In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Background
Enhanced Recovery After Surgery (ERAS) is a new concept that has emerged in recent years, which refers to the use of various effective methods to guide and adjust the patients both physically and psychologically before, during and after surgery. These methods are to reduce stress complications after surgery or during treatment, helping the patients maintain a good mental state, and reduce postoperative complications, such as postoperative bleeding, lung infection, delayed wound healing, deep vein thrombosis, etc.
According to the amount of exercise required by clinical ERAS (under the premise of meeting risk prevention and control), patients are encouraged to complete daily customized activity goals, such as off-bed mobilization on Day 1 after surgery for 1 to 2 hours, and getting out of bed for 4 to 6 hours every day at the time of discharge.1
Therefore, how to ensure patients’ safety during the exercise and how to enable patients to ambulate safely? Continuous and uninterrupted vital signs monitoring is the key.
Mindray ePM wearable monitoring system provides physiological parameter monitoring for patients’ early off-bed mobilization after surgery, comprehensively assists in medical decision making, and better postoperative rehabilitation management.
Case Introduction
A 55-year-old male patient was diagnosed with “malignant liver tumor” more than 4 years ago. He underwent TACE surgery twice in 2016 and 2017 respectively, the process of surgeries went smoothly, and the postoperative recovery was acceptable. A re-examination was performed again, and the outpatient department admitted the patient to the hospital for a follow-up examination after malignant liver tumor surgeries.
Examination after admission
1. Contrast-enhanced MRI of upper abdomen Liver
After 2 TACE surgeries for liver cancer, a nodule with enhancement was observed in segment CIII of the liver, which was considered as tumor recurrence, and the nodule was new as compared to the previous MR image.
2. Hematology test
White blood cell count: 13.52*109/L; neutrophil count: 10.42*109/L; red blood cell count: 2.72*1012/L;
3. Liver function test
Total protein 55.6 g/L; albumin 32.3 g/L; alanine aminotransferase 99 U/L; aspartate aminotransferase 129 U/L;
4. Four-item infectious disease test
Hepatitis B surface antigen (+); Hepatitis B core antibody (weakly positive)
Diagnosis
- Malignant liver tumor
- Cirrhosis
- Portal hypertension
- Liver nodule
Surgical Records on May 23, 2021:
Operations:
- Laparoscopic right hepatectomy
- Ligation of communicating portal vein branches
- Bile duct repair
- Middle hepatic vein repair
- Intestinal adhesiolysis
- Cholecystectomy
Postoperative Diagnosis:
- Malignant liver tumor
- Interventional treatment for malignant liver tumor
- Cirrhosis
- Portal hypertension
- Left simple renal cyst
- After splenic surgery
After the surgery, the patient was transferred from PACU to ICU.
Clinical data shows that various complications such as bleeding are prone to occur after hepatectomy for liver cancer, with an incidence of 1% to 8% and a mortality rate of 17% to 80% respectively. 48 hours after surgery is the peak period of postoperative adverse events in patients. If the occurrence of adverse events such as hypoxia, arrhythmia, hypotension, or hypertension in the patients cannot be identified in time, it may cause delays in treatment or rescue and it is not conducive to the recovery of the patients. Therefore, continuous vital sign monitoring is a safety guarantee for patients to get out of bed early after surgery.
Uninterrupted monitoring of vital signs
In order to monitor and control the status of the patient’s vital signs in real time, the medical staff helped the patient put on the Mindray ePM wearable monitoring system which is connected to the central monitoring system via the network. The medical staff could check the patient’s status anytime anywhere.

Return to the ward safely
0h - 6hrs
The patient’ s vital signs were continuously monitored.

After 6hrs
Got out of bed for mobilization and exercised for 1-2hrs according to the doctor’s advice and ERAS principles.
7: 05 a.m.
Got out of bed and started trying to walk slowly.

7:25 a.m.
The patient’s heart rate gradually increased from 102 bpm to 150 bpm. The nurses’ central monitoring station (CMS) and the doctor’s handheld Mobile Viewer received the patient’s increased heart rate event alarm, and the nurse in charge immediately went to check on the patient.
The patient reported rapid heartbeat without palpitation or chest pain. The nurse reviewed his SpO2 and blood pressure data during the exercise, no anomalies were indicated, then the patient was instructed to stand still and observe whether the discomfort could be eased.
After a few minutes of inactivity, the patient’s the patient to continue to exercise, and she also advised that the patient to rest until his heart rate was restored when he felt unwell, then go on.

