Optimal utilization of mechanical ventilator at tertiary care hospital during Covid pandemic
Mindray 2021-12-13

Deepak Agarkhed, Dr. Anand.BM, Dr. Madhusudan R, Dr. Sreekanth Shetty, Dr. Bevin Dsilva, Biken from Sakra World Hospital, Bengaluru
Team of Sakra World Hospital, Bengaluru
Case study: Optimal utilization of mechanical ventilator at tertiary care hospital during COVID 19 pandemic
India is one of the top countries having more deaths so far due to Covid pandemic. Bangalore city too witnessed an average of 12 COVID-19 deaths a day in first wave and 96 COVID 19 fatalities a day in the second wave. Indian healthcare system was under severe challenges including bed availability, Oxygen consumption and medical equipment due to unprecedented surge of Covid patients
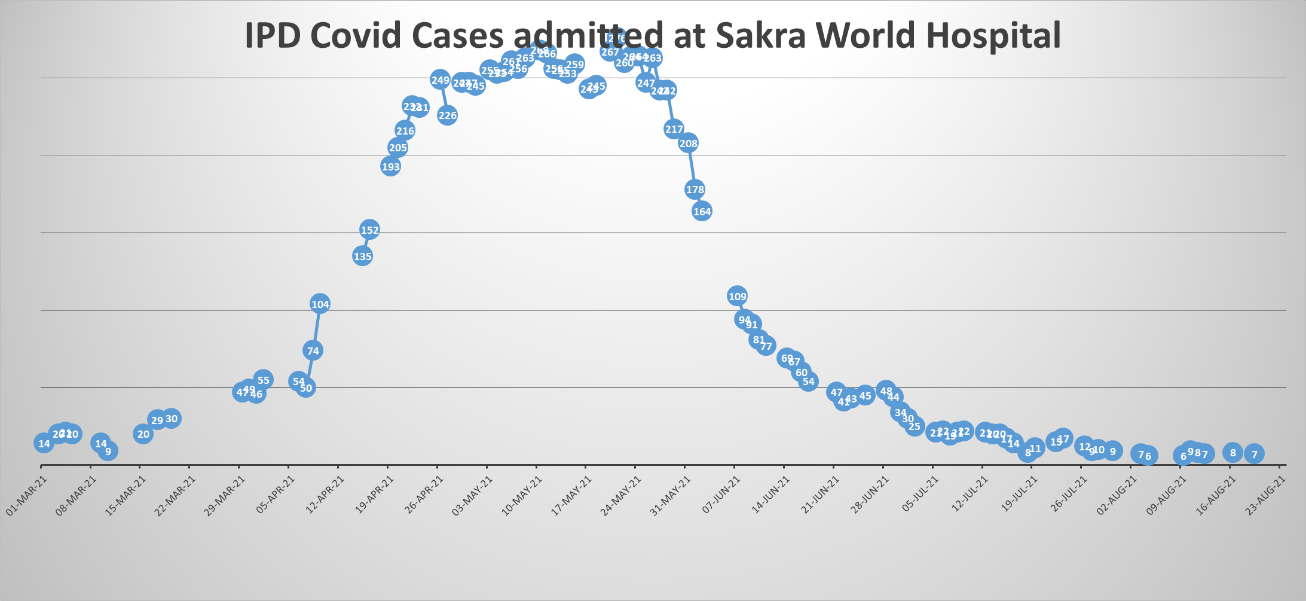
Sakra World Hospital, Bengaluru is tertiary care hospital has 300-bed capacity. During the mid of April 21 till the first week of Jun 21 COVID-19 cases increased drastically as shown in the graph. The average length of patients too increased from 4 to 7.1 day on account of COVID-19 patients thereby creating a shortage of bed availability for the needy patients. The resources required to serve increased COVID-19 patient load was challenging especially materials and equipment.
Graph showing pattern of inpatient COVID 19 patient at Hospital
The COVID 19 pandemic mainly affects patient lungs. The necessity of oxygen and usage of a mechanical ventilator, CT scanner becomes the need of hour during this pandemic. The medical equipment management had become a major focus during COVID 19 time especially for patient treatment and recovery like mechanical ventilator & BIPAP units. This article is highlighting how in peak COVID-19 pandemic situation hospital team has tried to tackle the shortage of intensive care beds wherein patients required a mechanical ventilator.
Waiting for ventilator for the needy patient, Unnecessary motion of staff, rework of staff to connect patient circuit on ventilator and delayed transportation are MUDA (waste) which compromised or delayed patient who needed ventilator in a hospital. The location of Intensive care is scattered across the high-rise building and managing timely usage of ventilators in required ICU was a real challenge for the hospital COVID-19 task force.
