More than a million people worldwide have been infected by COVID-19 with thousands of medical staff included. WHO declared the COVID-19 a pandemic on March 11th recently stated that “When health workers are at risk, we’re all at risk”. This is why the urgent demand for personal protective equipment is at an all-time high. Healthcare workers are exposed to respiratory hazards in various forms, mainly airborne inhalation and droplets from an infected person. Diseases, which respect no national boundaries, can challenge efforts to protect workers especially handling patients with COVID-19. Healthcare workers can protect themselves when caring for patients by adhering to infection prevention and control practices, including appropriate use of engineering controls, administrative controls, and personal protective equipment (PPE).
Patients with severe COVID-19 should select the appropriate respiratory support therapy based on the severity of hypoxemia. For COVID-19 patients with mild to moderate hypoxemia, oxygen therapy with nasal cannula or simple oxygen masks, nasal high-flow oxygen therapy, and non-invasive ventilation (NIV) are the preferred for respiratory support. NIV, invasive mechanical ventilation (IMV), and external membrane oxygenation (ECMO) are used for moderate to severe hypoxemic patients. Due to the characteristic of airborne transmission in COVID-19 patients, droplets and aerosols from the patient presents a great challenge for prevention and control of infection under different respiratory therapy strategies.
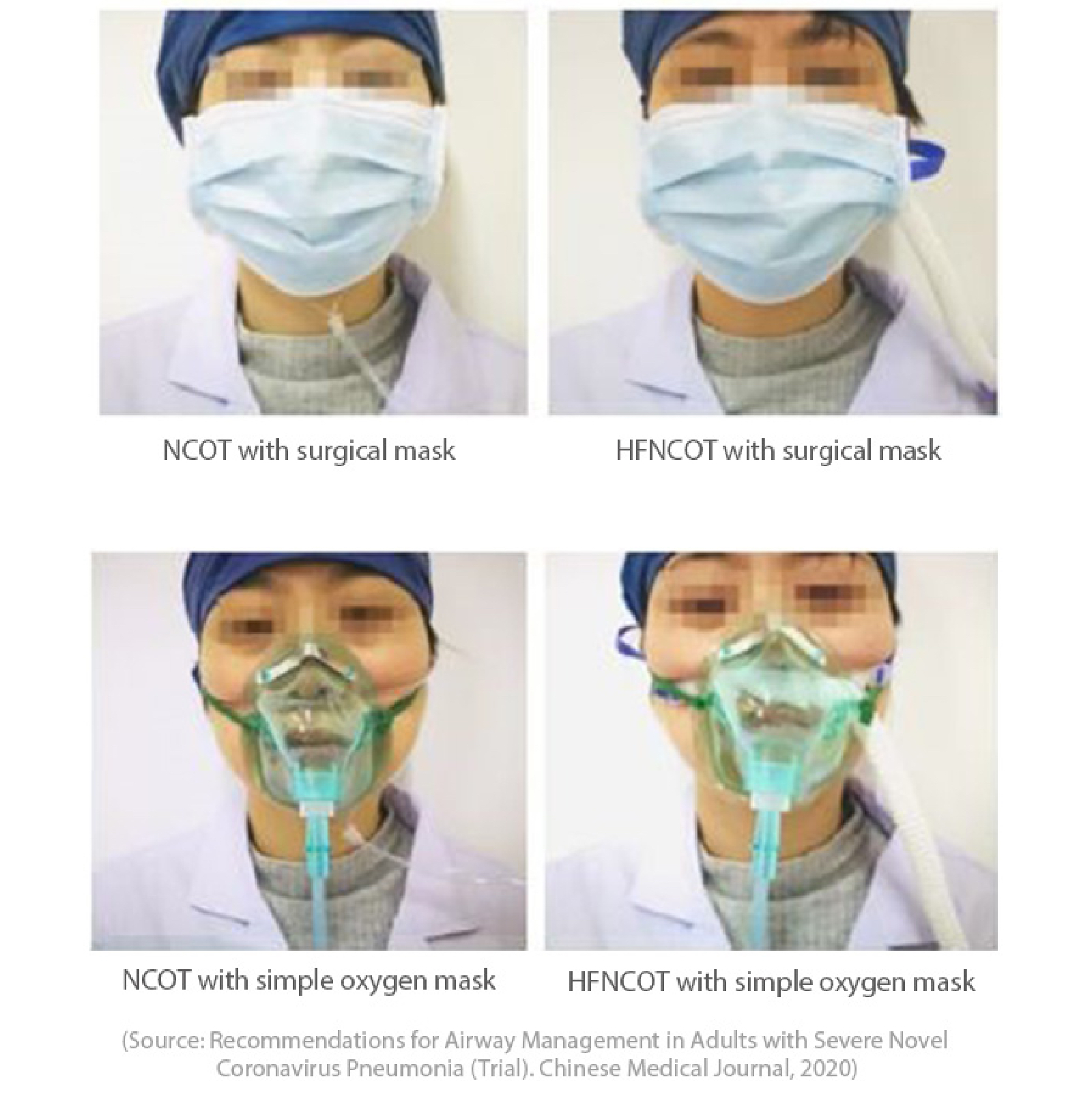
Patient airway management personal protective equipment (PPE) configurations
Reducing Aerosol Dispersion during Nasal Cannula or Nasal High-Flow Oxygen Therapy
Nasal cannula oxygen therapy (NCOT) and high-flow nasal cannula oxygen therapy (HFNCOT) are open-system oxygen delivery methods. With humidification, the flow of oxygen generates a large amount of aerosols which may carry virus. In addition, the high-speed oxygen flow can further aid the spread of virus-containing aerosols to the surrounding environment, which increases the risk of infection for the healthcare workers.
Correctly wearing of surgical or N95 masks for patients can significantly reduce the spread of virus-containing aerosols during coughing and breathing. Some researchers have combined N95 masks with nasal cannula to design a new type of oxygen therapy mask, which can effectively reduce the aerosol transmission. Airtight sealed masks with bacterial and viral filters are also believed to effectively reduce aerosol diffusion.
