In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
For critically ill newborns, blood oxygen saturation is one of the most important vital signs in NICU, and it is also the parameter, for which every NICU department requires the highest standard on monitors.
Case Introduction:
A female patient who was delivered at Week 32 of GA with a birth weight of 1.5 kg.
Current Diagnosis:
Neonatal respiratory distress syndrome (NRDS), acute respiratory failure, pneumonia, shock, patent ductus arteriosus (PDA), patent foramen ovale (PFO).
Disease Introduction:
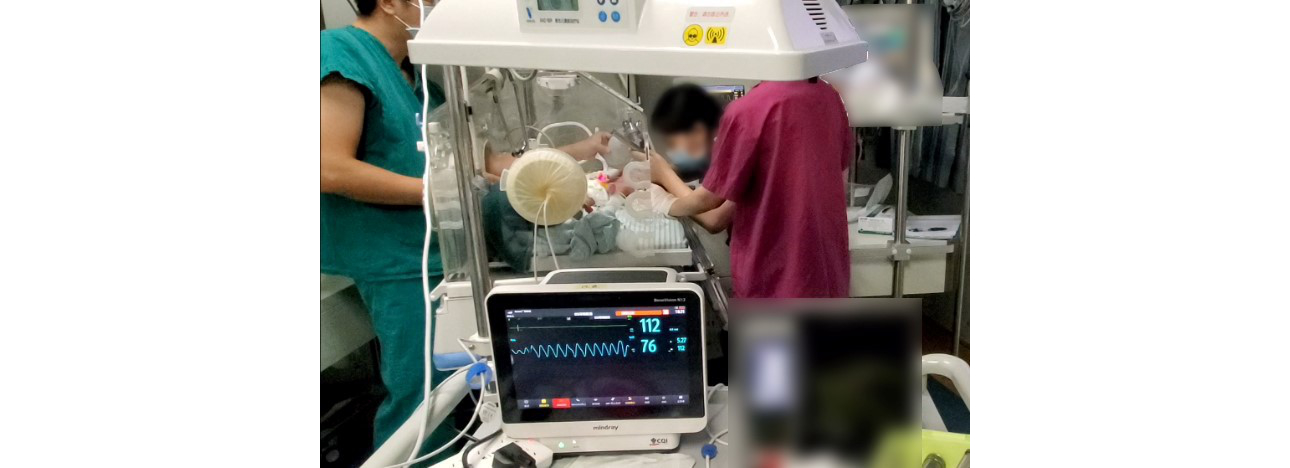
Situations that occurred during the hospital transfer:
The patient was transferred from a lower-level hospital. Due to relatively severe infection, the patient was prone to secrete a large amount of sputum, and the airway was prone to be blocked. During the transfer, the patient required sputum suction every half an hour. The patient had relatively poor oxygenation, and oxygen supply must be depending on mechanical ventilation. Her oxygen saturation could be maintained at about 80 – 85% until she was transferred to a higher-level hospital for further treatment.
After being transferred to a higher-level hospital:
Continuous anti-infective therapy, fluid supportive therapy and mechanical ventilation were given in IMV mode, after trying to increase FiO2 to 60%, the SpO2 of the patient could be maintained at 90%.
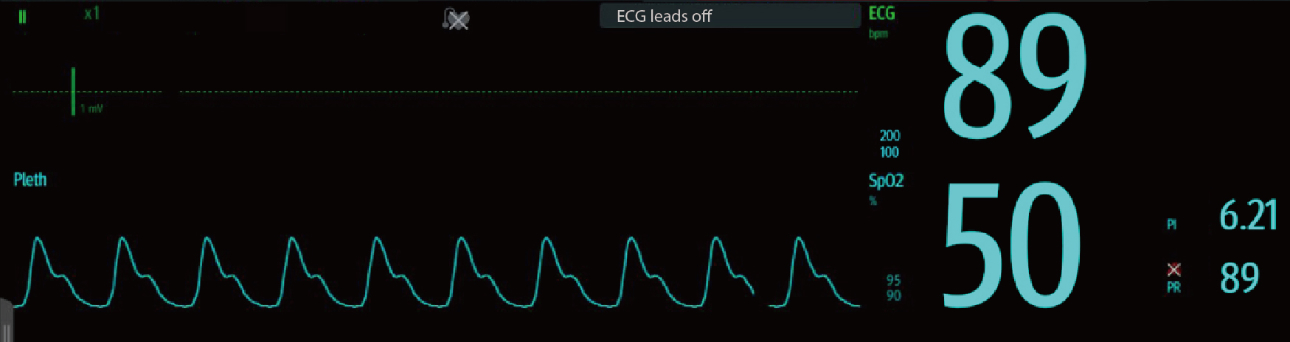
06:03 p.m.
