You may have heard of hepatitis B and C. While the letters differ, they both have one thing in common — a dangerous inflammation of the liver.

Find the Missing Millions
Viral hepatitis B and C are the second major killer infectious diseases after tuberculosis, causing 1.4 million deaths a year. Out of the 325 million people living with viral hepatitis globally, 290 million — that’s 9 in 10! — are not aware they have it. Unless there is a massive scale-up in screening, diagnosis and medical care, more people will become infected and lives will continue to be lost.

Viral hepatitis B and C, alcohol abuse and non-alcohol-related steatohepatitis can lead to liver fibrosis and subsequently cirrhosis and cancer.
Liver fibrosis is the excessive accumulation of extracellular matrix proteins including collagen that occurs in most types of chronic liver diseases. Over time the extracellular matrix proteins increases, leading to fibrosis with potential progression to cirrhosis. Fortunately this dynamic process is reversible through breakdown of the matrix proteins. Early detection and treatment can prevent it from developing into liver cirrhosis and even cancer.

Liver Fibrosis Diagnosis
The “gold standard” for assessing the liver inflammation stage is liver biopsy. However, it is an invasive procedure with the risk of complications and high variability due to the heterogeneity in disease distribution and inter/intraobserver variations. Noninvasive methods, including indirect biomarkers, direct biomarkers and imaging modalities, are commonly used in clinical practice.
Alanine aminotransferase (ALT) has been widely used as a traditional biomarker for the evaluation of the liver inflammatory activity. However, studies have reported that patients with chronic liver disease with normal or near-normal ALT are not necessarily free from liver damage and require antivirus therapy according to current guidelines. Therefore, more sensitive and accurate biomarkers are needed to evaluate liver inflammation.
Hyaluronic acid (HA), laminin (LN), collagen type IV (CIV), and N-terminal propeptide of type III procollagen (PIIINP) are four major direct biomarkers for the noninvasive assessment of liver fibrosis. They reflect the deposition or removal of extracellular matrix in the liver.
The Third Affiliated Hospital of Sun Yat‐Sen University, China, has conducted a case study on a total of 242 patients with chronic hepatitis B (CHB) who were enrolled in the hospital from October 2012 to December 2017. All patients underwent a liver biopsy and their serum levels of ALT, aspartate aminotransferase, HA, CIV, PIIINP, and LN were quantified by Mindray CL‐2000i Chemiluminescence Immunoassay System.
The results are reported as follows:
TABLE 1 Evaluation of the efficacy of ALT, AST levels, and serum liver fibrosis markers in the diagnosis of significant liver inflammation (≥G2) in patients with CHB.

TABLE 2 Evaluation of the efficacy of ALT, AST levels and serum liver fibrosis markers in the diagnosis of significant liver inflammation (≥G2) in patients with CHB with ALT < 2 × ULN
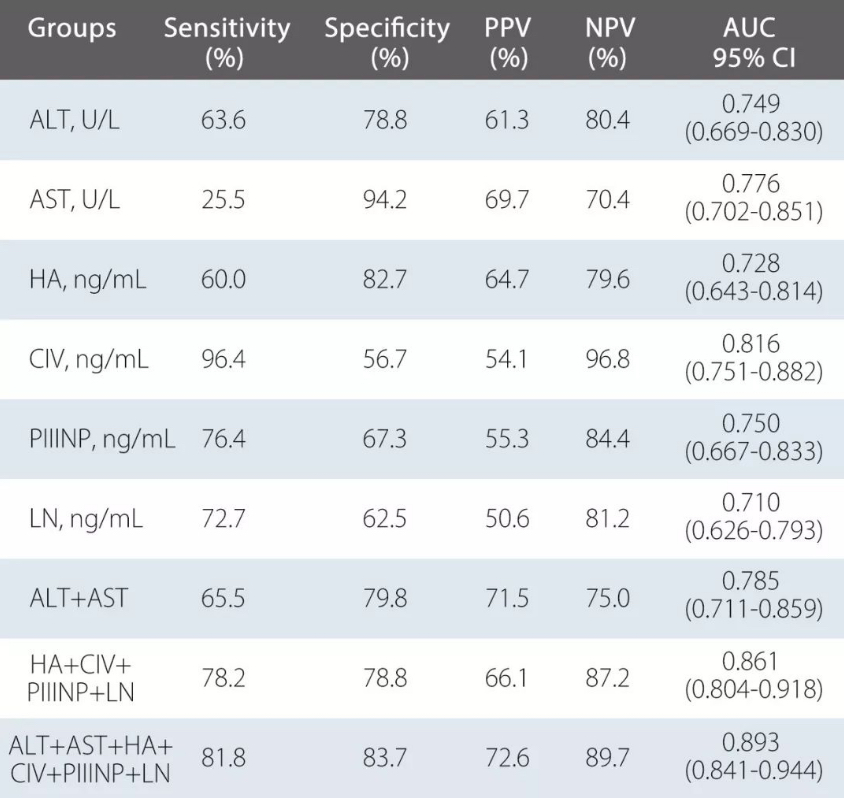
The study has shown that these four markers quantified by Mindray chemiluminescence immunoassay have high diagnostic values for predicting significant inflammation in patients with CHB. In this study, it is also found that a combined index, including the four markers, significantly improved diagnostic performance and achieved excellent diagnostic accuracy in patients with CHB with normal or near-normal ALT levels.

Fighting to Eliminate Hepatitis
WHO’s new analysis shows that hepatitis testing and treatment are high-impact interventions that can help countries accelerate progress towards its elimination.
Stop ignorance and neglect of viral hepatitis – share information about it. Educate yourself and others to learn risks for viral hepatitis, and access testing services.
On World Hepatitis Day 2019, join the cause to help 325 million people.