Clinical Recommendation
1. For COVID-19 patients with mild to moderate hypoxemia (oxygenation index > 150 mmHg, 1 mmHg = 0.133 kPa), it is recommended to use NCOT, HFNCOT simple masks and NIV.
2. During NCOT or HFNCOT, the patient should wear a surgical mask or facial mask outside the nasal catheter to further reduce the spread of viral aerosols (see Figure 1); if possible, use an airtight mask or an oxygen tent.
Reducing Aerosol Dispersion during Non-Invasive Ventilation
Based on multiple studies of SARS, H1N1, it has been proved that non-invasive ventilation may cause aerosol dispersion, increasing the risk of infection. Guidelines from the European Respiratory Society / European Society of Intensive Care (ERS/ESICM), the World Health Organization (WHO), the National Health Service (NHS), the Hong Kong Chest and Lung Foundation, and the American Respiratory Therapy Association (AARC) suggest that during an epidemic of infectious diseases, non-invasive ventilation is still a high-risk therapy which requires extensive prevention. However, experience from many front-line pulmonary critical care experts in Wuhan, shows that many severe patients with mild/moderate hypoxemia can be effectively treated with non-invasive ventilation (NIV).
Clinical Recommendation
1. Non-invasive ventilation can be used as first-line treatment for severe COVID-19 cases with mild to moderate hypoxemia.
2. Other patients who may have contact with a patient receiving NIV are required to wear sufficient protective equipment. Try to use NIV in a single-ward or negative-pressure room if possible. Reduce the frequency of visits by the medical workers, and strictly monitor their symptoms or signs of infection of the NIV patient.
3. Use a dual-limb circuit ventilator as much as possible and add virus/bacterial filters to the machine. Disposable circuit (i.e. single-patient use) is recommended. The circuit and filters should be treated as medical waste.
4. In terms of the parameters of ventilators, a lower inspiratory pressure should be selected at first, which could later on be adjusted according to the respiratory rate and arterial blood gas of the patient.
5. As for the method of connection, a helmet is preferred, followed by a full-face mask or a well-sealed mask. Avoid the use of nasal mask. Make sure to have a viral/bacterial filter placed between the mask and the expiratory valve (port). It is recommended to wear the mask before turning on the ventilator as well as turning off the ventilator before removing the mask.