The SpO2 of the patient suddenly decreased to below 80%. The doctor immediately checked the airway through laryngoscopy and found that the patient’s airway and intubation tube were completely blocked due to continuous excessive sputum secretion, leading to asphyxia, and the patient was immediately subjected to endotracheal tube replacement and airway clearance therapy. (As shown in Figure 1)
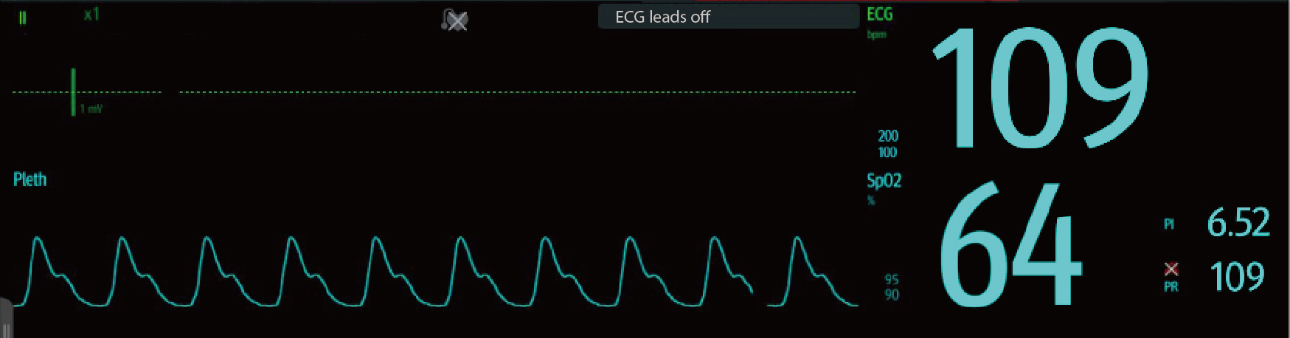
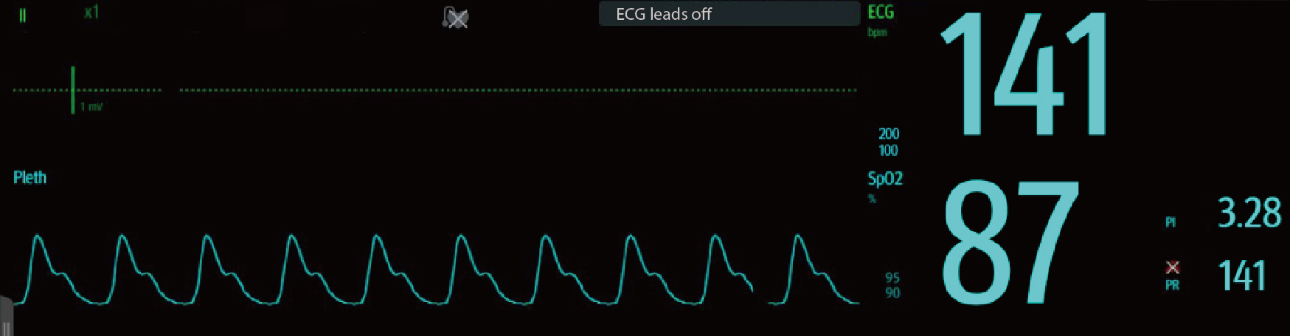
06:05 p.m.
