In the UK, the NHS has adopted an ambitious digital transformation agenda to enhance diagnosis and treatment in public healthcare while delivering more efficient services to patients.
Mindray is working closely with North Tees and Hartlepool NHS Foundation Trust in the UK to lead the way in digital transformation within the NHS. The Trust serves around 400,000 people living in Hartlepool, Stockton and parts of County Durham and has over 500 beds at its busy hospitals. As clinical teams stretch themselves to meet increasing demand for healthcare services, the Trust’s approach to technology is about freeing up nurses’ time, so they can spend more time with each patient.
Pursuing Optimal Performance
To streamline workflows and save time, the Trust is customising two-way data flows to collect the monitoring information that’s most important for each ward or specialism while reducing the manual, administrative burden for clinical teams. For instance, in the ITU, the continuous monitoring data sent to EPRs was expanded to not only include patient monitors, but also third-party ventilators and New Early Warning Scores (NEWS) 2 data. This ensures clinical teams remain responsive to any early signs of deterioration while also supporting smoother transfers between departments and stage downs to lower acuity settings as the EPR automatically provides a more complete view of patient health.
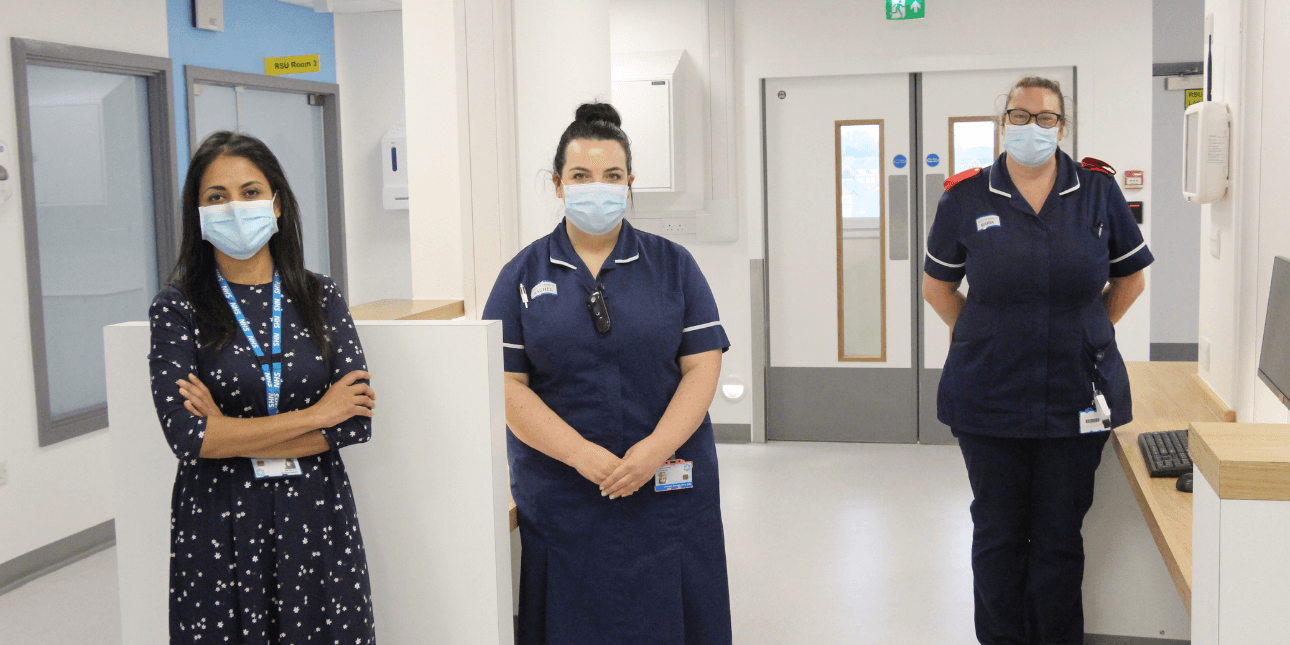
Kelly Calvert is the chief nursing information officer at the North Tees and Hartlepool NHS Foundation Trust and one of the leaders in the NHS’ Digital Change programme. Working with Mindray, Kelly aims to make digital workflows as efficient as possible for each department.

Kelly Calvert
Chief Nursing Information Officer, North Tees and Hartlepool NHS Foundation Trust
Interoperability of data between devices and clinical systems is certainly important, but for me, that alone isn’t enough to make our device set-up efficient for staff. Before I ask busy nurses and other clinicians to use new technologies in the Trust, I need to ensure it won't create unnecessary work and that it will save staff time. Technology must be deployed in ways so that it helps staff as they deliver safe and effective patient care. We need to make it easy and efficient both to capture data on devices, and to make that data available.
Suppliers need to understand workflow needs too, so we can collaboratively push the boundaries of what their products do. I’m glad to say that Mindray actively supports this.
A pandemic push
The first project started in the purpose-built Respiratory Support Unit (RSU) which was opened during the Covid-19 pandemic to allow nurses to care for respiratory patients.

The Trust had deployed Mindray patient monitoring devices in the unit to capture vital signs at the bedside. Working with Mindray, a Central Monitoring System (CMS) was installed so that staff could view the data acquired from all the devices on big central screens so clinical teams could easily spot when a patient starts to deteriorate.
Using these digital workflows, RSU staff could capture electronic observations directly from the patient monitor and view it in real time on the CMS without any manual intervention. Prior to this, though the Trust had deployed similar devices on general wards that integrated with early warning charts in its EPR, many high acuity areas largely relied on paper to carry out observations. Not only did this provide better access to patient data, but as information was visible remotely, there was less unnecessary contact between patients and medical staff, reducing the risk of transmission.

