Point of care ultrasound (POCUS) has increasingly become more common in expediting patient assessment and diagnosis in emergency settings. As ultrasound continues to become the imaging modality of choice for helping to assess patients, comprehensive education around POCUS imaging has become a necessity for clinicians. Unfortunately, ultrasound training can be challenging due to a shortage of experienced teachers and budget constraints.
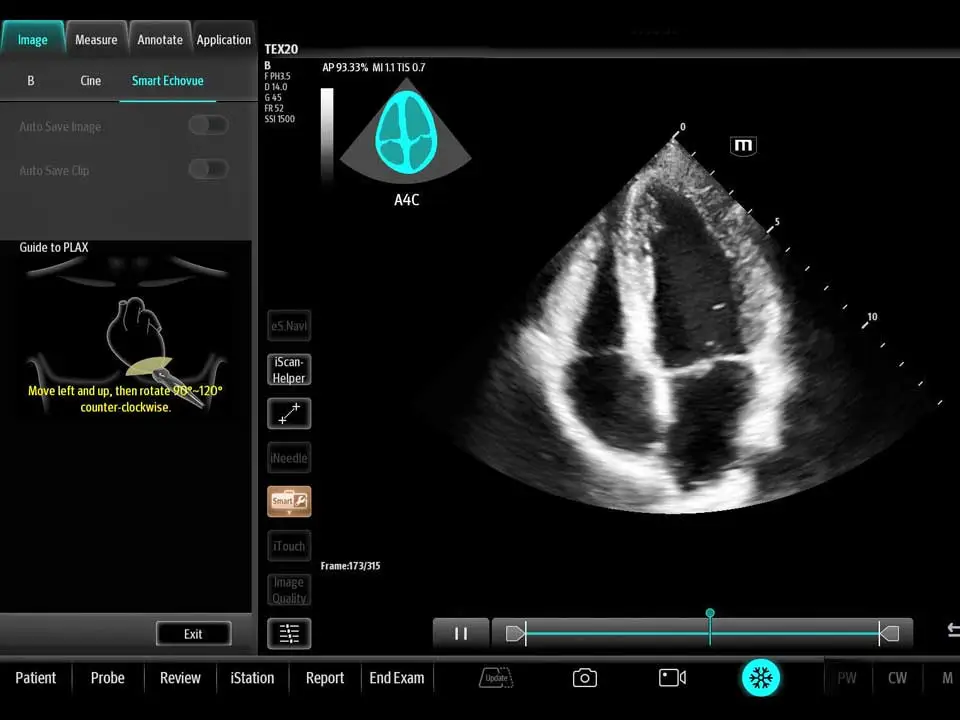
However, advanced ultrasound technology, including artificial intelligence (AI)-assisted scanning, on-system tutorials, guided protocols, and self-testing features, is revolutionizing POCUS education and helping novice users quickly become accustomed to the POCUS environment.
The Role of Technology in Modern POCUS Education
Continuous learning is a necessity in the emergency medicine field, where new techniques and advancements emerge frequently. Staying updated with the latest technology in POCUS not only enhances diagnostic accuracy but also can improve patient outcomes. Integrating advanced technology into POCUS education helps to reduce the learning curve for new clinicians entering the field, as well as clinicians who are adopting the new technology, and enables experienced users to get accustomed to advanced diagnostic tools more quickly.
AI-Assisted Ultrasound Scanning
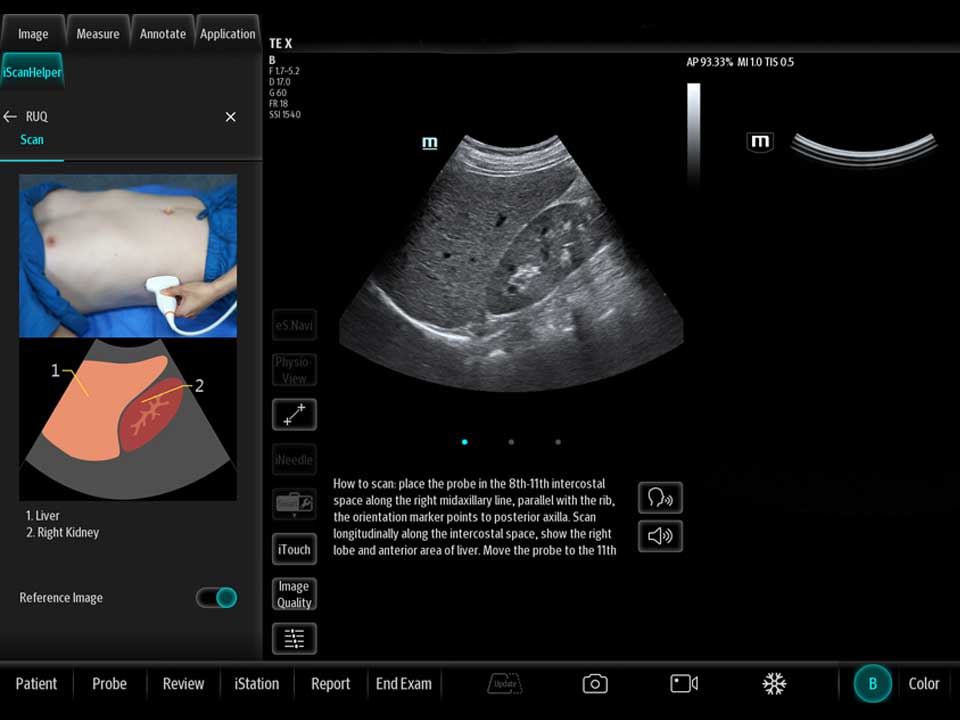
Guided Ultrasound Protocols
Guided ultrasound protocols provide a structured approach to scanning and help mitigate inconsistencies by offering clear instructions for common procedures. An ultrasound machine with a guided workflow can enable clinicians to recognize abnormalities simply, swiftly, and accurately – for example, features that automate exam steps based on user-defined protocols. From automatic image annotations to activating modes and measurement packages, ultrasound systems with guided protocol technology can reduce the chance of incomplete exams, allowing for more efficient quality assurance reviews. Guided protocols can help provide detailed instructions for the following exams:
· RUSH exam – The RUSH exam stands for Rapid Ultrasound for Shock and Hypotension. POCUS can help to identify shock in patients in the emergency department, enabling clinicians to take the appropriate life-saving measures. The initial RUSH protocol, now often remembered by the pneumonic HI-MAP, evaluates five major areas: Heart, IVC, Morrison’s pouch, Aorta, Pneumothorax. This has since been expanded to a broader view, or the “pump, tank, pipes” protocol. This refers to evaluating several organ systems and adds views to evaluate for pulmonary effusion and interstitial edema, as well as for DVT in the lower extremities.2
· eFAST exam – The eFAST exam, or Extended Focused Assessment with Sonography in Trauma, uses ultrasound imaging to examine a patient’s heart, lungs, and abdomen to detect peritoneal fluid, pericardial fluid, pneumothorax (otherwise known as a collapsed lung), and hemothorax (blood collection in the hollow space between the lungs and chest) in a trauma patient.3
· BLUE protocol – In POCUS, the BLUE protocol is known as the Bedside Lung Ultrasound in Emergency. This exam is performed to detect respiratory failure at the bedside immediately after the physical examination, and before echocardiography.4
