Ultrasound Journal 19 - The Role of High-frequency Ultrasound in the Diagnostics of Nevus
By Dr. Ivanovskaya Yulia PhD, 2023-10-10
Special thanks to Dr. Ivanovskaya Yulia PhD, Head of Medical Research Department Novacutan for sharing this case.
Introduction
Currently, all available diagnostic tools in cosmetology (noninvasive) allow you to assess the condition of the dermis based on a visual assessment of the data obtained through photographs, dermatoscopy, etc. These methods do not allow to obtain information about the depth of a particular skin formation, instrumentally evaluate the condition of soft tissues [1].
High-frequency ultrasound (HFUS) is a technique used in skin science. It shows real-time images of skin layers, appendages and skin lesions in vivo and can make a significant contribution to skin science. These clinical cases summarize the potential applications of HFUS in dermatology and cosmetology with an emphasis on quantitative tools that can be used to evaluate various skin conditions. This method may eventually become essential for evaluating the effectiveness of dermatological and cosmetic treatment.
Case 1
Dermatoscopic examination
melanocytic nevus of 5.8x7.4 mm, globular structure (intradermal nevus) (Figure 1).

Ultrasound examination
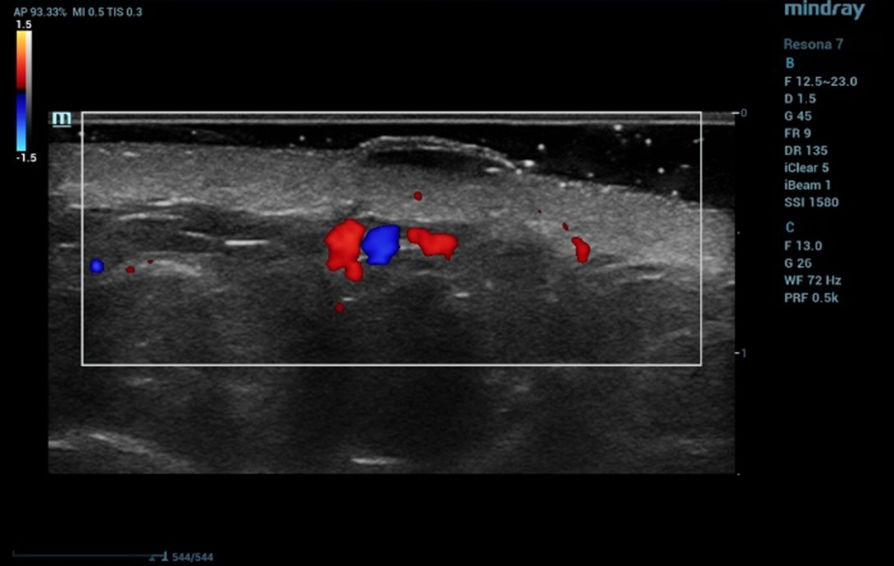
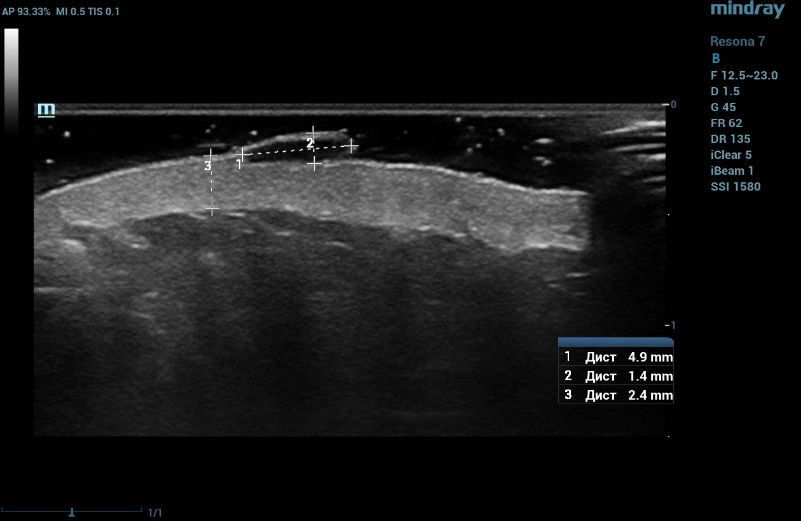
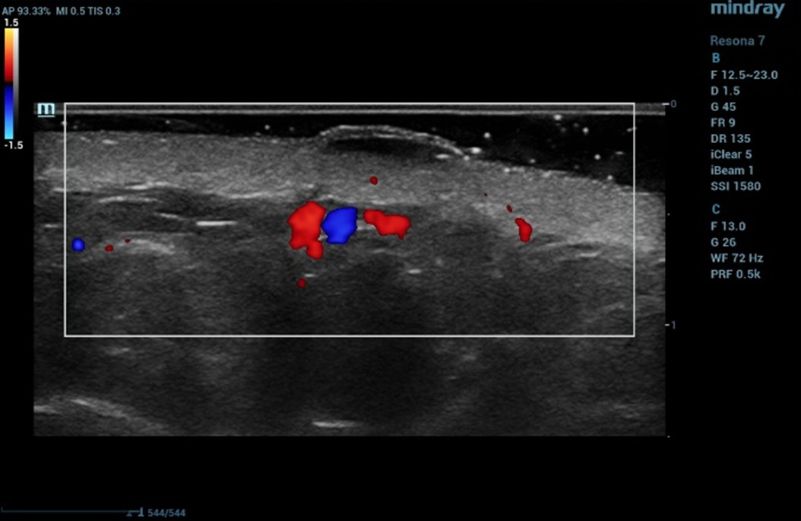
Ultrasound examination of the nevus was performed on the Resona 7 ultrasound machine (Mindray, China) using the high frequency linear transducer L20-5U (max frequency 23 MHz). When the transducer was placed in the projection of the visible nevus of the right zygomatic region of the face, the derma was locally thickened to 2.4 mm due to a hypoechogenic mass located under the epidermis and slightly elevated, spreading in depth to all layers of the dermis with clear rough boundary of heterogeneous echogenicity, without hyperechogenic sports, giving a weak acoustic darkening of the echo signal (Figure 2). Blood flow is not registered inside the nevus in the Color Doppler mode (Figure 3).