Although hospital had 50 % Intensive care units (ICU) beds having mechanical ventilator, with a surge in COVID-19 especially in May & June 21, there was sub-optimal utilization of Ventilators at the start of the second wave of COVID 19 pandemic. Before the start of Covid pandemic medical equipment in general and ventilator, BIPAP, in particular, were allotted to various ICU & wards based on user requirements. To make transfer equipment from one area to another, there was a due delay since approval at various levels were required. The time to shift from one ICU to another ICU involved a lot of paper work and was time-consuming. Due to the possibility of essential elective surgery, there was need to keep few ventilators on standby mode. Unfortunately, no team either nursing, medical administration, or clinical engineering was owning the responsibility to this critical process of timely resource sharing and quickly utilizing on needy patient.
The repeated delay in ventilator shifting and undue escalation of this problem at various levels led to a discussion at COVID 19 task force meeting. After analyzing the root cause of lack of ownership for the medical equipment transfer & tracking process, the management had given both authority and responsibility to the Associate Vice president (AVP) to take lead and quickly adopt a workable solution for the best utilization of equipments, especially ventilator.

Table showing 5 Why analysis conducted by Hospital quality team to understand root causes for sub optimal ventilator utilization
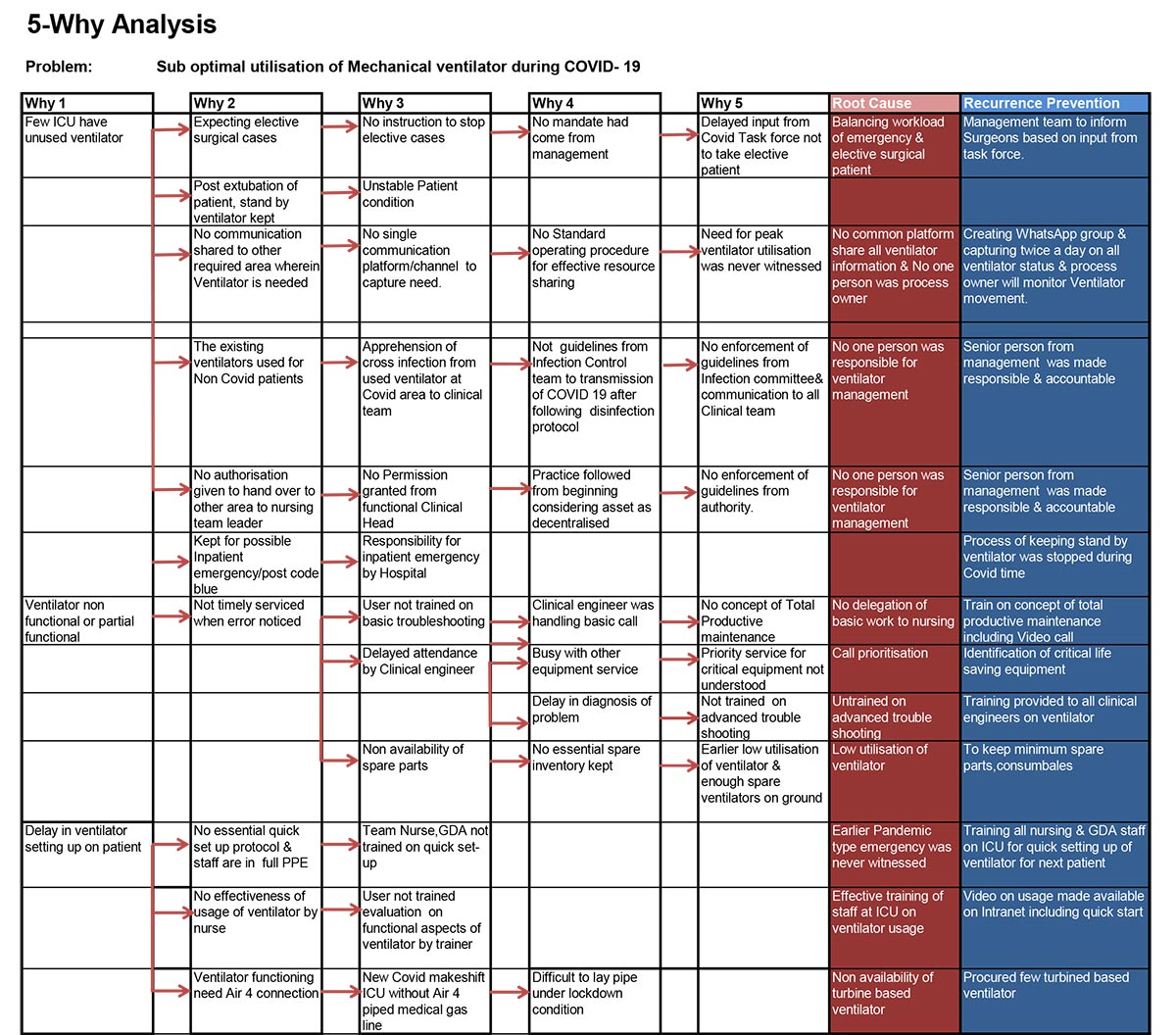
The Hospital quality assurance team to understand root causes for sub-optimal ventilator utilization with help of all stakeholders through 5 WHY analysis tool and recommended to have senior management member as process owner for Ventilator management.
