In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Case Introduction
A 70-year-old female patient was admitted to the hospital for “dyspnea for 3 days with aggravation for 3 hours”.
Three days ago, the patient developed dyspnea without obvious predisposing factors during her afternoon nap, and dyspnea was aggravated three hours ago.
Outpatient ECG: Sinus rhythm, second-degree type I AVB, deeper Q wave with ST elevation (I, aVL, V5, V6), and acute lateral wall myocardial infarction was not ruled out.
Biochemistry test related to heart failure and myocardial infarction: NT-proBNP 13,348 pg/ml, cTnI 11.27 ng/ml; CK-MB 38.34 ng/ml; Myo 56.49 ng/ml; normal D-Dimer.
Immediate emergency angiography + PCI: Well-balanced myocardial perfusion; normal LM, 40% stenosis at the proximal end of LAD; occlusion at the middle segment of LCX; RCA narrowing, with no significant stenosis observed. A 2.75*18 mm drug stent was placed into the LCX. The patient was admitted to the ward due to “acute myocardial infarction”.
Past Medical History
- Diabetes, medication as “acarbose 50 mg tid and repaglinide 1 mg tid”.
- Hypertension for several years, with a systolic pressure up to 160 mmHg, and drugs were not regularly administered.
First Physical Examination at Admission
Body Temperature: 36.5°C
Pulse Rate: 97 beats/minute
Respiratory Rate: 18 breaths/minute
Blood Pressure: 112/72 mmHg
The patient was conscious, with coarse breath sounds in both lungs and a small number of moist rales could be heard in both lower lungs. Her heart rhythm was regular, and no pathological murmur was heard in the auscultation area of each valve. Mild edema in both lower limbs.
Preliminary Diagnosis
- Acute myocardial infarction & KILLIP class III
- Grade 2 hypertension
- Diabetes mellitus type 2
Conditions After Admission Are As Follows
After admission, the patient was given 5-lead ECG monitoring, SpO2 and NIBP monitoring, and oxygen inhalation. The patient did not state any discomfort. Re-examination of biochemical indicators related to heart failure and myocardial infarction showed significantly improved results, indicating that the stent treatment was effective, no accompanying symptoms such as postoperative stent re-clogging occurred, and the condition of heart failure was in remission.
On Day 5 after admission, at 8: 25 a.m.
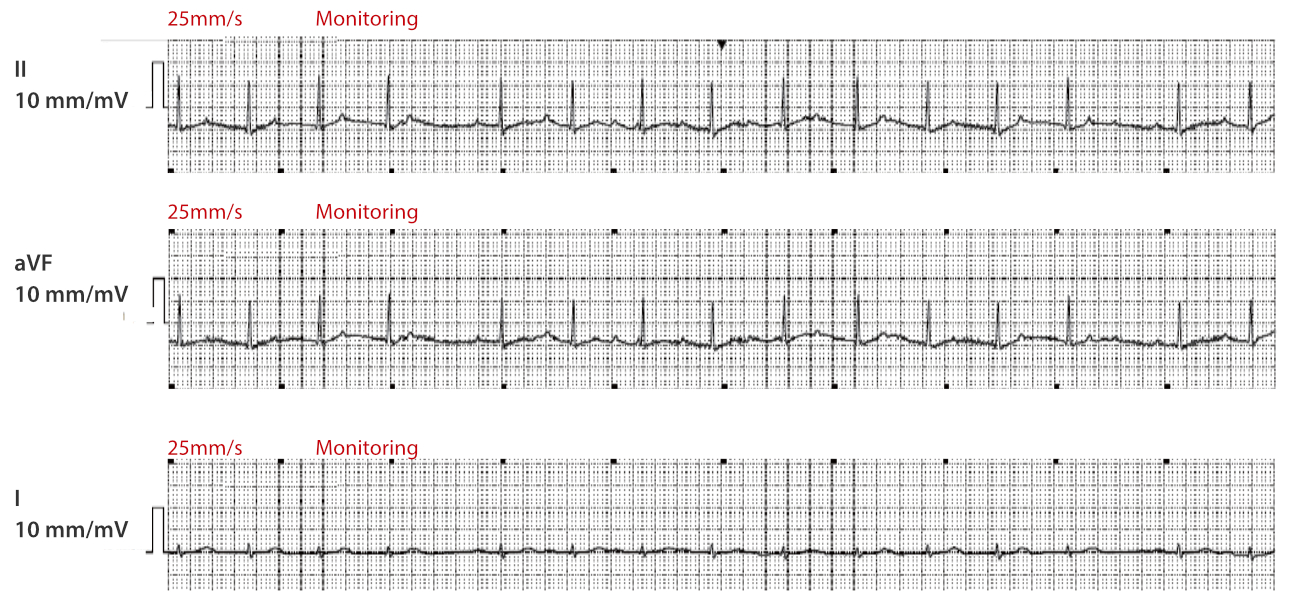
The patient had sudden atrial fibrillation.
