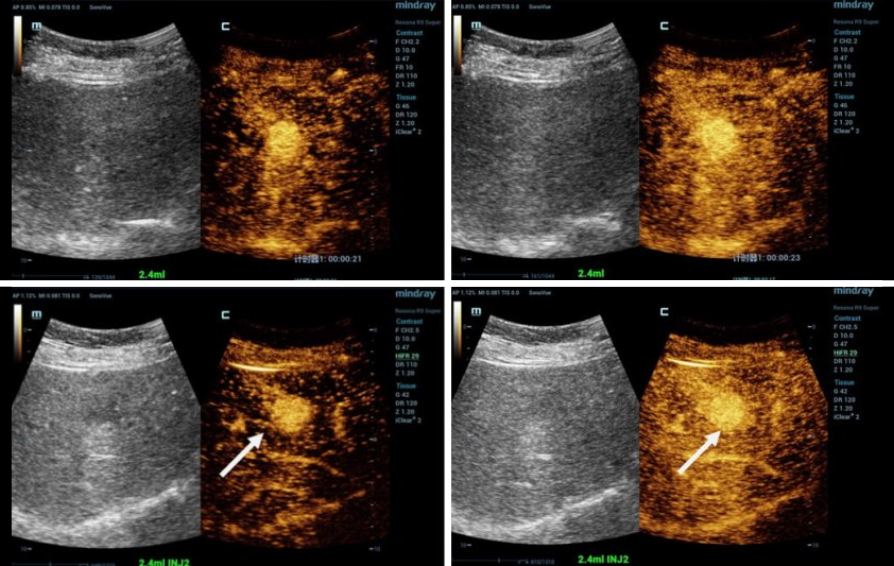
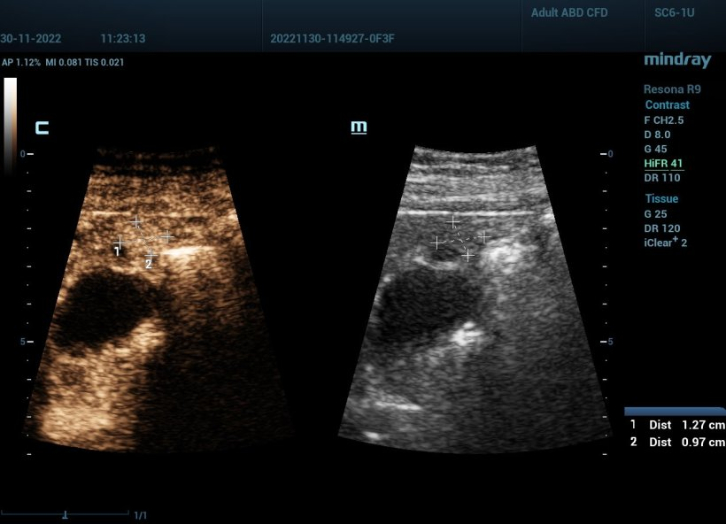
A current multicenter study at six university hospitals evaluates whether high frame-rate contrast-enhanced ultrasound (HiFR CEUS) can more accurately than conventional ultrasound methods distinguish small hepatocellular cancers from other small liver lesions.
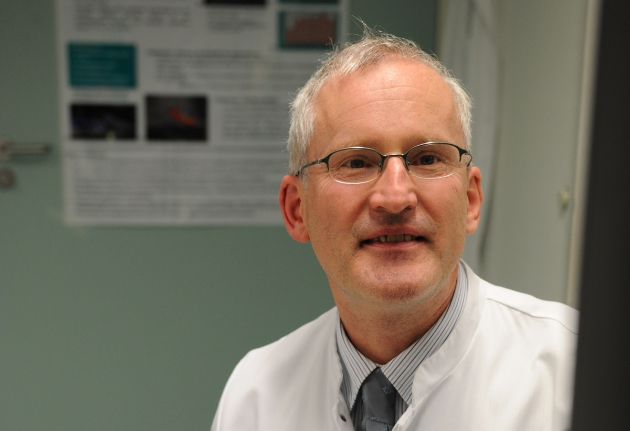
Contrast-enhanced ultrasound (CEUS) is a very dynamic field and in the past few years technological innovations have further increased image quality. One of these innovations is high frame-rate contrast-enhanced ultrasound (HiFR CEUS) which can generate up to ten times more images than conventional ultrasound – in the same time. Researchers in seven centers in Germany, Switzerland and China are evaluating the effectiveness of HiFR CEUS in diagnosing small liver lesions. Professor Dr Yi Dong of the Department of Ultrasound, Xinhua Hospital, Shanghai Jiaotong University School of Medicine, and Professor Dr Christoph F Dietrich, Department of General Internal Medicine, Hirslanden Bern, Switzerland, explain the background and the objectives of the study.
What exactly is being investigated in this study?