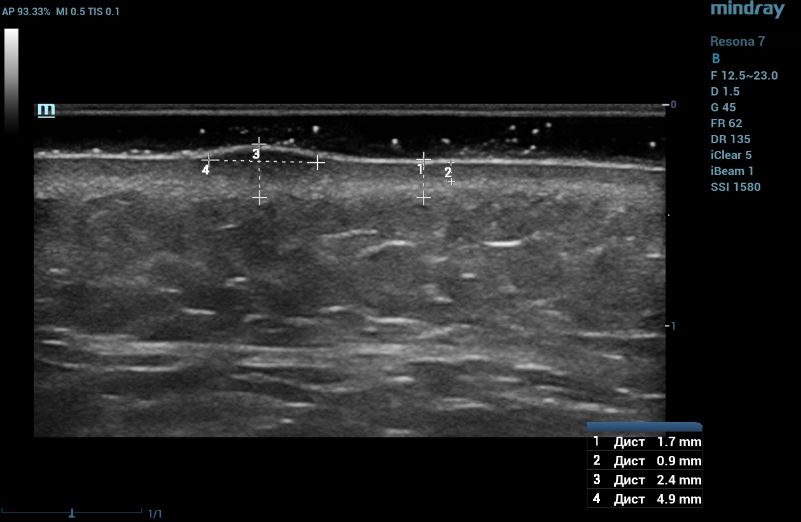
Such ultrasound signs are characteristic of compound nevus [2]. A pronounced subcutaneous low-echo band (SLEB) attracts attention (0.9 mm – 50% of the total thickness of the dermis – 1.7 mm), which is the ultrasound sign of facial skin photodamage [3].
Case 2
Dermatoscopic examination
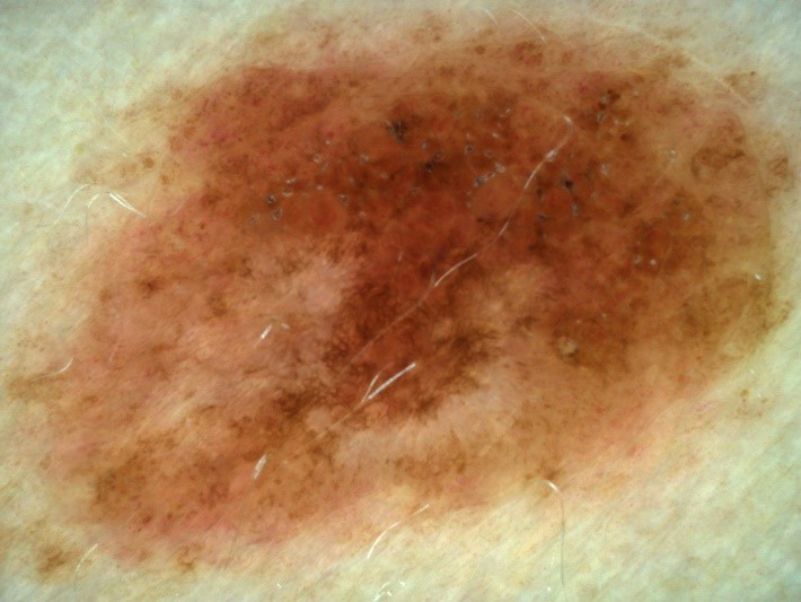
melanocytic nevus 14.1x9.4 mm, globular structure (congenital intradermal nevus) (Figure 4).
