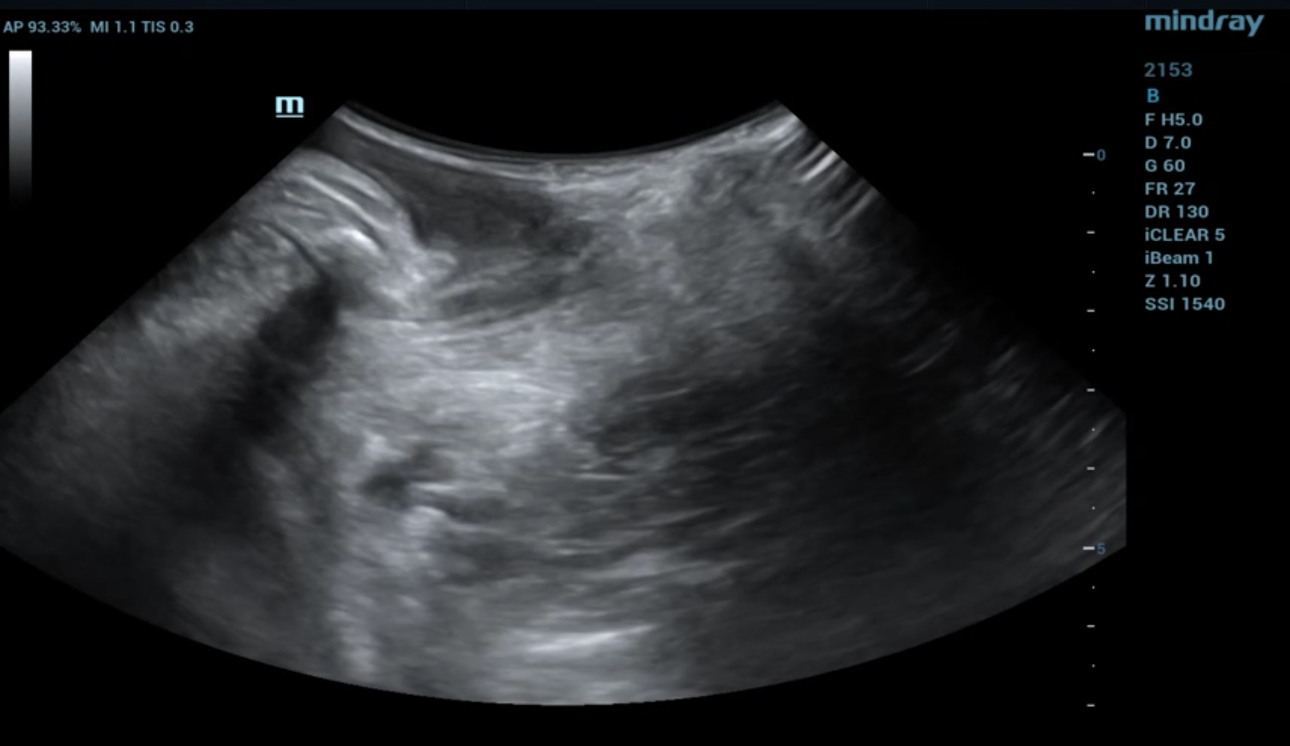
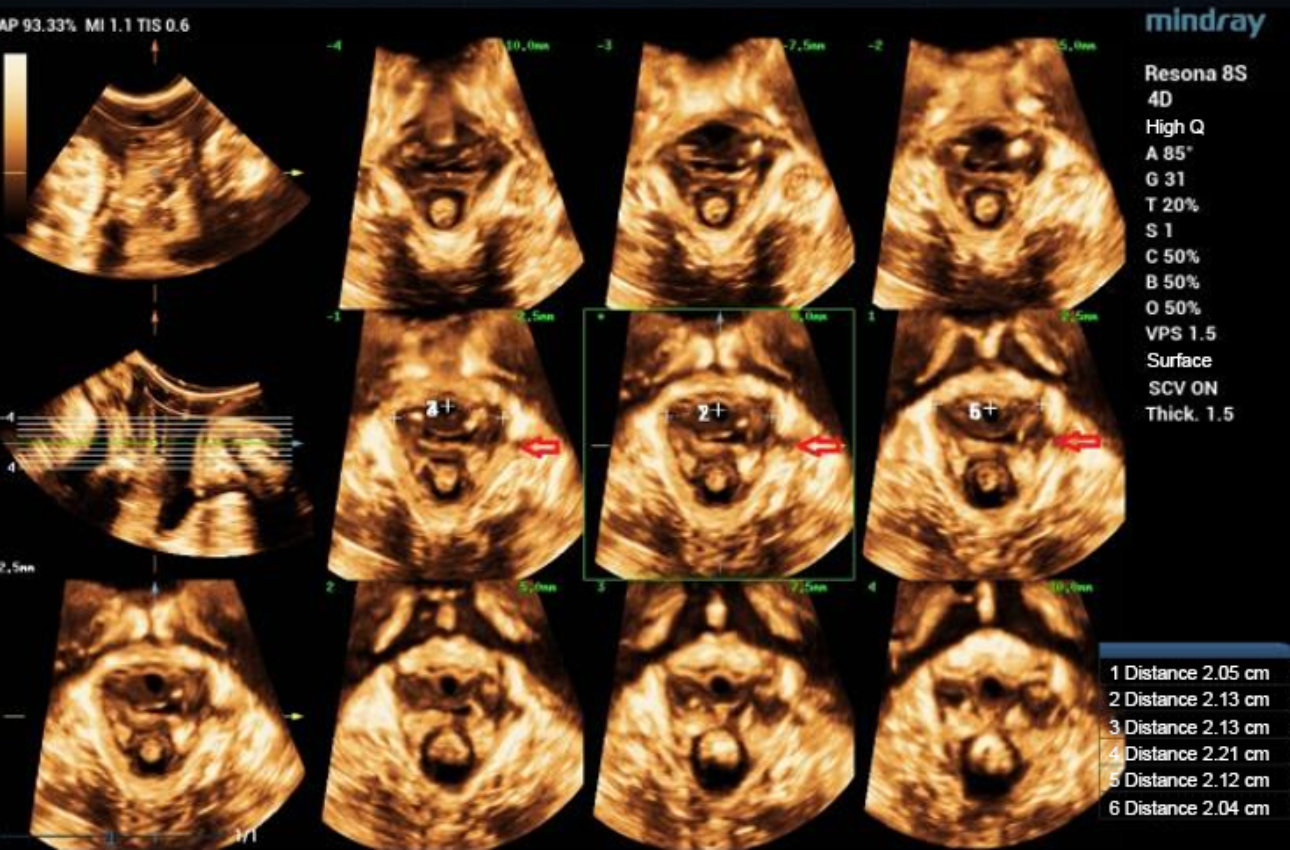
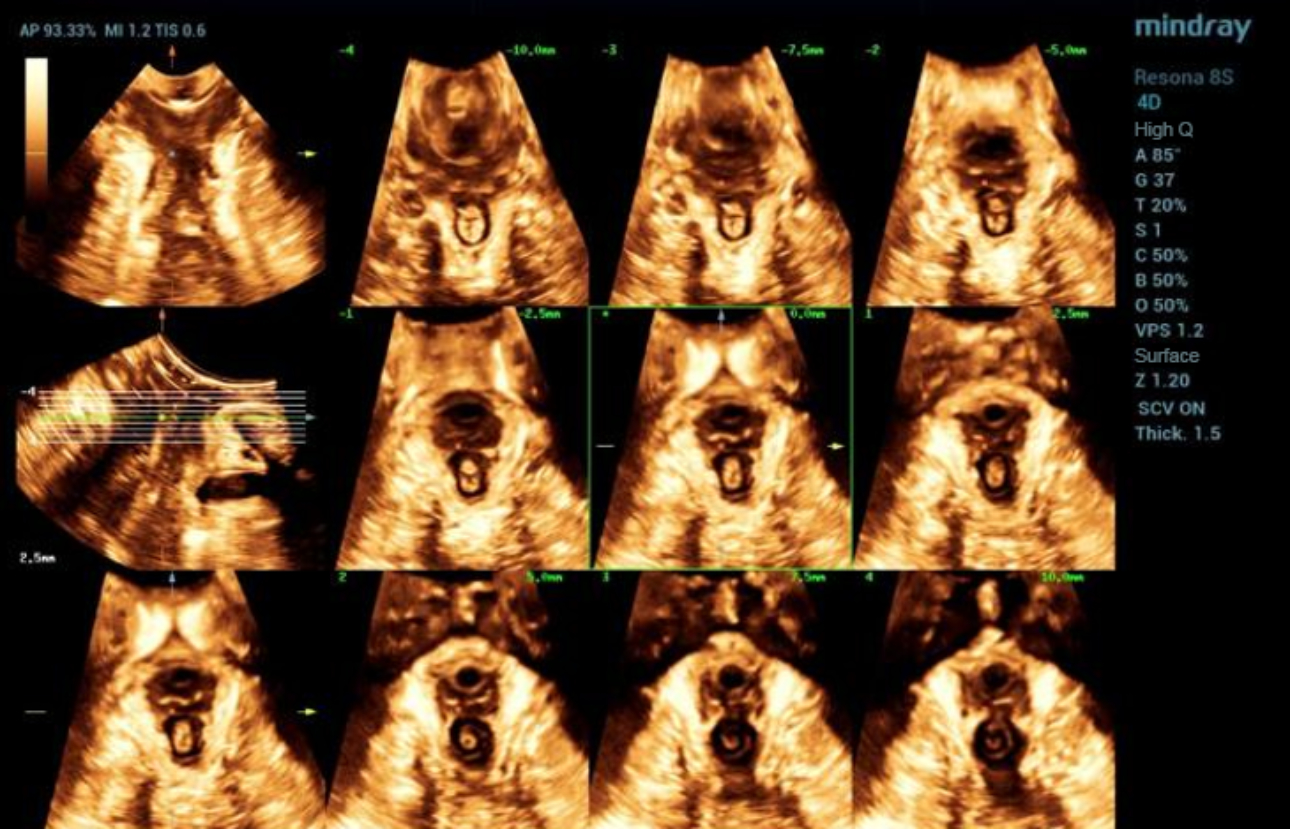
The main scanning methods include transperineal/intraluminal 2D scanning in parasagittal view, 3D/4D volume imaging, and tomographic ultrasound called iPage+.
Case Introduction:
A 30-year-old female, G1P1, vaginal delivery at 39+ weeks. Negative-pressure vacuum extraction and left perineotomy were applied during delivery. The weight of the newborn is 3370g. Pelvic floor ultrasound was carried out 42 days after delivery.

Discussion:
Differential Diagnosis:
1. False positive caused by gas inside and outside the probe sleeve:
2. Congenital agenesis of levator ani muscle:
The development of levator ani muscle is abnormal, mostly bilateral and symmetrical, presented as thin levator ani. Volume imaging is helpful for differential diagnosis.