Establishing Artificial Airways: When and How
Critically ill COVID-19 patients require mechanical ventilation in the event of severe hypoxemia and respiratory distress. Related clinical studies of MERS, SARS, and influenza have shown that NIV has a higher failure rate for such patients, and delayed intubation may increase patient mortality. According to the experience by clinical experts in this round of pandemic, COVID-19 patients have a slower progression of respiratory failure compared with SARS patients. In addition, some patients with severe respiratory failure can still be successfully treated with NIV. It is still recommended to use NIV as preliminary support while invasive ventilation should be established immediately if the following patient condition occurs:
1. Deterioration of consciousness (disobey instructions or restlessness);
2. Upper airway obstruction (wheezing, delayed inspiratory sounds);
3. Deterioration of oxygenation [oxygen saturation (SaO2) below 92%, while FiO2 > 60%] or deterioration of ventilation [respiratory rate below 30 times/min];
4. Arterial Partial pressure of carbon dioxide (PaCO2) exceeds 40 mmHg to 50 mmHg.
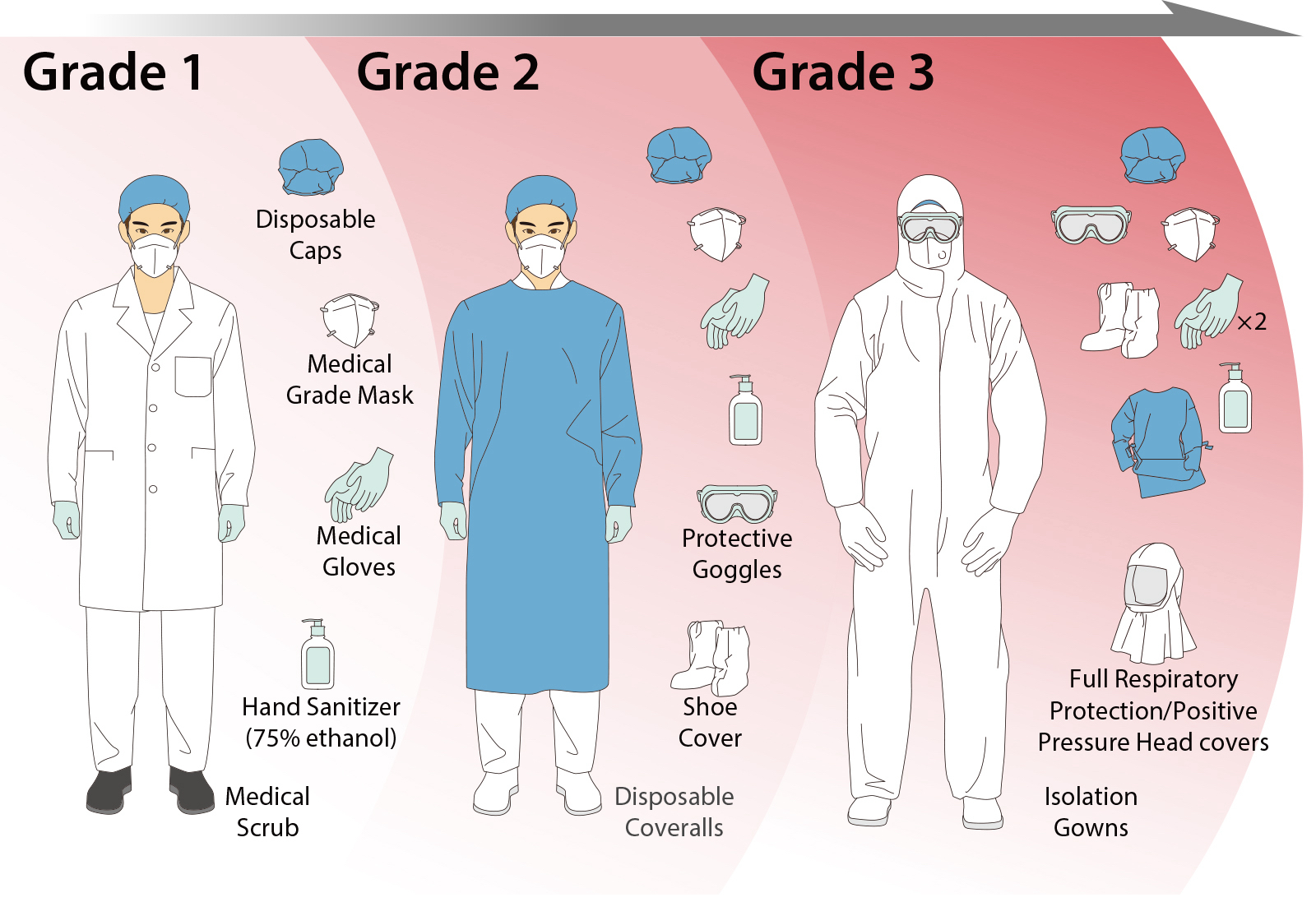
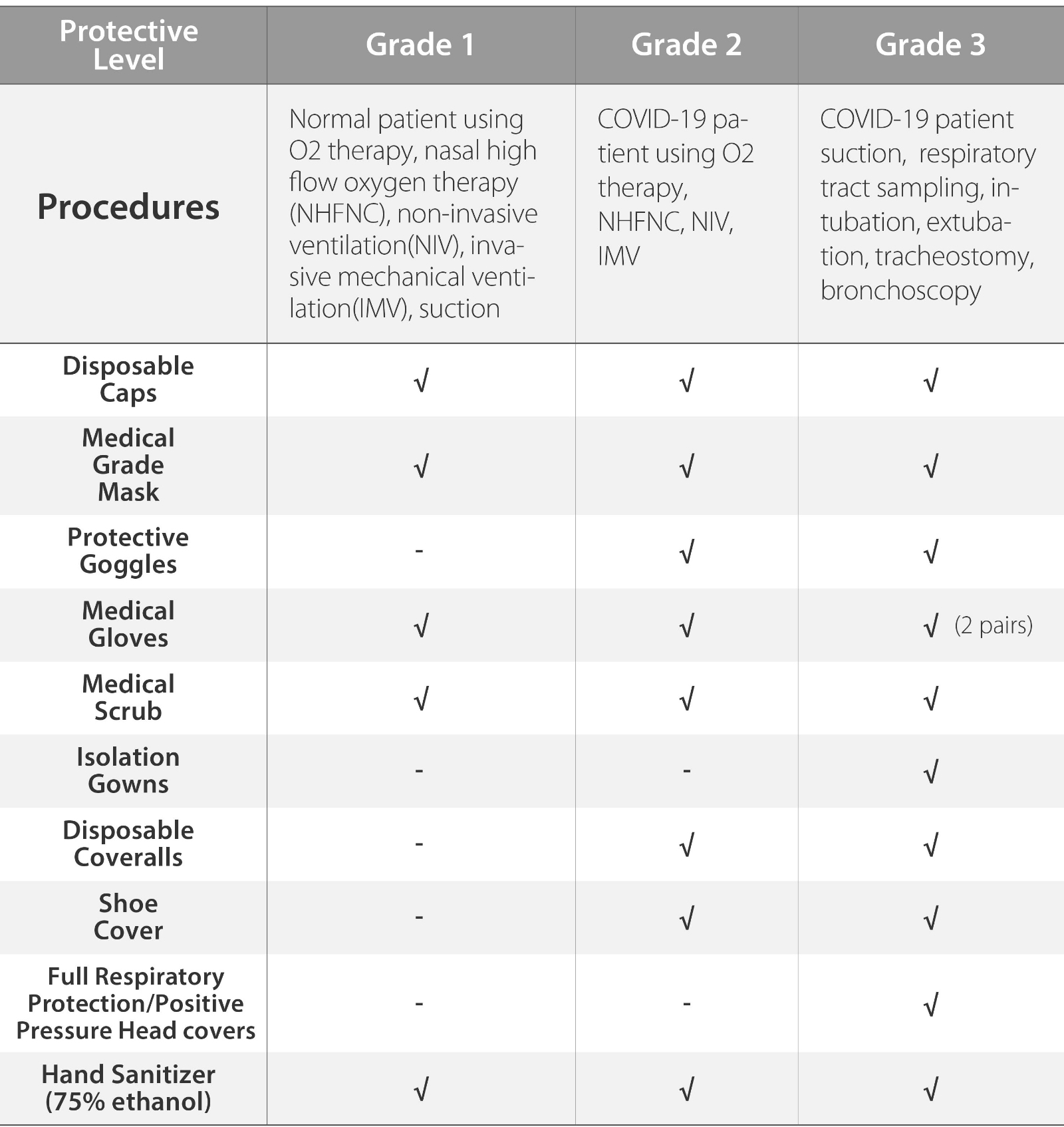
The principle of establishing an artificial airway is to minimize coughing and the transmission of droplets in patients. Endotracheal intubation is divided into two types: oral and nasal. It is highly recommended to operate this therapy with Grade-3 prevention standards, with oral endotracheal intubation preferred. Try to avoid the use of ordinary laryngoscope, which will stimulate the glottis and cause a large amount of airway secretions to be expelled. Electronic laryngoscope or bronchoscope can be used to guide the insertion to reduce operator exposure time during intubation. When there is a contraindication to oral intubation, nasal tracheal intubation under the guidance of a bronchoscope can be used as an alternative.