At 8: 40 a.m.
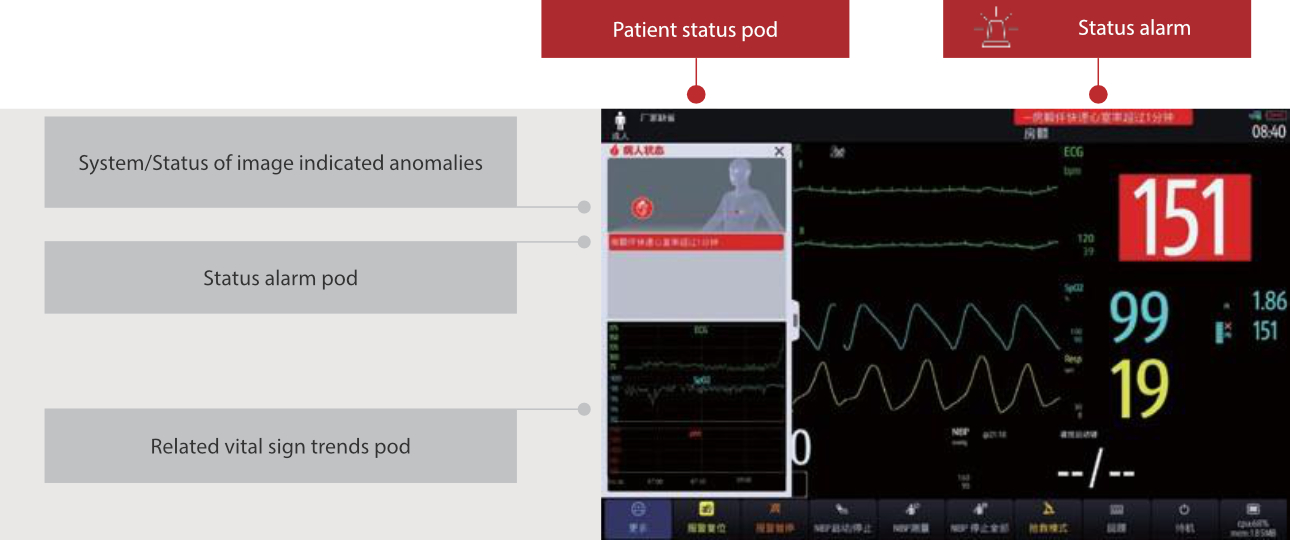
The heart rate rose to 151 beats/min, triggering the “Atrial Fibrillation with High Ventricular Rate” high-level alarm.

After the nurse discovered the alarm above, the doctor was informed immediately. The results of a re-examination of the bedside ECG clearly showed: Atrial Fibrillation. The monitoring data was reviewed, and it was the patient’s first episode of atrial fibrillation after surgery. Because atrial fibrillation usually causes hemodynamic instability, it is manifested by an unstable heart rate.
Considering that the persistently high heart rate may induce the risk of aggravation of heart failure and other risks, and it was a high-risk atrial fibrillation, so amiodarone was used for cardioversion treatment.
