Dr. PM Venkata Sai
Professor and Head Of Clinical Services (HOCS) & Senior Consultant at Sri Ramachandra Institute of Higher Education and Reasearch (SRIHER ) Sri Ramachandra University, Porur, Chennai.
An Approach To Emergency Bedside Lung Ultrasound
The utility of computed tomographic imaging in lung pathologies is undisputed. However, lung ultrasound (LUS) is very useful in emergency situations, where time is of the essence. Thorax and lung ultrasound has gained importance in daily routine which is especially true in the setting of Point of Care UltraSound examination (POCUS)1 . Furthermore, the portability of the equipment, which allows for even bedside examination, the comfort of the patient, repeatability, and reduced cost are the true strength of this imaging technique. It is done bedside immediately after a physical examination and before echocardiography in critical care.
Lung ultrasound is often decribed as interpretation of artefacts and can be performed rapidly in critically ill patients.The purpose of lung ultrasound to look for lung sliding, anterior lung rockets, posterior and/or lateral alveolar and/or pleural syndrome (PLAPS).
The preset requirement for doing lung ultrasound are to use 5 MHz convex probe, single focal point kept on a pleural line, highest frame rate, reduced dynamic range, off the compound and harmonic imaging. Low mechanical index store freeze images and video clips in DICOM format.
Lung examination - Patient supine, transducer placed in sagittal, coronal and M mode for lung sliding or PLAPS point for pleural effusion.
FINDINGS
A-lines - Classic reverberation artefact, horizontal hyperechoic lines deep to the pleural line. These waves are reflected strongly by tissue/air interface and reverberate or bounce back and forth between the transducer and lung surface – bat sign. The bat sign – posterior acoustic shadowing of the ribs are the wings of bat and hyperechoic belly – pleural line represents the bat.
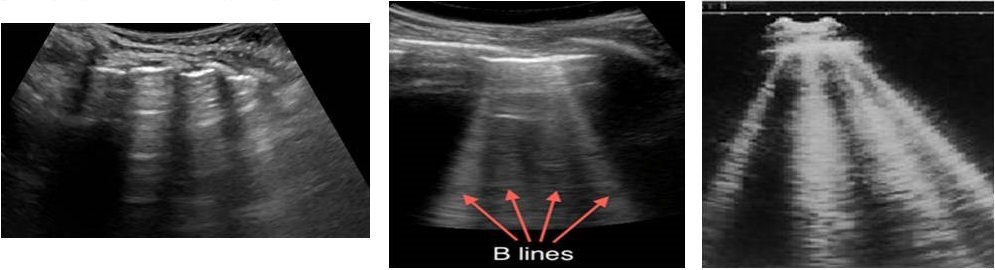
B-lines - correlates with interstitial oedema. They are comet tail artefacts, arising from pleural line, hyperechoic, laser beam like an artefact, long, without fading, erasing A-lines moving with lung sliding.
B lines present in any disease affecting the interstitium, interlobular septa surrounded by alveolar air. B lines are likely to represent fluid or fibrosis. Air in alveoli and water in the interlobular septa causes the sound to reverberate to and fro between the septa creating the line for each reverberation which combine to form B lines.
Two B lines – comet-tail artefact. Two or three B lines – lung rockets in interstitial syndrome. Three or four B lines indicate septal rockets due to edematous subpleural interlobular septa. B lines correlate with kerley B lines on chest Xray. Diffuse B line pattern represent cardiogenic or noncardiogenic pulmonary oedema or pneumonitis. Focal multiple B lines present posterolaterally in a normal lung seen in pneumonia, atelectasis, lung contusion and pulmonary infarcts. At least seven B lines are called ground glass rockets.
C-lines - concave or curvilinear in shape, centimetres in size, represents alveolar consolidation. Lung sliding – During normal respiration or mechanical ventilation, the visceral pleural moves against the parietal pleura. A subtle sparkling to and fro movement artefact called lung sliding.
Lung sliding can be confirmed using M-mode. In the presence of lung sliding, the seashore phenomenon occurs. Subcutaneous tissue above the pleural line generates the horizontal straight line, there will be a sandy appearance below the pleural line created by the movement of the lung sliding.
INDICATIONS
Evaluate the critically ill patients who are experiencing severe shortness of breath, different pathologies have a distinct sonographic appearance. Severe shortness of breath – Causes – pneumothorax, alveolar interstitial oedema, pneumonia, pleural effusion and acute respiratory failure have a distinct sonographic appearance.
1. Pneumothorax - presence of A-line, no B lines, absent lung sliding, lung point may be identified. Air – being non-dependent will collect anteriorly in a supine patient.
M mode – lung point sign appears at the precise line where the seashore sign shifts to stratosphere/barcode sign – very specific sign of pneumothorax.
2. Alveolar interstitial syndrome2
B lines 7mm apart indicate thickened interlobular septa and ultrasound equivalent to Kerly B lines.
B lines 3mm apart correlate with ground glass opacities.
Better appreciated in the mid axillary anterolateral intercostal scans.
3. Pneumonic consolidation
Early pneumonia - B lines are tiny areas of subpleural consolidation.
Tissue like sign - shred sign - alveolar consolidation.
4. Lung sonography in acute respiratory failure
A-lines transformed into B lines at a pulmonary artery occlusion pressure threshold of 18mmHg at the anterior chest wall in a critically ill patient. B lines appear with interstitial oedema.
The bedside lung ultrasound in emergency (BLUE) protocol for immediate diagnosis of acute respiratory failure and fluid administration limited by lung sonography (FALLS).
Protocol of management of acute respiratory failure - BLUE protocol was designed to assess the acute respiratory failure in spontaneously breathing patient.
Lung ultrasound is a visual stethoscope and limits one-third of urgent bedside radiograph and two-thirds of urgent CT scan.
The characteristic findings of Lung ultrasound in COVID pneumonia -
A. Thickening of the pleural line with irregularity.
B. B lines in a variety of patterns including focal, multifocal and confluent.
C. Consolidation in a variety of patterns including multifocal, small, non-translobal and translobar with occasional mobile air bronchograms.
D. Appearance of A-line during the recovery phase.
Lung USG in COVID 19 patients for rapid assessment of severity, to track the evolution of the disease, to assess the varying degree of interstitial syndromes and alveolar consolidation and for making a decision to weaning the patient from ventilatory support.
LIMITATION
Lung ultrasound cannot detect the lesion that is situated deep within the lung.
CONCLUSION
Promising bedside diagnostic technique. Used to follow up on disease progression and therapy.