The patient’s heart rate increased to 150 bpm twice while exercising, and the event was relieved after resting. Considering the patient’s poor physical status and unstable heart rate, the patient was recommended to return to the ward to rest, and changes in the patient’s vital signs were closely observed.
48hrs after surgery
As the patient’s condition improved, the medical staff encouraged the patient to gradually extend the exercise within his acceptable range.
Although occasional tachycardia occurred during subsequent exercise, the nurse promptly dealt with it after receiving the alarm to ensure that the patient could exercise safely.
Quantifiable ERAS to assist decision-making
In addition to providing continuous and uninterrupted monitoring of vital signs for the patient, the ePM wearable monitoring system also supports the statistics of patient’s exercise time and rest time, as well as the pain scores and trends. These functions are able to efficiently assist medical staff to intuitively understand the patient’s daily exercise compliance status, sleep status, and the true state of the pain.
Day 1 after surgery
Exercise Time Records:
As mentioned above, there was a safety risk due to the patient’s heart rate fluctuation event, and the medical staff instructed the patient to control the amount of exercise.
It could be seen from the “ERAS Assistant” of the ePM wearable monitoring system that the total exercise duration of the previous day was 50 mins, which did not meet the requirement. Therefore, the patient was encouraged to start extending exercise duration the next day in order to achieve the predetermined goal.
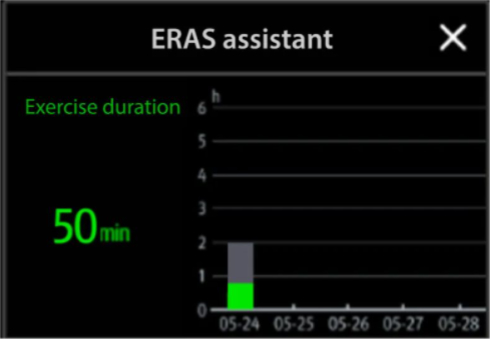
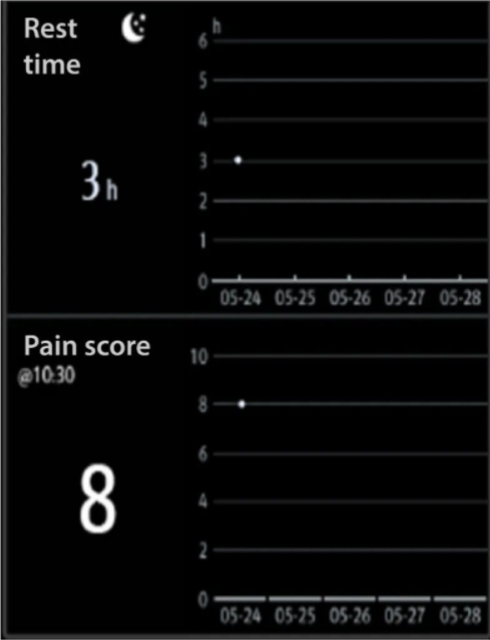
Pain Score And Rest Time Management:
In this case, the patient underwent open hepatectomy, and the postoperative pain intensity was stronger than that of the general open surgery.2 On the same day after surgery, the patient did not get a good sleep at night due to the wound pain.
According to the “ERAS assistant”, the patient had 3hrs of sleep at night and an NRS pain score of 8, which was consistent with the patient’s self-reported sleep and pain.
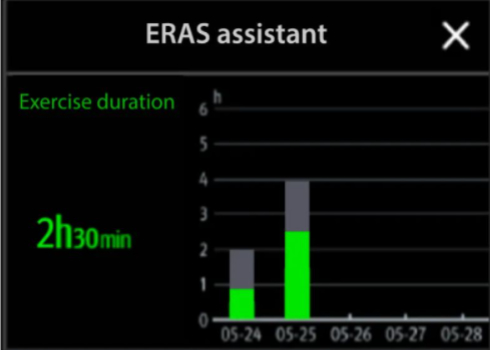
Day 2 after surgery
Exercise Time Records:
The patient’s basic status was improved, his wound pain was relieved than before, and after his physical strength was restored, he continued to exercise while wearing the ePM.
It could be seen from the “ERAS Assistant” that the patient accumulated 2.5hrs of exercise duration on that day and completed the
2-4hrs of exercise goal of the day. There was a significant improvement compared to Day 1. The nurse encouraged the patient to maintain the amount of exercise in the future to strengthen the rehabilitation.
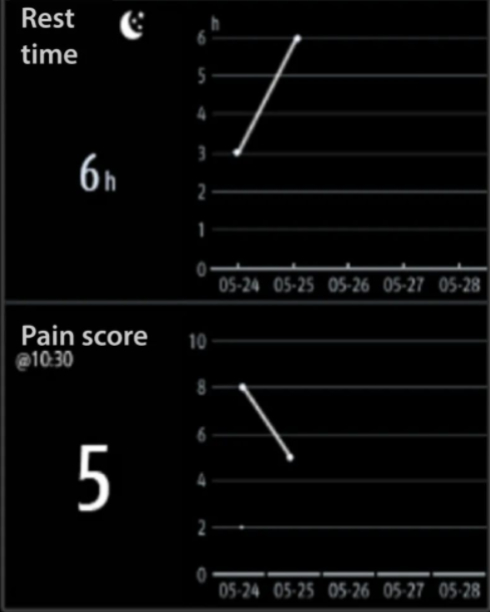
Pain Score And Rest Time Management:
It could be clearly seen from the “ERAS assistant” that the patient’s sleep was improved, his sleep time at night reached 6 h, and his pain score dropped to 5.
The doctor believed that the patient’s rehabilitation process was relatively smooth, so no special treatment was required, but only maintaining observation was required.
ERAS is a perioperative optimization treatment measure with multidisciplinary involvement to achieve the purpose of reducing the occurrence of complications and promoting rapid recovery of patients. Early off-bed mobilization is one of the important measures.
The ePM wearable monitoring system is in line with the ERAS concept, enabling patients to ambulate safely in the early postoperative period, accelerate rehabilitation, as well as improving the turnover rate of departments and the operational effi ciency of hospitals.
Appendix
[1] Anonymous Chinese Expert Consensus on Perioperative Management of Enhanced Recovery After Surgery (2016) [J]. Chinese Journal of Surgery, 2016, 54(006): 413-418.
[2] Li Dawei, Bai Dousheng, Jiang Guoqing, et al. A Study on Multimodal Analgesia after Hepatectomy for Liver Cancer Based on the Concept of Enhanced Recovery after Surgery [J]. Chinese Journal of General Surgery, 2018, 033(008): 704-706.