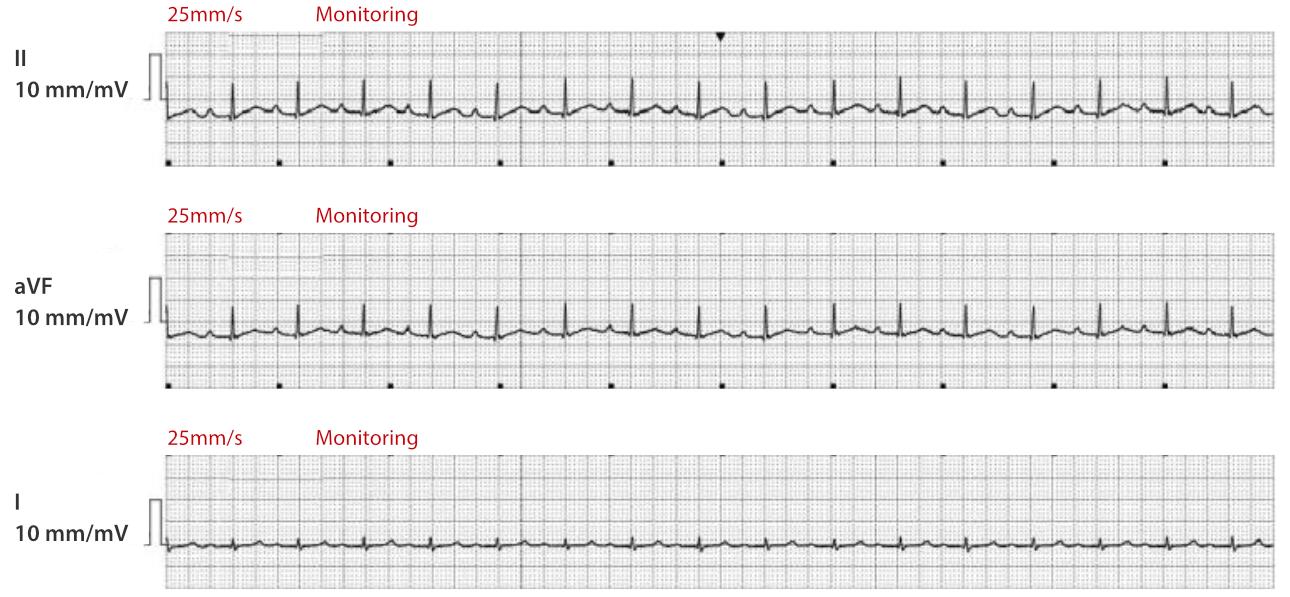
At 09:37 p.m.
After 13 hours of continuous amiodarone pumping and cardioversion treatment, the patient was converted to sinus rhythm and amiodarone was discontinued. The ECGs are as follows:
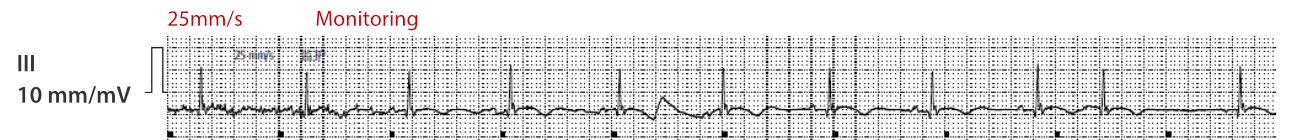
On Day 6 after admission, at 9:53 a.m.
