In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Case Introduction
A 49-year-old male patient complained of fever without obvious predisposing factors and was diagnosed with subacute infective endocarditis, sepsis, grade 1 hypertension, type 2 diabetes mellitus, and lung infection.
Disease Progression
At 12:30 p.m. on that day
The chief physician of the department performed a round and found that the patient’s body temperature was 37.7°C and heart rate was 100 beats/minute. Blood pressure was maintained at 118/79 mmHg with norepinephrine 1.33 ug/kg/min + terlipressin. A blowing murmur was heard in the auscultation area of the mitral valve and the first auscultation area of the aortic valve. As directed by the chief physician, the patient was currently hemodynamically unstable and might be at risk of distributive shock.
At 10:28 p.m. on the same day
The patient’s heart rate began to increase, and the ECG monitoring waveform showed a supraventricular arrhythmia waveform. At the same time, the patient’s respiratory rate also gradually increased, the invasive blood pressure decreased rapidly within minutes, and the systolic blood pressure decreased to below 90 mmHg.

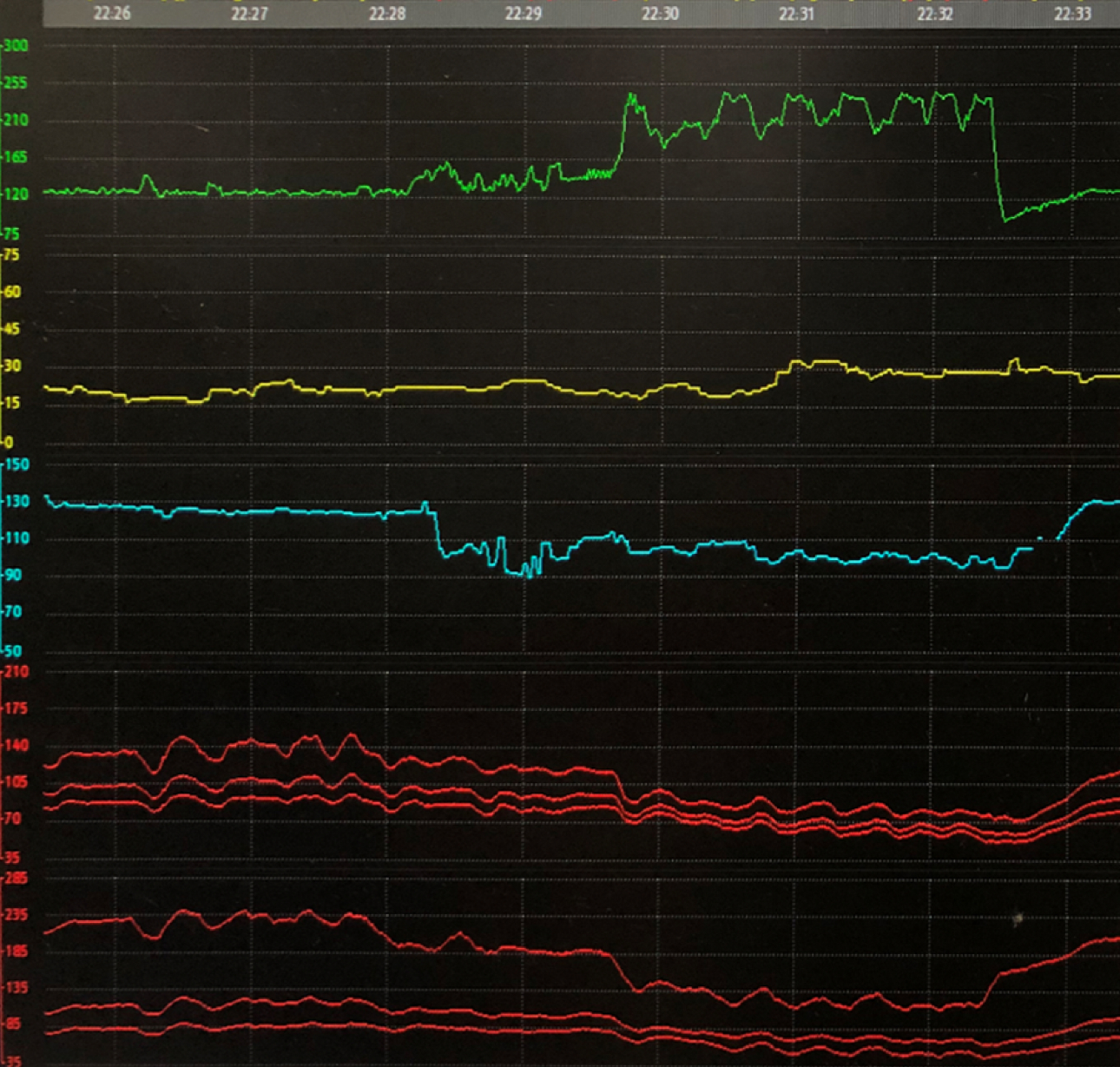
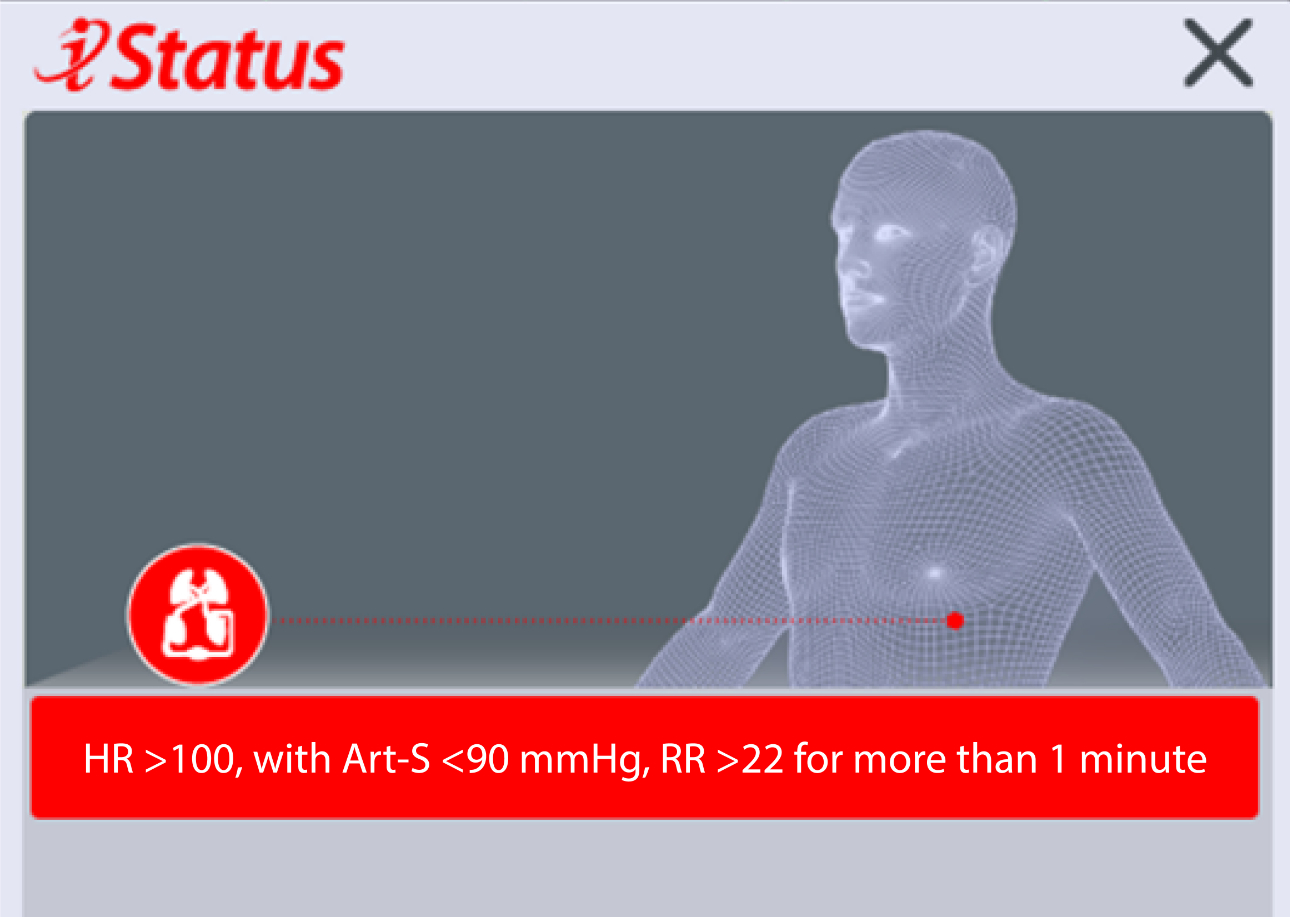
Changes in the patient’s physiological state triggered the status alarm of shock state deterioration of the Mindray monitor “HR >100, with Art-S <90 mmHg, RR >22 for more than 1 minute”, and the iStatus interface reminded the clinician of the changes in the hemodynamic state of the patient in the form of intuitive images.