Since it is difficult to use the bronchoscope when using positive pressure headgear, an electronic bronchoscope should be used whenever possible. The use of electronic bronchoscopes can also avoid being too close to the patient, reducing the chance of contamination from splatters. Due to high risk of sputum and blood splatter, tracheotomy is not the initial option.
Clinical Recommendation
1. Oral intubation is preferred for the establishment of artificial airways, and tracheotomy should be avoided as far as possible.
2. It is recommended to use electronic laryngoscope or fiber bronchoscope to guide the intubation. Use an electronic bronchoscope with display screen, if available.
3. The ward should be promptly ventilated after performing intubation.
Preventive Measures during Tracheal Intubation
When patients require intubation, careful prevention and control measures must be taken in three aspects: the operator, the patient, and the environment. During intubation, the operator should avoid repeated attempts to reduce exposure. When performing intubation, the operator shall follow Grade-3 protection standards and wear protective equipment. It is recommended to quickly intubate in combination with sedatives, analgesics and neuromuscular blockade to reduce coughing. Intubation should be performed in a negative pressure ward, which can effectively reduce the risk of infection to the medical workers.
Clinical Recommendation
1. During intubation, personal protective equipment (PPE) should be worn in accordance with Grade-3 protection standards, and it should be operated, if possible, in a negative pressure ward. An air purifier can be used if it is available.
2. It is suggested that tracheal intubation be done quickly with sufficient sedation and analgesia, to reduce coughing and transmission of droplets.
Suctioning during Invasive Mechanical Ventilation
For patients relying on artificial airways, it is strongly recommended that a closed-suctioning device should be used for this therapy. It should be determined carefully whether the patient requires suctioning or not, to avoid frequent and unnecessary suctioning, which may lead to discomfort or cause severe coughing. Suctioning may be considered if and when the patient has the following clinical manifestations:
1. The patient has noticeable secretions in the airway (directly visible or heard through cough sound);
2. The ventilator shows apparent sawtooth in flow-volume loop waveforms or on expiratory flow-time waveforms;
3. The ventilator shows an increase in peak airway pressure (volume-control mode) or a decrease in tidal volume (pressure-control mode);
4. The patient has decreased oxygenation (through a pulse oximeter), increased respiratory rate and compulsory breathing;
5. The patient has worsened arterial blood gas (ABG) results, (e.g. PaCO2 rose sharply);
6. The patient has increased heart rate and blood pressure, shows irritability or sweating.
For patient requiring high FiO2 or positive end-expiratory pressure (PEEP) and/or shows significant deterioration of vital signs, pre-oxygenation should be performed for 2 minutes before suction to avoid hypoxemia during suctioning. Disconnecting the ventilator circuit may cause alveolar collapse and large transmission of droplets and aerosol. Therefore, it is recommended to use closed-suction, to reduce the risk of pathogen transmission.
Shallow suctioning can be used to avoid mucosal edema, inflammation, severe coughing, and even bleeding caused by the stimulation of carina and airway. Each suction period is preferably < 15 seconds, and continuous negative pressure should be performed and maintained between 80 and 150 mmHg during suctioning. The closed-suction should be replaced every 24 hours.
Unless required by the patient, conventional bronchoscopy is not recommended for suctioning. Unless necessary, make sure that a three-way connector (i.e. T-Piece) is used to avoid disconnection of the breathing circuit!
Clinical Recommendation
1. Closed-suction should be based on the patient's clinical manifestations. Pre-oxygenation can be given for 2 minutes prior to suction.
2. Shallow suctioning is preferred with each session less than 15 seconds.
3. Conventional bedside bronchoscopy is not recommended. If necessary, a three-way connector (i.e. T-piece) in connection to the breathing circuit.
Reference:
Critical Respiratory Medicine Group at the Respiratory Medicine Branch of the Chinese Medical Association, Critical Care Medical Working Committee at the Respiratory Medicine Branch of the Chinese Medical Doctor Association. Recommendations for Airway Management in Adults with Severe Novel Coronavirus Pneumonia (Trial). Chinese Medical Journal, 2020,100 (00): E004-E004. DOI: 10.3760 / cma.j.issn.0376-2491.2020.0004