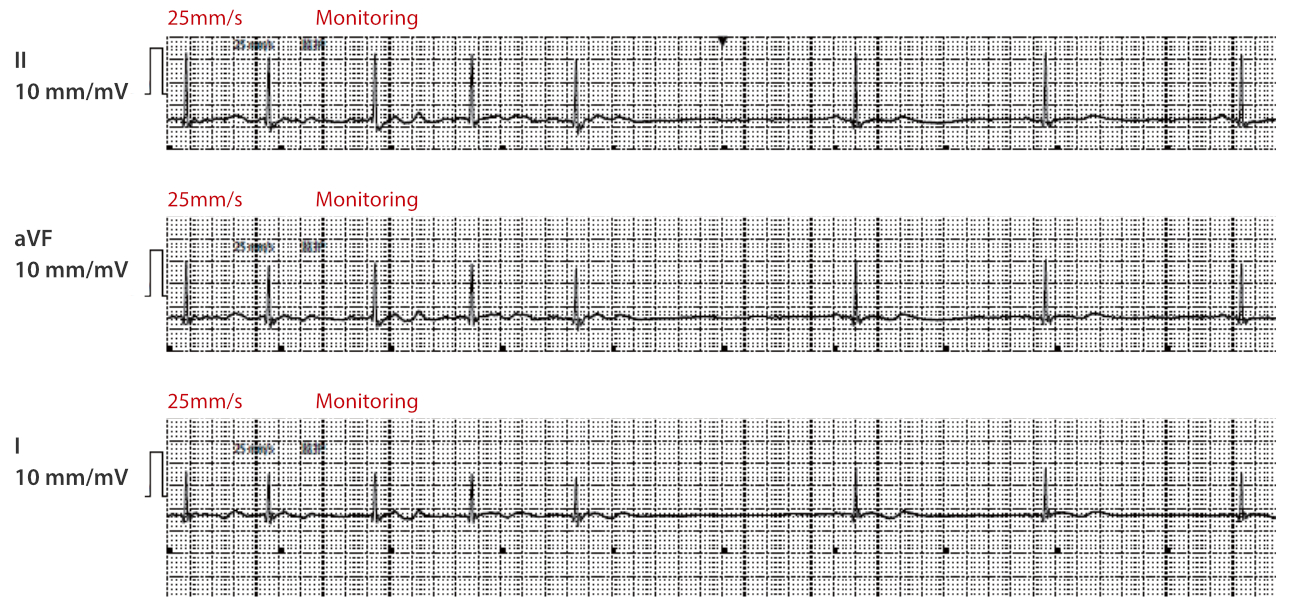
The patient developed atrial fibrillation again.
A few minutes later, the heart rate rose to 153 bpm, triggering atrial fibrillation with high ventricular rate alarm, and the doctor continued amiodarone for cardioversion retreatment.

As the patient had recurrent paroxysmal atrial fibrillation and the duration of atrial fibrillation had exceeded 24 hours, according to the 2020ESC/EACTS Guidelines for the Diagnosis and Management of Atrial Fibrillation, the doctor added anticoagulation on the basis of the original dual antiplatelet therapy and switched to a triple antithrombotic treatment regimen.
Ten hours after drug administration, the patient was converted to sinus rhythm again.
In the subsequent treatment, the patient continued to have sinus rhythm and atrial fibrillation did not recur.
On Day 9 after admission
The superior professor went the rounds of the wards, and analyzed the symptomatic treatments such as antiplatelet therapy, ventricular remodeling improvement, diuresis, amiodarone for cardioversion that had been given to the patient during hospitalization and found that the patient recovered well for that time. The patient was discharged from the hospital with medication and instructed to undergo regular re-examination. She must return for follow-up for any discomfort.
Analysis
In this case, the patient’s surgery went well, the stent placement was effective, the symptoms of heart failure were improved, and the patient’s condition was stable. Low-frequency ECGs are difficult to detect new onset of atrial fibrillation in patient in a timely manner, which may lead to delayed atrial fibrillation treatment. What are the reasons?
Clinically, atrial fibrillation is divided into first diagnosed atrial fibrillation, paroxysmal atrial fibrillation, persistent atrial fibrillation, long-standing persistent atrial fibrillation, and permanent atrial fibrillation. If atrial fibrillation occurs in the form of an alarm, the monitor may face persistent or high-frequency triggering of atrial fibrillation alarms, resulting in severe alarm fatigue in clinical practice. Therefore, the monitor manufacturer sets atrial fibrillation alarm as a non-audible alert message by default. For busy medical staff, atrial fibrillation is easily overlooked.