When the obstructed airway catheter is pulled out and replaced with the manual bag valve mask for temporary ventilation, the asphyxia was not relieved, and the SpO2 and heart rate continued to decline. When the SpO2 dropped to about 60%, the doctor decided to complete the tracheal intubation first, and then clear the sputum around the airway as soon as possible after ensuring the normal ventilation status of the patient. (As shown in Figure 2)
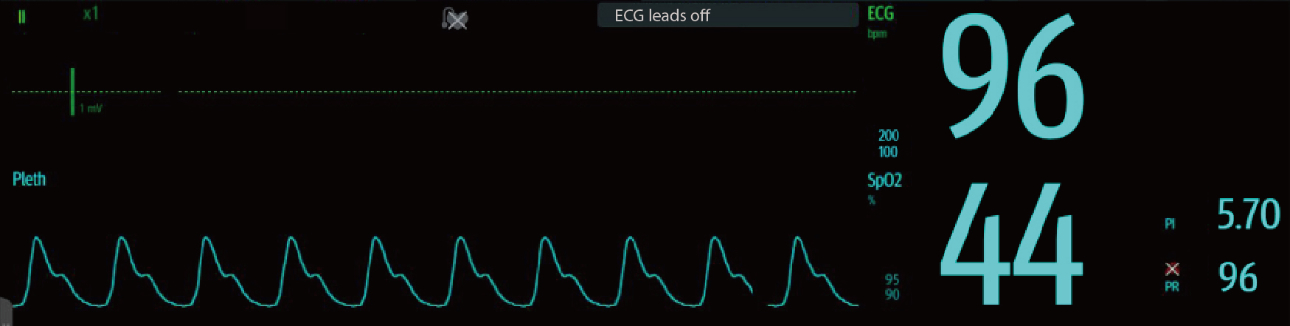
06:07 p.m.
During laryngoscopy-assisted tracheal intubation, the heart rate dropped to below 100 bpm, and the SpO2 dropped to 44%. The patient was in a critical status. (As shown in Figure 3)
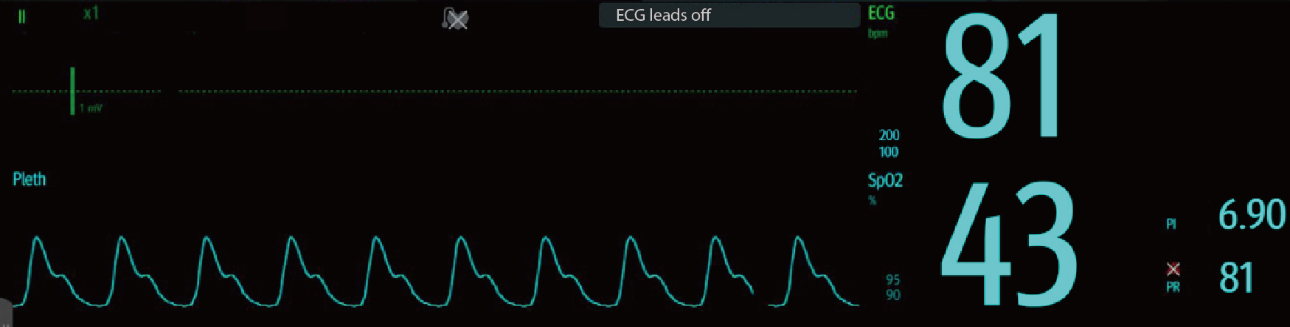
06:08 p.m.
The endotracheal intubation was rapidly completed, but the patient’s heart rate and SpO2 were extremely low, and her condition was very critical. The SpO2 parameter on the monitor is consistent with the patient's status. (As shown in Figure 4)
06:09 p.m.
The doctor immediately started to perform cardiopulmonary resuscitation for rescue, in conjunction with manual bag valve mask for rapid ventilation. After 1 minute of cardiopulmonary resuscitation, the patient's heart began to show an upward trend. The effectiveness of the cardiopulmonary resuscitation was measured by the continuously increasing blood oxygen value on the monitor. (As shown in Figure 5)
06:10 p.m.
The patient’s heart rate returned to 138 bpm and SpO2 returned to 80%, so this rescue was considered as successful.
After the patient’s heart rate and SpO2 steadily rose to the normal range, the airway was cleared after repeated sputum suction for 2 times, so that the patient’s airway was kept patent and mechanical ventilation support was continued to be provided, and her SpO2 could eventually stabilize at more than 90%. (As shown in Figure 6)
Mindray’s Neonatal Patient Monitor ensures stable and continuous output of SpO2 performance in monitoring neonates, which provides an important reference for clinical medical care and treatment, and protects every precious and weak life.
