Ultrasound Journal 20 - Features of Subcutaneous Venous Port Systems Implantation Using Ultrasound Marking and Ultrasound Navigation
2023-11-24
Special thanks to Prof. Buidenok Y. V. for sharing this case. He is from the Interventional Radiology Department of the Federal State Budgetary Institution «N.N. Blokhin National Medical Research Center of Oncology» оf the Ministry of Health of the Russian Federation.
Antitumor therapy in cancer patients can last for many years. During intravenous administration of antitumor drugs, major complications may arise due to their irritant and cutaneous-penetrating effects and are manifested by extravasation and phlebitis. These complications are accompanied by severe pain syndrome, disrupt the planned scheme of anti-tumor therapy, cause anxiety in the patient and create additional burden on the medical staff [1,2,3]. The optimal solution to the problem of long-term infusion therapy of cancer patients is the implantation of a port system in the superior vena cava, which eliminates the above problems due to high linear and volumetric velocities of hemodynamics.
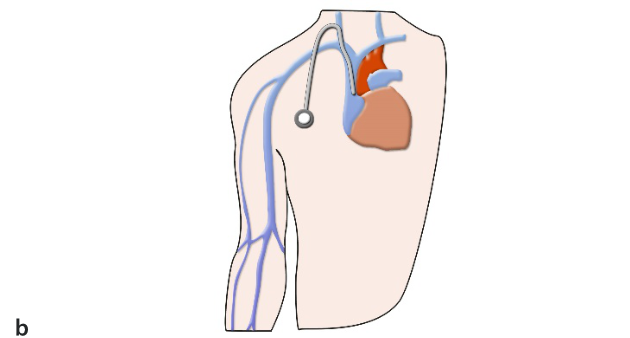
Also, the long-term access system should not significantly affect the patient's quality of life, so the catheter should enter the venous vessel smoothly (without sharp angles and loops), which prevents kinks and strong tension of the catheter when moving in the neck and shoulder girdle causing deterioration of catheter patency, pronounced discomfort and, even pain when the patient moves. A schematic representation of long central venous access devices is shown in Fig. 1.
Currently, the catheter insertion through the subclavian vein is abandoned due to the high probability of severe complications. The most frequent one is catheter impingement between clavicle and first rib with pinch off syndrome (with permeability failure, catheter damage or detachment with fragment migration into the heart cavity). The use of ultrasound monitoring during subclavian vein puncture is also limited [4].
Ultrasound-guided jugular vein puncture provides confident visualization of the neurovascular bundle, allows continuous observation of the process, but requires additional resources - assistant time and consumables (sterile sheath, sterile gel). Visualization of the jugular vein does not cause any problems. But on many mid-level devices it is difficult to visualize the puncture needle, and the needle must be guided by traction of the surrounding tissues. Experienced surgeons often use ultrasound-guided preoperative evaluation and marking the projection of the jugular vein on the skin.
There are several advantages with this method: preliminary assessment of the vessels is performed, the method does not take much time, sterile technology is not required, puncture is performed with both hands of the surgeon, in small children the degree of freedom of manipulation is improved, with a puncture needle. Therefore, the use of ultrasound marking is very popular when inserting venous access systems through the jugular vein. Considering that the main neurovascular bundle of the neck consists of the internal jugular vein, common carotid artery, deep lymphatic cervical nodes and vagus nerve, sometimes we must face complications in the form of unintentional carotid puncture with development of massive hematoma and failure to install the catheter in the selected area.
