In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Case introduction
A 70-year-old female patient was admitted to the hospital due to “intermittent chest pain for half a month, which has been aggravating for 4 days”.
Half a month ago, the patient developed chest pain symptoms after vigorous physical activity, which manifested as a dull pain, accompanied by radiating pain in the left shoulder, back and left upper limb, as well as palpitations. The patient had no dyspnea, sweating, cough, expectoration, loss of consciousness and other symptoms. The symptoms could relieve after 1 hour of rest, and subsequent episodes of intermittent chest pain were induced mainly by physical activity, which could alleviate spontaneously after about 1 hour of rest. In the past 4 days, the symptoms of chest pain were worse than before, and the duration was longer than before. The patient sought treatment at a local tertiary A-level hospital. An electrocardiogram revealed: atrial fibrillation, ST segment depression in leads II, III, avF, and V4 - V6. A laboratory test showed: Troponin was 39.46 ng/mL. The possibility of “acute myocardial infarction” was considered, and the patient was admitted to the cardiovascular intensive care unit from the emergency department.
Past Medical History
The patient had a history of hypertension for a year, with her highest blood pressure being 180/120 mmHg, which was not regularly controlled. She denied a history of diabetes.
First Physical Examination at Admission
T 36.3°C, BP 100/65 mmHg, PR 113 bpm, RR 20 rpm, the patient’s consciousness was clear and mentally poor, HR 120 bpm, her heart rhythm was absolutely irregular, and the intensity of the first heart sound varied.
First Auxiliary Examination at Admission
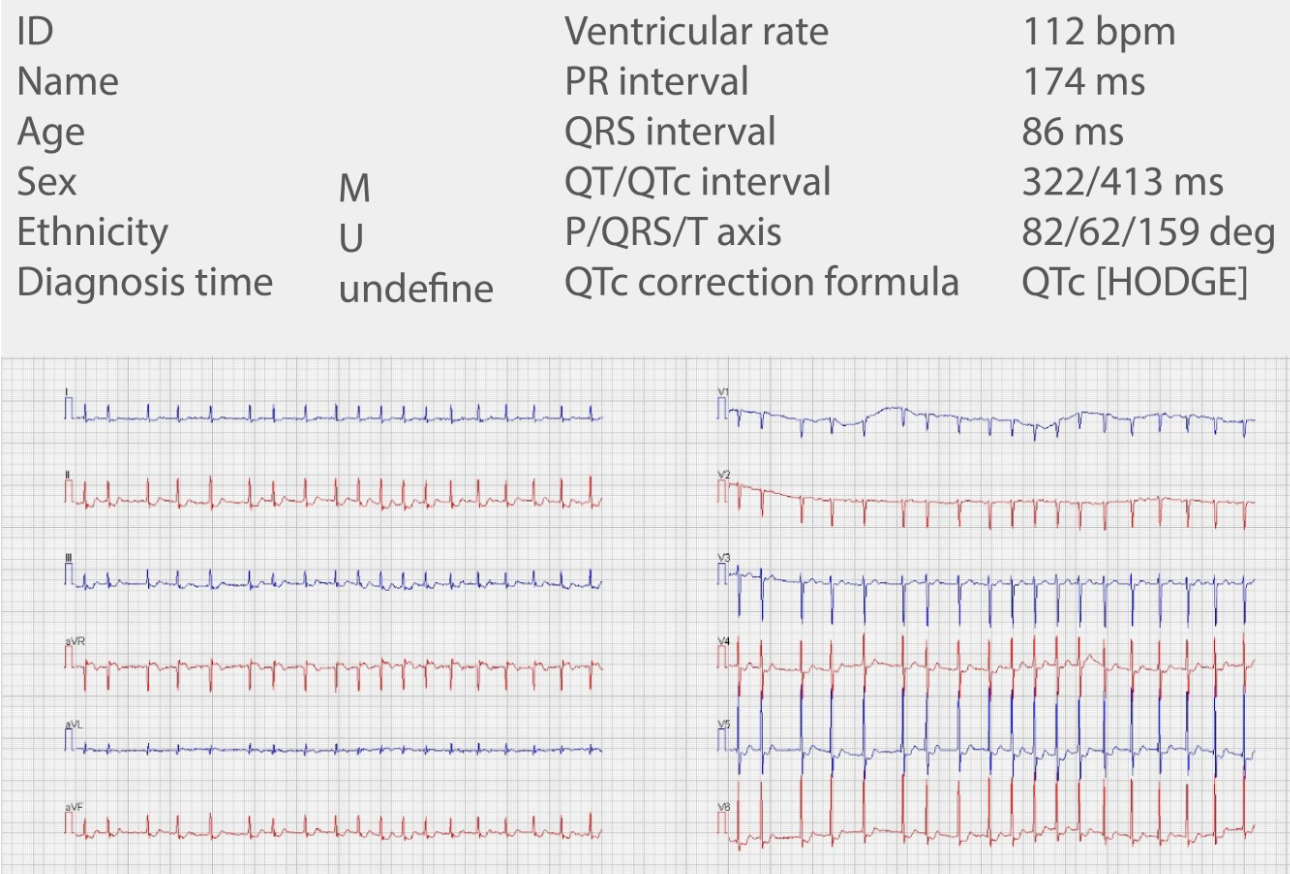
Electrocardiogram
Preliminary Diagnosis
- Killip class I acute non-ST-segment elevation myocardial infarction
- Grade 3 hypertension, extremely high risk
- Atrial fibrillation
The post-admission monitoring is as follows
Electrocardiogram
The patient was given ECG monitoring throughout the whole process. The patient’s heart rate was relatively fast, fluctuating in the range of 70 - 150 bpm, which frequently triggered the monitor’s “tachycardia” related alarm, and occasionally triggered the “extreme tachycardia” alarm with a heart rate exceeding 170.