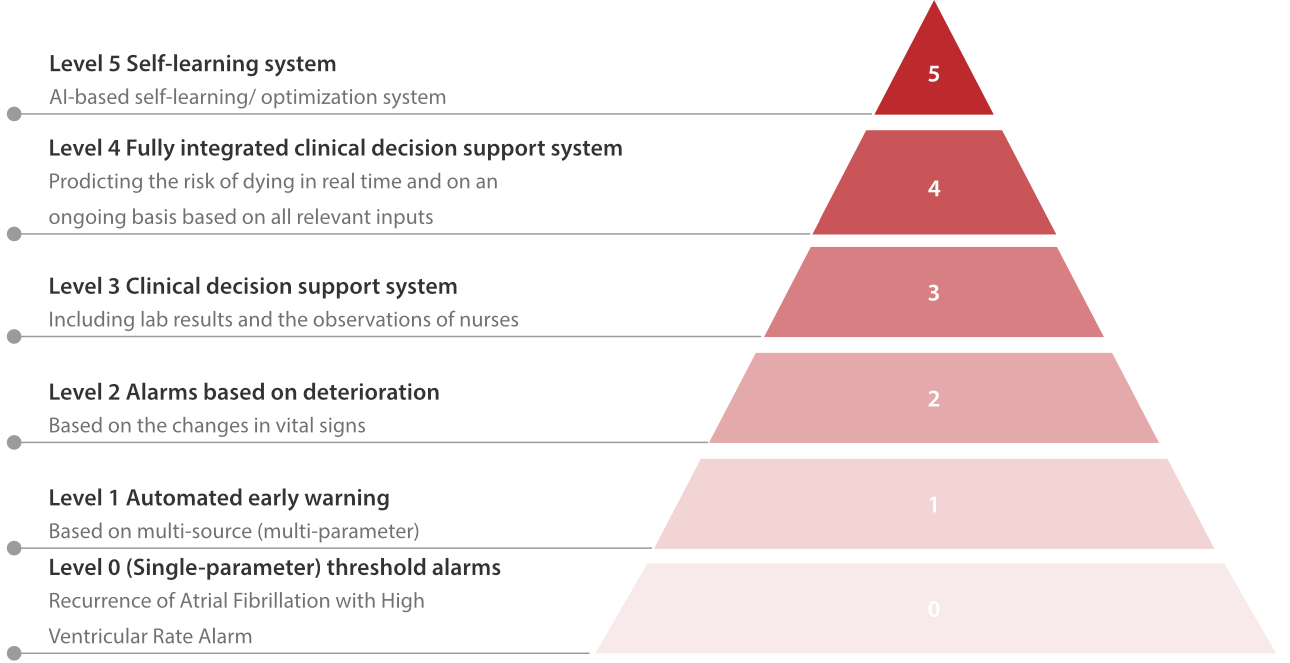
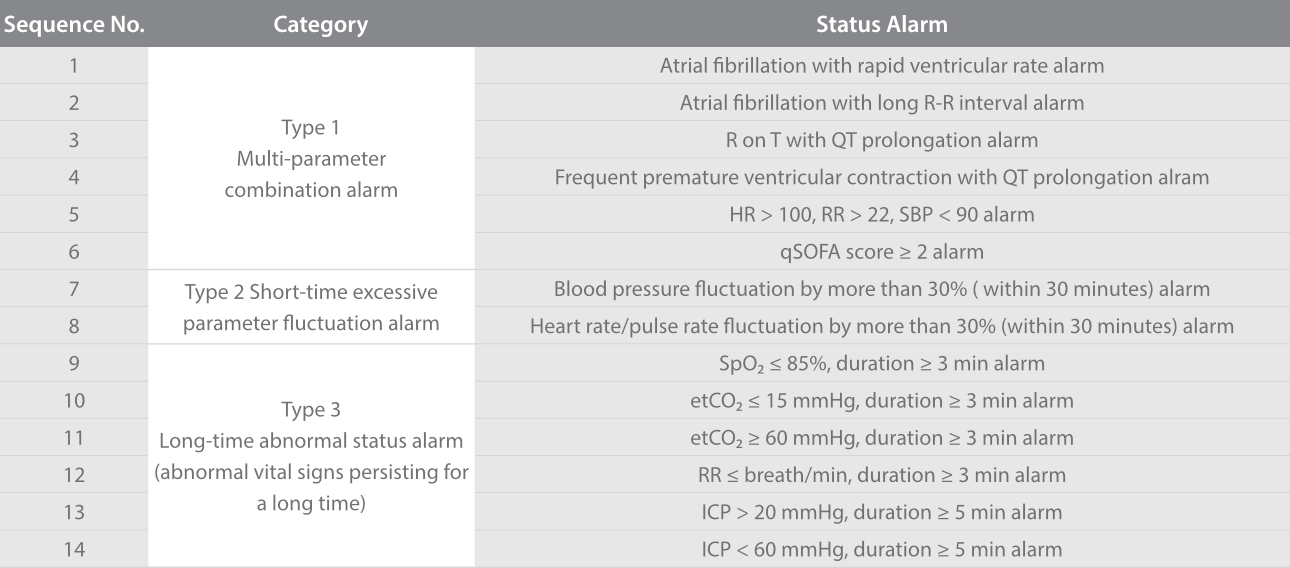
Therefore, Mindray monitoring, in reference to domestic and foreign guidelines and consensus, and based on the level 1 and level 2 alarm levels classified by the five leading academic hospitals in the European Union, has innovatively developed a combined alarm system to create 3 types of 14 status alarms, assisting in effectively reducing the alarm frequency in clinical practice and reducing the alarm load for medical staff.