The nurse called the doctor after seeing and confirming the authenticity of the alarm.
The doctor made a quick judgment on the patient, chest compressions were immediately initiated and amiodarone was intravenously infused via a micropump for antiarrhythmic rescue therapy. At the same time, three Art <90 synchronized cardioversions at 150 J were performed at 10:30 p.m., 10:35 p.m. and 10:38 p.m., respectively.
As a result of the timely rescue, the patient converted to sinus rhythm at 10:39 p.m., his blood pressure returned to 113/73 mmHg and oxygen saturation was 98%, indicating the rescue was successful.
Case Analysis
At the time of admission to the ICU, the patient was diagnosed with a variety of diseases. During the round at noon on that day, the doctor judged that there was a probability of disease progression and distributive shock, such as septic shock. For such patients, how to detect the patient’s deterioration as soon as possible and intervene in a timely manner has always been an area of clinical concern.
In fact, many clinical studies have explored the prediction of the progress of shock status in patients, including heart rate, respiratory rate, and arterial blood pressure. Levi D. Procter, a well-known expert in the field of shock treatment and professor at the University of Kentucky College of Medicine, pointed out in the “MSD Manuals” that multiple indicators of patients should be analyzed in combination for shock diagnosis and prediction.
The patient’s condition deteriorated at 10:30 p.m., which was a period with fewer medical staff. Before the alert message of “HR >100, with Art-S <90 mmHg, RR >22 for more than 1 minute” was triggered, due to the setting of the alarm limits for heart rate and blood pressure, the deterioration of vital signs did not trigger high-level alarms, and the only medium-level alarm was triggered for arterial blood pressure and respiratory rate that reached the single-parameter thresholds. In clinical practice, the occasional single-parameter medium-level alarm is often regarded as a fluctuation by nurses and cannot get enough attention.
Based on the Mindray monitor, the triggering of the status alarm message and the presentation of the visualization of the patient status guide interface allow clinicians and nurses to quickly and accurately identify the deterioration of the patient’s status and take clinical intervention measures. This is also the best use of the alarm value of the bedside monitor.
References
[1] Chen, W.‐L. and Kuo, C.‐D. (2007), Characteristics of Heart Rate Variability Can Predict Impending Septic Shock in Emergency Department Patients with Sepsis. Academic Emergency Medicine, 14: 392-397.
[2] Parker MM, Shelhamer JH, Natanson C, Alling DW, Parrillo JE. Serial cardiovascular variables in survivors and nonsurvivors of human septic shock: heart rate as an early predictor of prognosis. Critical Care Medicine. 1987 Oct;15(10):923-929.
[3] Loughlin P C, Sebat F, Kellett J G. Respiratory Rate: The Forgotten Vital Sign—Make It Count![J]. Joint Commission journal on quality and patient safety, 2018, 44(8): 494-499.
[4] Gernardin G, Pradier C, Tiger F, et al. Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock[J]. Intensive care medicine, 1996, 22(1): 17-25.
[5] https://www.merckmanuals.com/professional/critical- care-medicine/shock-and-fluid-resuscitation/shock