Using guided protocols provides educational value by helping clinicians learn the rationale behind each step, improving their understanding of the procedure. This deeper knowledge translates into better diagnostic accuracy and patient care.
On-System Ultrasound Tutorials
On-Board Ultrasound Self-Testing Features
Ultrasound systems with self-assessment tools allow clinicians to evaluate their skills and identify areas for improvement. Self-testing provides immediate feedback, enabling clinicians to adjust their techniques in real-time. This iterative learning process helps clinicians build competence. Over time, they can track their progress and see tangible improvements in their POCUS skills.
By incorporating self-testing into their routine, clinicians can maintain high standards of practice. Regular assessment helps reinforce learning and keeps skills sharp, ultimately benefiting patient care.
Benefits of Integrating Educational POCUS Technologies
The integration of AI-assisted scanning, on-system tutorials, guided protocols, and self-testing features in an ultrasound system creates a comprehensive toolset for POCUS clinicians. This integrated approach accelerates the learning curve for POCUS users. Clinicians can quickly acquire the necessary skills and knowledge, reducing the time required to become proficient in POCUS. This efficiency is crucial in a healthcare environment where time and ultrasound training are often limited.
Better-trained practitioners lead to improved patient outcomes. When clinicians are confident in their POCUS abilities, they can make faster and more accurate diagnoses. This leads to timely interventions and better overall patient care.
The Mindray Difference in Ultrasound Training
Mindray’s Point of Care Ultrasound Machines provide leading-edge technology and everyday applications that meet the diverse demands of your departments and the evolving needs of your patient population. At Mindray, we recognize the importance of staying up to date on the latest advancements and best practices in the field. We are dedicated to enhancing POCUS education by sponsoring numerous hands-on workshops throughout the year, offering new and experienced clinicians opportunities to sharpen their skills and get accustomed to advanced ultrasound technology. To keep up with our educational opportunities, please visit our events page for more information.
References:
[1] Baum, Evan, et al. “Acquisition of cardiac point-of-care ultrasound images with Deep Learning.” CHEST Pulmonary, vol. 1, no. 3, Dec. 2023, p. 100023, https://doi.org/10.1016/j.chpulm.2023.100023.
[2] Stolz, Lori A., and Aalap Shah. “Rapid Ultrasound for Shock and Hypotension (Rush).” ACEP , 10 Nov. 2021, www.acep.org/sonoguide/advanced/rush/.
[3] Habrat, Dorothy. “How to Do E-Fast Examination - How to Do e-Fast Examination.” Merck Manual Professional Edition, Merck, Dec. 2023, www.merckmanuals.com/professional/critical-care-medicine/how-to-do-other-emergency-medicine-procedures/how-to-do-e-fast-examination.
[4] Carroll D, Bell D, Kang O, et al. Bedside lung ultrasound in emergency (approach). Reference article, Radiopaedia.org (Accessed on 01 Jul 2024) https://doi.org/10.53347/rID-61395