Ultrasound examination
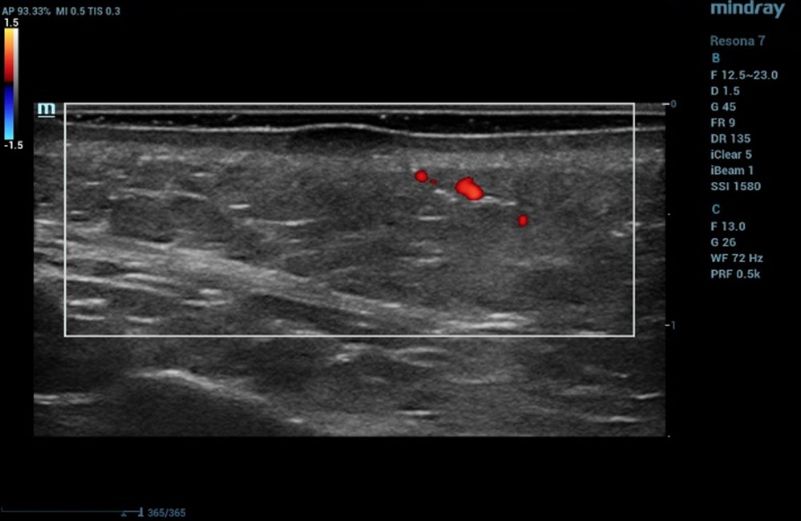
Ultrasound examination of the nevus was performed on the Resona 7 ultrasound machine (Mindray, China) using the high frequency linear transducer L20-5U. When the transducer is placed in the projection of the visible nevus of the left lateral surface of the anterior abdominal wall, an anechogenic oval-shaped mass, located under the epidermis, significantly protruding above the surface and deforming the epidermis outward, with clear even bounds, homogeneous echogenicity, without spreading into the dermis in depth, is visualized. The dermis is homogeneous with increased echogenicity (Figure 5). Blood flow is not registered inside the nevus in the Color Doppler mode (Figure 6).
Discussion
Сurrently, dermatoscopic examination is the "gold standard" in diagnostics of skin formations. It requires extensive experience and imaging skills on the part of the physician, while being limited in its ability to assess the depth of penetration/spread of the mass into the skin [1].
A lot of patients with cosmetic considerations seek for non-surgical treatment of the melanocytic nevus (MN) lesions, such as laser ablation, cryotherapy, and electrodesiccation to avoid the postsurgical scar formation [4]. Generally, dermatologists would empirically apply these therapies for once or limited times to MN lesions with small size (usually<6mm in diameter), flat shape, and no signs of malignancy. But the recurrence and residual pigmentations are often encountered, perhaps due to inadequate intensity and depth of these destructive methods or mis-judgement for MN subtypes. Junctional nevi with small and flat lesions are more sensitive to treatment, while intradermal and compound nevi with larger and deeper lesions are difficult to remove without recurrence the detailed HF-US features of MN lesions with different subtypes and might assist the dermatologists to classify MN subtypes, select, and apply treatments more accurately [2].
High-frequency linear probes (scanning frequency 15-23 MHz) allow to estimate noninvasively in vivo the degree of photodamage of skin, to build an individual treatment protocol and to estimate in dynamics the results of performed cosmetic correction [5].
Conclusions
The HF-US and dermoscopic evaluation of MN in subtype differentiation for the first time and proved that these two methods had a good consistency, implying that the combination of them could provide accurate and objective information for MN classification from both vertical and horizontal perspectives [2]. In cosmetology practice it is a unique opportunity for instrumental non-invasive assessment of derma condition. A lightweight transducer with a small aperture is convenient for examination, which avoids excessive compression on tissue and ensures accurate positioning in difficult for acquisition anatomical areas of face (such as the nasolacrimal trough) – this provides optimal conditions for scanning and measurements.
Reference
[1] Habif T, Dinulos J, Chapman D, Zug K. Skin disease: Diagnosis and treatment. 4th ed. Elsevier; 2018: 18-25
[2] Yu-Kun Wang, Yuan-Jing Gao , Jie Liu, Qing-Li Zhu, Jun-Cheng Wang, Jing Qin , Hong-Zhong Jin A comparative study of melanocytic nevi classification with dermoscopy and high-frequency ultrasound. Skin Res Technol 2022 Mar;28(2):265-273
[3] Gniadecka M, Gniadecki R, Serup J, Søndergaard J. Ultrasound structure and digital image analysis of the subepidermal low echogenic band in aged human skin: diurnal changes and interindividual variability. J Invest Dermatol. 1994;102:362–5
[4] Robert L. Bard. Anatomy of the Face for Cosmetic Purposes. In: Wortsman X, Jemec GBE (eds). Dermatologic Ultrasound With Clinical and Histologic Correlations. 1st ed. New York, NY: Springer; 2013:357–372
[5] Sardana K, Chakravarty P, Goel K. Optimal management of common acquired melanocytic nevi (moles): current perspectives. Clin Cosmet Investig Dermatol. 2014;7:89–103