As shown in the figure below, the monitoring interface will clearly and prominently present the status display area and status alarm pod, increasing the attention of medical staff to important alarms, so that they can immediately discover the changes in the patient’s condition and abnormal status, leading to more timely and accurate formulation of treatment regimens for patients to achieve better prognosis.
References
1. Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest 1990;98:1388–92.
2. Bedell SE, Deitz DC, Leeman D, Delbanco TL. Incidence and characteristics of preventable iatrogenic cardiac arrests. JAMA 1991;265:2815–20.
3. Franklin C, Mathew J. Developing strategies to prevent in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med 1994;22:244–7.
4. Rich K. In-hospital cardiac arrest: pre-event variables and nursing response. Clinical Nurse Specialist 1999;13:147–53.
5. Buist M, Bernard S, Nguyen TV, Moore G, Anderson J. Association between clinically abnormal observa- tions and subsequent in-hospital mortality: a prospective study. Resuscitation 2004;62:137–41.
6. McQuillan P, Pilkington S, Allan A, et al. Confidential inquiry into quality of care before admission to intensive care. BMJ 1998;316 (1853–8.4).
7. Sax FL, Charlson ME. Medical patients at high risk for catastrophic deterioration. Crit Care Med 1987;15:510–5.
8. Daffurn K, Lee A, Hillman KM, Bishop GF, Bauman A. Do nurses know when to summon emergency assistance? Intensive Crit Care Nurse 1994;10:115–20.
9. Buist MD, Jarmolowski E, Burton PR, Bernard SA, Waxman BP, Anderson J. Recognizing clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. A pilot study in a
tertiary-care hospital. Med J Aust 1999;171:22–5.
10. Hillman KM, Bristow PJ, Chey T, Daffurn K, et al. Antecedents to hospital deaths. Intern Med J 2001;31:343–8.
11. Kause J, Smith G, Prytherch D, et al. A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia, New Zealand, and the United Kingdom—the ACADEMIA study. Resuscitation 2004;62:275–82.
12. Hillman K, Bristow PJ, Chey T, et al. Duration of life-threatening antecedents prior to intensive care admission. Intensive Care Med 2002;28:1629–34.
13. Goldhill DR, White SA, Sumner A. Physiological values and procedures in the 24 h before ICU admissions from the ward. Anaesthesia 1999;54:529–34.
14. Morgan RJM, Williams F, Wright MM. An early warning scoring system for detecting developing critical illness. Clin Intensive Care 1997;8:100.
15. Stenhouse C, Coates S, Tivey M, Allsop P, Parker T. Prospective evaluation of a modified early warning score to aid earlier detection of patients developing critical illness on a general surgical ward. Br J Anaesth 2000;84:663P.
16. Subbe CP, Davies RG,Williams E, Rutherford P, Gemmell L. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilization in acute medical admissions. Anaesthesia 2003;58: 797–802.
17. Hodgetts TJ, Kenward G, Vlachonikolis IG, Payne S, Castle N. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation 2002;54:125–31.
18. McGloin H, Adam S, SingerM. Unexpected deaths and referrals to intensive care of patients on general wards. Are some cases potentially avoidable? J R Coll Physicians Lond 1999;33:253–9.
19. McQuillan P, Pilkington S, Allan A, Taylor B, Short A, Morgan G, et al. Confidential inquiry into quality of care before admission to intensive care. Br Med J 1998; 316(7148):1853–8.
20. Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? Resuscitation 1998;37:133–7.
21. www.nightingale-h2020.eu