Let us analyze the causes of these complications using a clinical example:
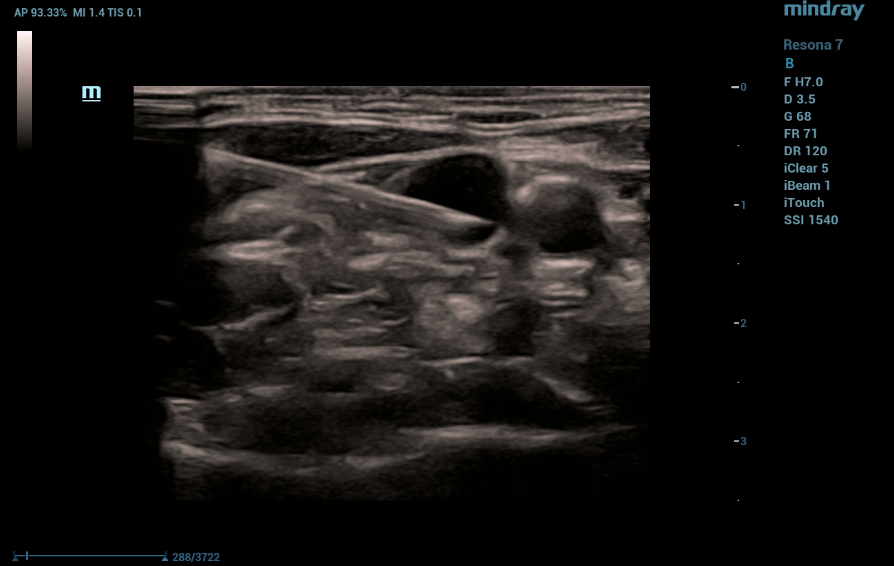
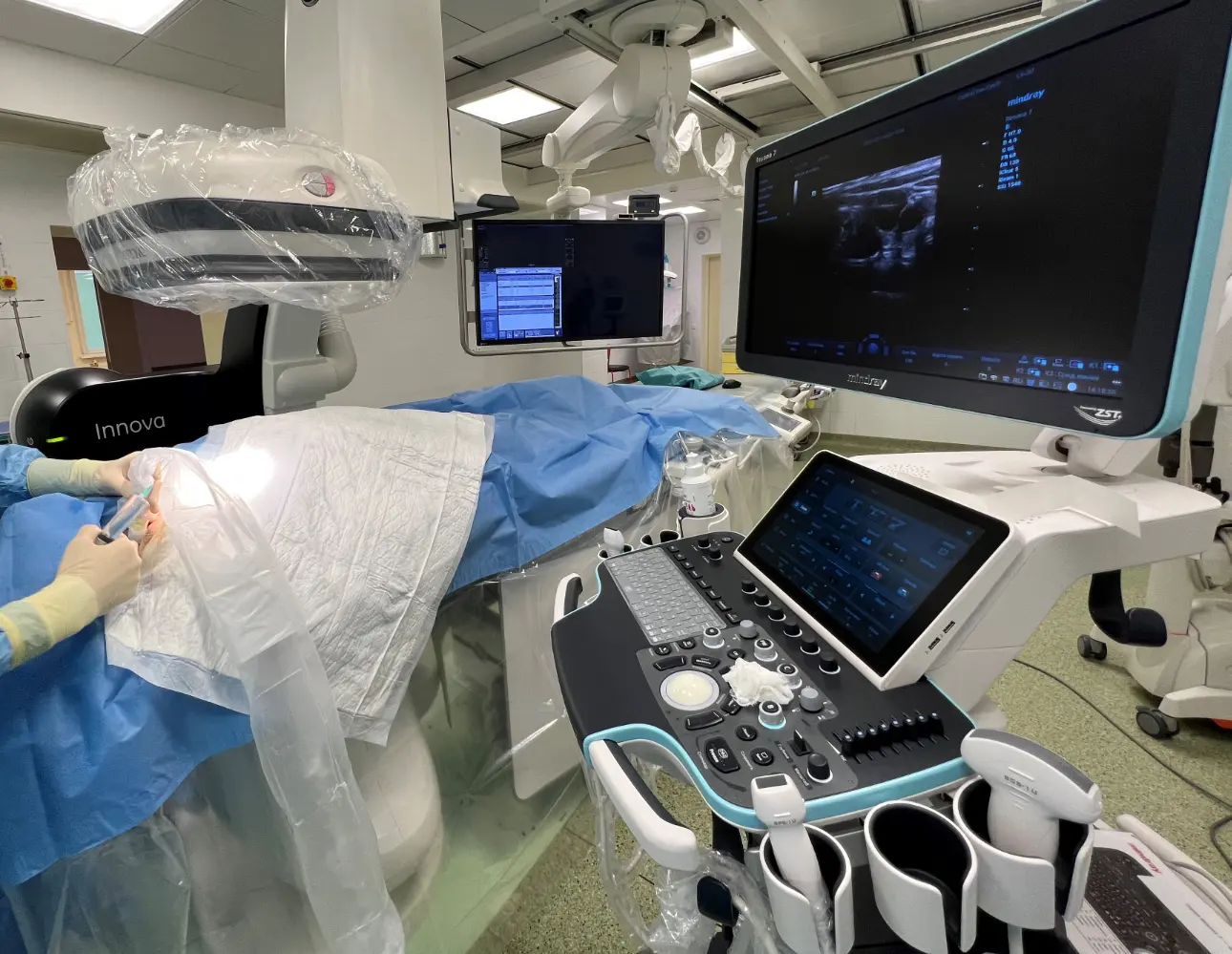
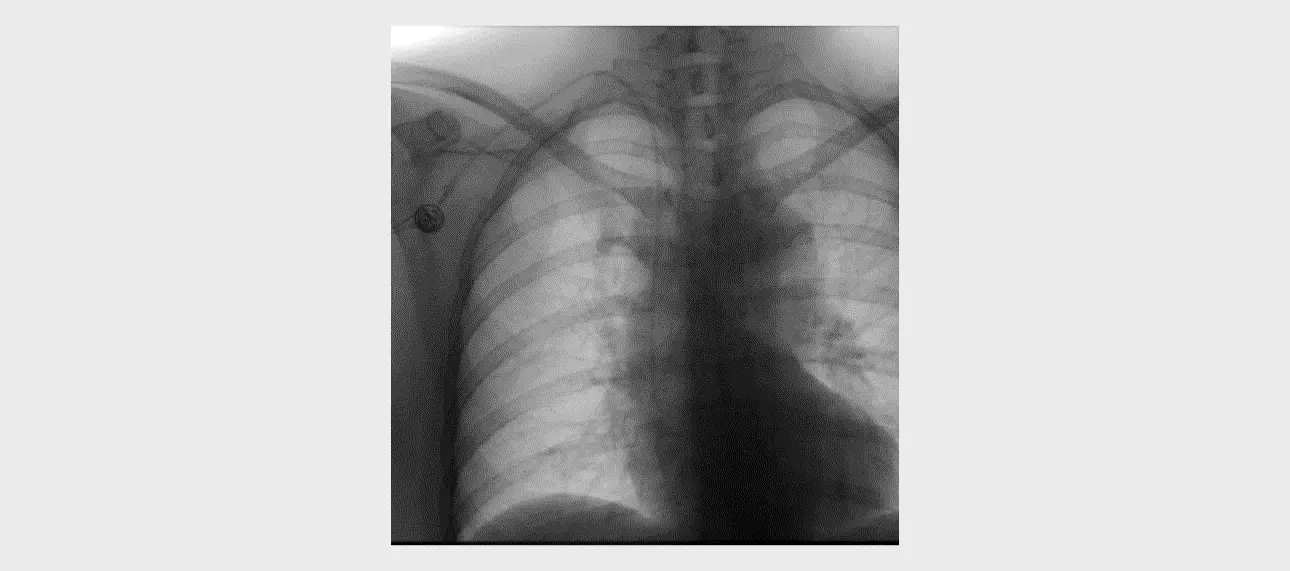
The patient is a woman, 48 years old. She was admitted to an oncology hospital for FOLFOX antitumor treatment, diagnosed with cancer of the stomach antrum pT3N1Mo stage IIB: Before chemotherapy, implantation of a port system with insertion of a catheter through the right subclavian access was indicated. Right jugular vein puncture was performed under ultrasound guidance. The investigations were performed on a Mindray Resona7 expert-class ultrasound machine with a cine recording.
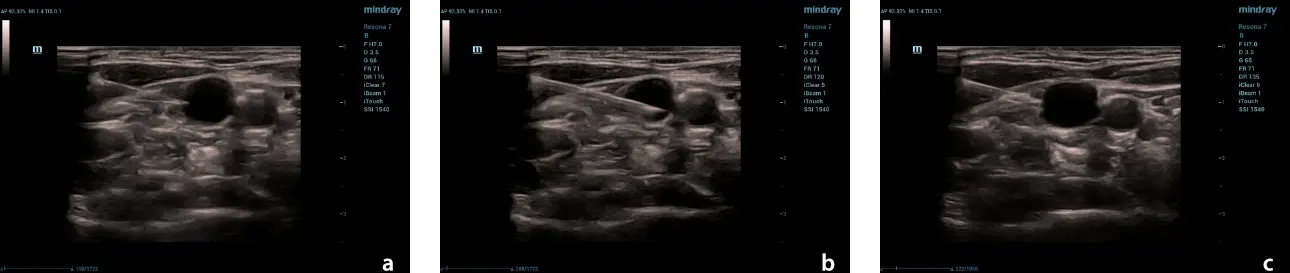
As a result of good visualization of the vein and needle, the puncture was successfully performed, followed by implantation of a saphenous venous port system.
Discussion
The use of an ultrasound machine allows preoperative evaluation of the neck vessels and, with experience, successful puncture after preliminary ultrasound imaging and marking. Performing a puncture with ultrasound navigation allows the procedure to be performed with the greatest accuracy and real-time monitoring to avoid complications such as unintentional carotid puncture.
References:
[1]. Buidenok Y. V. Recommendations for the treatment of the consequences of extravasation of antitumor drugs. Malignant Tumors: Practical Recommendations RUSSCO #3s2, 2020 (Vol. 10). С. 156–162.
[2]. Kim T. J.., Park J. Y., Lee H.J., Cheon J. Y. Guidelines for the management of extravasation J Educ Eval Health Prof. 2020;17:21. DOI:10.3352/jeehp.2020.17.21. Epub 2020 Jul 16.
[3]. NSH Network Guidelines for the Management of Extravasation of a Systemic Anti-Cancer Therapy Including Cytotoxic Agents (2017, England)
[4]. Pinch-off syndrome Jin-Beom Cho 1, Il-Young Park, Ki-Young Sung, Jong-Min Baek, Jun-Hyun Lee, Do-Sang Lee. Affiliations expand. PMID: 24020024. PMCID: PMC3764366. DOI: 10.4174/jkss.2013.85.3.139