The following improvement ideas were adopted by Associate Vice President (AVP) with help of COVID-19 task force for a better, quick change over of ventilator without compromising on the uptime of equipment.
- Total productive maintenance (TPM) concept was adopted through training all Clinical engineers on troubleshooting on COVID 19 related critical equipment.
- The critical spare parts, accessories needed for equipment were procured extra and kept in the hospital without waiting for supply chain lead time.
- The user group was trained on identifying error codes and communicating to the Clinical engineer through phone or video calls.
- The cleaning & disinfection of equipment based on OEM protocol was strengthened to reduce the risk of spread of COVID 19 through Ventilator and its accessories. Maximum disposable items were being used like patient circuits and special precautions were taken to disinfect parts that come in contact with patients like flow sensors.
- Most of the troubleshooting was resolved by the Clinical engineering team remotely and only for absolute need, engineer used to enter COVID 19 area with a proper protection kit.
- The instruction manual, service manual, and video on operation of equipment were uploaded in Hospital Intranet for ready reference.
- SMED (Single Minute Exchange of Dies) concept of LEAN Manufacturingmethod was adopted to reduce the time required to change over equipment like ventilator from one patient to another.
- The biggest challenge was ensuring that unused equipment is quickly moved to the required area without delay as there was a tendency of holding equipment in a specific area in anticipation of its need for any patient. This is also more pertaining to those areas wherein they expected surgeries may happen to result in possible ventilator needs.
- The closed social media group was created which included intensivist, surgeon, nursing and Clinical Engineering team. Twice in day, the status of areawide ventilators physically present, on use on patient and in stand by mode for patient besides ventilator needing maintenance was shared in closed group.
- On a daily basis the location-wise equipment availability, its usage was closely monitored by Associate Vice President with help of biomedical engineer and nursing staff.
- The care was taken to avoid mixing of a ventilator in the COVID-19 area from the non-Covid area although disinfection protocol was followed as per OEM norms.
- With still elective surgeries and emergency surgeries performed at hospital, few ventilators were in standby mode. This issue was addressed with the clinical team through sharing stand-by ventilators among various clinical specialties.
- Based on ventilator patient surge in number, an additional set of ventilators were quickly procured and installed. A mix of ventilators turbine-based (without compressor gas input) and other one took for flexibility in usage across the hospital as few ward beds were converted to ICU capabilities but without central compressed airlines.
- The ventilator modes of application were refined based on patient critical condition. The monitoring also involved is a ventilator in invasive or non-invasive mode to ascertain possible replacement of BIPAP exchange of ventilator based on the advice of intensivist.
- The decision to shift the ventilator from one area to another was purely based on patient clinical requirements.
- During the last few weeks of the 2nd wave of COVID 19, there was an increase in the need for patients who have recovered from COVID-19 but still needing assistance of mechanical ventilation in the Non-Covid area.
- After due diligence with the anesthesia team and service providers, an anesthesia ventilator was used for a few patients to address the shortfall of the mechanical ventilators.
The result was evident as there were only two breakdowns on ventilators with 0.1 % downtime and needless to say that there was maximum 100 % utilization of equipment with quick changeover from one patient to another. The transparency in the usage of ventilators resulted in no unnecessary row among stakeholders. Needless to say, precious lives of patients were saved through the Lean concept to tackle MUDA i.e. waste of rework, motion, transportation and waiting.
The following lessors were learned during this 2nd COVID 19 wave pandemic with respect to asset management.
- The equipment management process can’t be viewed in isolation by Clinical engineering, nursing, clinician. Cross-functional coordination is necessary as hospital processes curt across barriers of functional departments.
- Asset sharing at the shortest time is mandatory. The hospital is decided to adopt centralized medical equipment storage and distribution.
- The hospital had noticed that since their existing ventilators needed Air 4 bar for its function, in quick time intervals it was difficult to commission the existing area to ICU as a pipeline for Air 4 needed to be laid. It is better to have a combination of turbine-based ventilators along with current set of ventilators.
- Virtual training & maintenance is a way forward for user groups and clinical engineers.
- Systematic planning and procuring of inventory and strict infection control practice gives dividends of improving uptime and safety to patients & staff.

The experience of the best usage of the life-saving ventilator with minimum downtime and quick transfer and connection to the required patient by trained staff taught hospital team that Kaizen i.e. continuous improvement in process based on demand is best way to improve the quality of patient care and improve. The Kaizen can be only achieved through the application of thinking hats from various stakeholders and executed under able process owner.