Extended Reading:
In terms of monitor, Mindray has 30 years of experience in the research of parameter SpO2, covering neonates, infants and adults, and its accuracy is widely trusted. In 2017, Mindray initiated the clinical validation of blood oxygen monitoring for critically ill newborns, which has been successively carried out in 15 hospitals (80% A-level hospitals), and a total of 446 cases of critically ill newborns were finally included in the study. The distribution of the cases is as follows (the red bar graph – the distribution of critically ill neonatal patients):
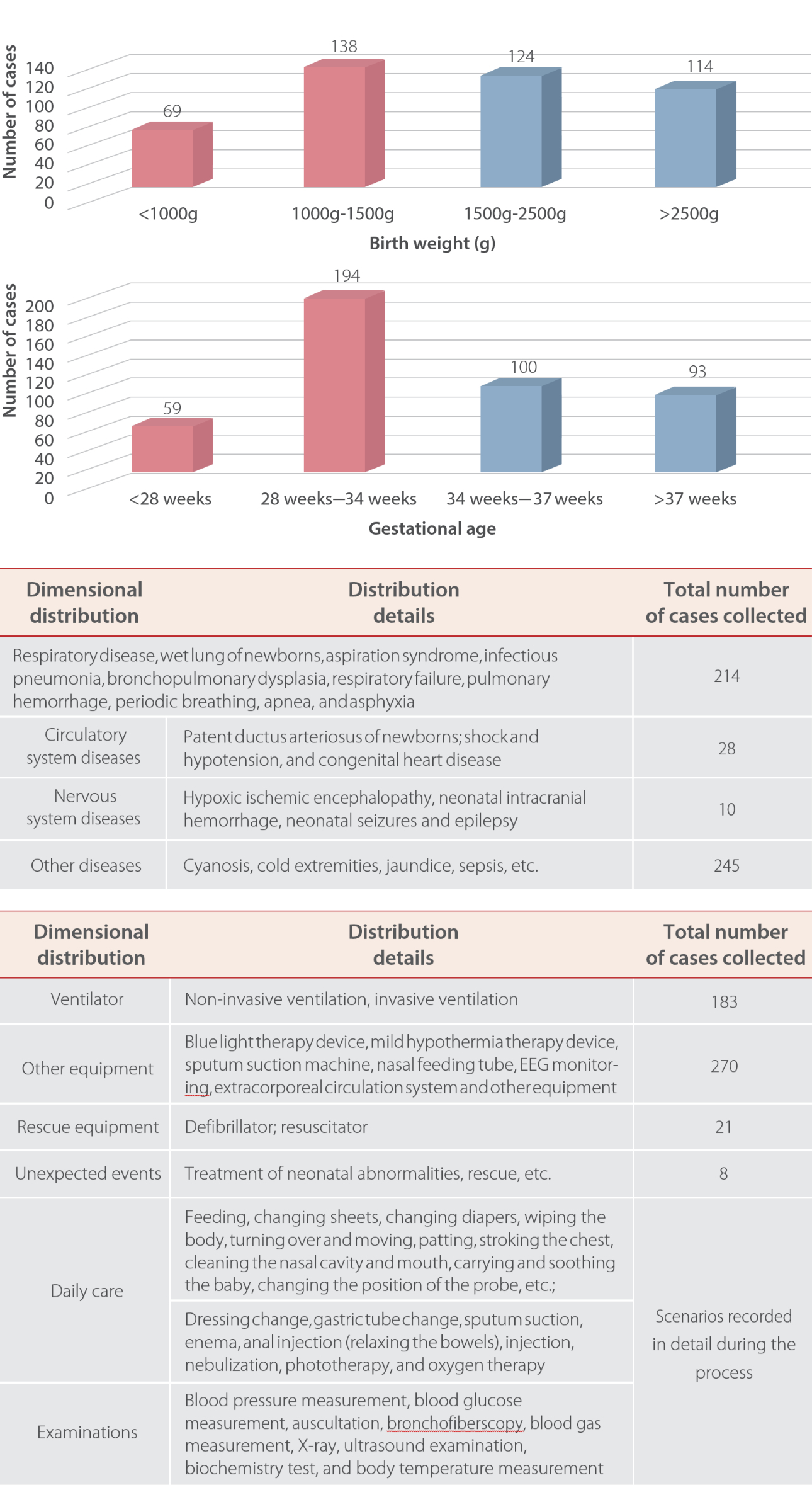
Mindray’s neonatal blood oxygen parameter monitoring can meet complex clinical scenarios and strict requirements under the conditions of low gestational age, very low birth weight, different diseases, and simultaneous use of multiple treatment equipment and medical procedures, and continuously maintain accurate and stable output values to protect every beat of life together with doctors and nurses.