Mindray has since begun work on a new interface that will allow National Early Warning Scores (NEWS2) and additional respiratory specific parameters to populate the observations chart on the EPR, providing the critical information that’s relevant for the RSU team.
Going further – so that nurses do things once
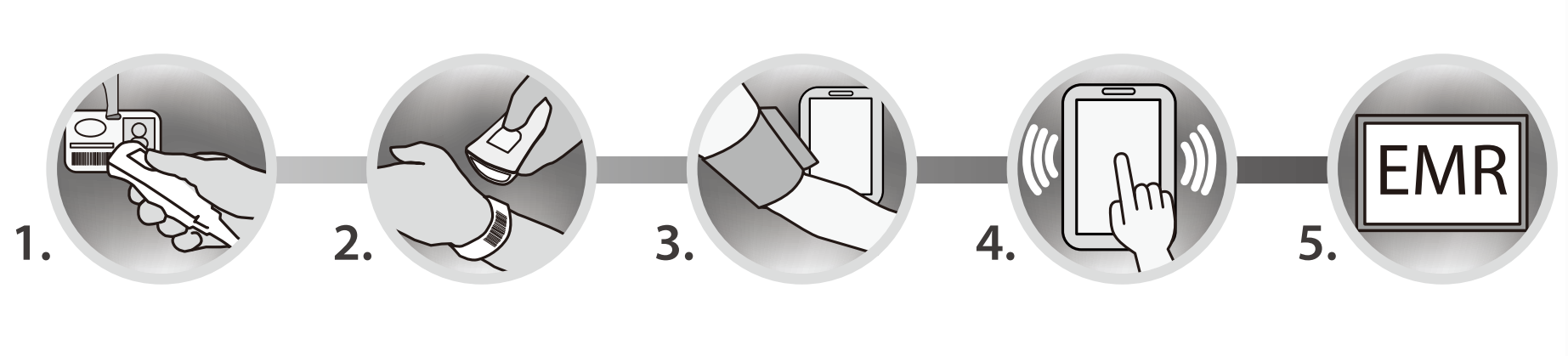
Timely interventions are crucial in any treatment, but there was special urgency during the pandemic. In RSU, devices are now configured so that nurses only need to enter information in one place. Typically, the Mindray patient monitoring device has a standard set of menu options. But for respiratory observations, nurses needed to capture additional information – such as whether the patient is on non-invasive ventilation, the oxygen level, and other specific information.
The ventilators weren’t capable of sharing this information so to avoid nurses having to input data manually on a separate tablet or mobile device, Mindray developed new menu options on the patient monitor so that all this information: their blood pressure, heart rate, sats, consciousness level, the patient’s pain score and other bespoke departmental measurements, could be entered by nurses in one place.
All of that information is then transmitted directly from the device into the electronic patient record. Most importantly, it means nurses only need to do things once.
A Blueprint for Connectivity
Mindray and the Trust have used what they’d learned from the RSU in other high-acuity areas, with similar approaches to efficient workflows in the emergency department (ED) and intensive therapy unit (ITU).
The ED will use a tailored approach to capturing standard four-hourly observations and continuous observations on the same high acuity Mindray monitoring device; a workflow which was first developed for RSU. And in ITU, the patient monitoring devices will be configured so that staff are alerted by the device with an event, if blood pressure drops for example. Nurses can comment on the event and write notes into the monitoring device, ensuring clinical teams always have the latest information.
For patients moving from ITU to a ward, and therefore from more detailed continuous observations to four-hourly observations, relevant National Early Warning Score parameters will be automatically extracted for the chart in their EPR. This means that people on the ward can see a complete observations history, relevant for the care they are providing.
“The ability for nurses to comment on an event and write notes using the patient monitoring devices is quite revolutionary and helps us keep patients safe. Both continuous observations flow sheets and early warning charts will be automatically updated in the EPR, removing a process for the nurse. We are also removing data entry risks as there is less manual data entry, and nurses must log into monitoring devices. Before observations are taken, nurses scan the unique barcode each patient wears into the device to ensure data is stored for the right person.”
The human side of nursing
The collaboration between Mindray and the North Tees and Hartlepool NHS Foundation Trust is a significant step forward from nurses having to write down scores, or enter data manually into the device or EPR.
None of this replaces the human side of nursing. One to one contact with patients and being able to spot what are called the ‘soft signs’, which can tell a nurse something isn’t right, remain crucial. With less administration and better access to patient data, nurses can focus on providing the very best care, and have a better chance of spotting when a patient needs intervention.
The collaboration is an important step towards realizing Mindray's goal of improving healthcare outcomes through digital innovation. The partnership allows Mindray to deeply understand the working needs of various departments within the Trust, providing an opportunity for Mindray to drive the digital transformation and upgrade of hospitals through innovative customized m-connect solutions.

Paul Bailey
General Manager of Mindray UK
Medical innovation originates from clinical practice and contributes back to clinical practice. Closely meeting the core needs of healthcare professionals and providing targeted solutions is Mindray's consistent research and development philosophy. The North Tees and Hartlepool NHS Foundation Trust provides Mindray with an opportunity to deeply understand the working needs of various departments. This forms the foundation for Mindray to drive the digital transformation and upgrade of hospitals through innovative customized solutions.
“Mindray has proved they are willing to listen and do things differently from both sides so that nurses can get even more out of the technology at the Trust. We want to make things quicker, easier and simpler. My nurses are already telling me they love this.” says Kelly.