3. The levator ani muscle is pushed by the perineal subcutaneous hematoma.
Key Points of Ultrasound Diagnosis of Levator Trauma:
- 2D scanning: The levator ani muscle fibers are completely or partially interrupted; the edge of the broken end is coarse. The levator ani muscles are asymmetrical on both sides.
- Volume imaging: The levator hiatus is asymmetric and deviated to the injured side.
- iPage+: If more than three slices show levator avulsion on one or both sides, the diagnosis of levator trauma may be considered.
Precautions for Scanning:
- When observing the integrity of the muscle, the scanning must start from the starting point to the ending point of the muscle along the direction of the muscle fibers, so as to avoid omission.
- Combine intracavitary probe and superficial probe that have high frequency to help diagnose when the diagnosis is not clear.
- If levator trauma cannot be excluded, the pelvic floor ultrasound should be repeated after 1–2 months.
Treatment:
Patients are advised to avoid fatigue and start rehabilitation exercise 3 months postpartum. At present, the main treatment methods include:
- Rehabilitation treatment, such as pelvic floor electrical stimulation and vaginal dumbbell exercise, can alleviate some clinical symptoms.
- Pelvic reconstructive surgery.
The long-term efficacy of these treatment methods still requires further evaluation.
Reference:
[1] DeLancey J, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 2003;101(1):46–53.
[2] Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol 2005;106(4):707–12.
[3] Hans Peter Dietz, Pelvic floor ultrasound: a review. American Journal of Obstetrics & Gynecology 2010(4); 321-334.