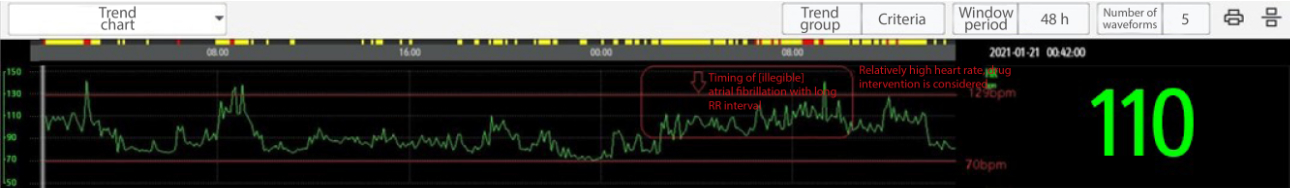
Early morning on Day 2 of admission
The patient’s heart rate fluctuated at an average of 110 bpm, and the nurse reported that the patient had atrial fibrillation and a high heart rate throughout the whole process. The “atrial fibrillation with long RR interval” alarm was triggered in the early morning.

The patient had frequent atrial fibrillation and tachycardia throughout the process, and her heart rate exceeded 150 bpm multiple times, which met the criteria for intermediate-to-high-risk atrial fibrillation in ECG critical values If there is no “atrial fibrillation with long RR interval” alarm, amiodarone will be routinely used for cardioversion.
However, the triggering of the “atrial fibrillation with long RR interval” alarm in this patient indicated that there may be risks such as conduction block and bradycardia. (Due to the long half-life of amiodarone, it may cause persistent sinus bradycardia or risk of conduction block after conversion of atrial fibrillation, causing the patient to experience syncope)
Therefore, after comprehensive consideration, it was decided to use dronedarone with a short half-life (the half-life of dronedarone is only 1 to 2 days after drug discontinuation, while the half-life of amiodarone is 6 to 8 weeks) for cardioversion and heart rate lowering therapy to effectively reduce the risk of syncope and arrhythmia events caused by long drug half-life after cardioversion.
Results
After oral treatment with dronedarone, the patient’s cardioversion was successful. There were no adverse events such as persistent sinus bradycardia or conduction block after drug discontinuation.
Analysis
Clinically, “long RR interval” is often overlooked or delayed during arrhythmia treatment, mainly due to the following reasons:
- The monitor does not have a “Long RR Interval Alarm”. The related “skipped beat” and “pause” alarms cannot specifically prompt long RR interval events, especially “atrial fibrillation with long RR interval” events that may trigger syncope.
- Some experienced clinicians can use thumbnails to find the “longest RR interval”, but dozens of hours of monitoring data make it easy to overlook this “long RR interval” of about 3 seconds. For example, as can be seen from the thumbnail of this patient, the patient had atrial fibrillation and arrhythmia throughout the whole process. In addition to the “long RR interval” of 3 seconds identified in the white box, there were dozens of “RR intervals” of 1 to 2 seconds long. During hectic hours, it is undoubtedly very difficult to timely identify arrhythmia events that point to high-risk atrial fibrillation and the risk of syncope from 40h, 2,400 lines (1 minute/line thumbnail) of thumbnails.
- In addition, some experienced clinicians is able to find the patient’s “long RR interval” through the slowest heart rate, but this is not a reliable method. For this patient, the slowest heart rate was 70 bpm, when the “long RR interval” occurred was 96 bpm, and the aforementioned arrhythmia event could not be identified by the slowest heart rate.
As can be seen above, for clinical purposes, “Atrial Fibrillation with Long RR Interval Alarm” can effectively help clinicians first identify whether atrial fibrillation and high heart rate in patients are accompanied by heart rhythm problems. It provides efficient and precise assistance for clinicians in the formulation of the next treatment regimen.
Mindray iStatus & iAlarm has a combination BeneVision monitoring system of “patient status display interface” and “atrial fibrillation with long RR interval”. When the abnormal heart rhythm of the patient is captured, the iStatus & iAlarm prompting abnormality alarm will be displayed in the patient status display area on the monitor’s main interface, laying the foundation for accurate decision-making and better treatment effect.
References
Huang Congxin, Zhang Shu, Huang Dejia, et al. Atrial fibrillation: current knowledge and treatment recommendations (2018) [J]. Chinese Journal of Cardiac Arrhythmias, 2018, 22(4):279-346.