Yi Dong: 'The main aim is the more precise diagnosis of focal liver lesions with a diameter of less than 3 cm in patients with and without liver cirrhosis. Previous studies have shown that HiFR CEUS visualizes patterns and vessel morphology in such lesions very well. We expect HiFR CEUS to offer improved temporal and spatial resolution, in other words higher quality images of very small liver lesions. This would increase confidence in the characterization and diagnosis of these lesions. Earlier research on hepatocellular carcinoma (HCC) has found that it makes quite a difference whether the small lesions are located in the cirrhotic or in the healthy liver background.'
Christoph Dietrich: 'Patients with liver cirrhosis have an increased high risk of developing HCC. Tumors larger than 30 mm in patients with liver cirrhosis are most likely HCC. If the lesion diameter is only 12 mm the likelihood of HCC is reduced to fifty-fifty. Consequently, characterization of small tumors is more important than that of larger ones since those are most likely HCC anyway, or other differential diagnoses have yielded unambiguous results. While in most cases HCC can be surgically removed or ablated, surgery is usually not indicated for other liver tumors. Our aim is to make sure no patient with a benign or malignant non-HCC undergoes unnecessary surgery.'
Which method is currently used to characterize the tumors in clinical routine?
Christoph Dietrich: 'In order to determine whether tumor surgery is indicated, a PET-CT scan from neck to pelvis, the so-called staging, is performed. In oncology, ultrasound does not offer the same performance as CT because, among other reasons, it cannot penetrate the lung. CT might be slightly inferior to ultrasound for certain exams of the abdominal organs but it is the evidence-based method of choice and in this context an all-in-one procedure. In our study we use HiFR CEUS on top to see whether such an ultrasound scan yields additional relevant information. If scientific evidence shows that HiFR CEUS can classify small lesions better than the current CT/MRI scan, patient treatment will be improved and superfluous surgery can be avoided.'
Yi Dong: 'We do expect HiFR CEUS to outperform conventional CEUS in the diagnosis of focal liver lesions with regard to diagnostic accuracy, sensitivity and specificity. In the study we directly compare the two imaging methods. However, we not only aim to show that HiFR CEUS is superior to conventional CEUS; we also want to identify the strengths of each of these two methods.'
Christoph Dietrich: 'No matter whether high or low frame-rate, CEUS offers one crucial advantage: it is strictly intravascular. While CT contrast agents are active outside of the blood vessels, ultrasound contrast agents only show the vasculature.'
How does this imaging technology work?
Yi Dong: 'In conventional ultrasound systems the frame-rate in non-cardiac contrast-enhanced imaging is about ten frames per second. The HiFR CEUS system we use, Mindray Resona 9, is much faster: it can generate up to 100 images per second. Such a high frame-rate offers better visualization of vascular morphology and it shows microvascular perfusion details and better tracking movement. In short: it improves the diagnostic efficiency of CEUS. In our study we will focus on the vascular architecture during the arterial CEUS phase, the early wash-in phase, contrast-enhancement time, elimination and the relevant patterns.'
Would you mind explaining this in more detail?
Christoph Dietrich: 'Approximately 70% of total liver blood flow is through the portal vein which carries nutrients and metabolic products from the gastrointestinal tract and toxins for detoxification to the liver. The arterial blood also provides 30% of the oxygen. Contrast-enhanced liver ultrasound thus uses the arterial as well as the portal venous phase to generate images. In a cirrhotic liver the portal vein is damaged and the blood can no longer be detoxified. Thus, with regard to imaging, the portal venous phase offers less information. Therefore, our study will focus on the arterial phase. Due to the high frame-rate a high volume of relevant data is acquired despite the fact that the portal venous phase is disregarded. It’s like a fishing net: the more tightly woven the net, the more fish you can catch. With regard to imaging: the higher the line density, the higher the resolution. More tumors are caught and can be dealt with in compliance with current medical guidelines.'
Would you mind explaining this in more detail? Are other innovative technologies used in the study?
Yi Dong: 'We use a particular software package called VueBox to perform a quantitative analysis of the data. This allows us to capture the time intensity curve and to provide quantitative parameters for future diagnostics. We do hope that these quantitative analyses will allow us to detect small lesions earlier.'
Christoph Dietrich: 'Quantifying enhancement kinetics is a promising tool to make imaging more objective. After all, figures provide more information that the mere degrees of brightness that are visible during contrast agent enhancement and wash-out.'
Going forward, could HiFR CEUS be used for other indications?
Yi Dong: 'HiFR CEUS might support the diagnosis of small breast or thyroid lesions and of the microvascular perfusions of the vessels feeding the carotid.'
Christoph Dietrich: 'What we said earlier about the liver also holds true for other organs: the smaller the lesion, the higher the likelihood that it is a benign or a different kind of malignant tumor. Nevertheless the method cannot be transferred 1:1 to other organs. Each organ has its own rules.'
Thank you very much for this interview.
Profiles:
Professor Dong Yi, MD, PhD is Chief of the Ultrasound Department at Xinhua Hospital, Shanghai Jiaotong University School of Medicine. She serves as Vice Chair of the Youth Committee, Chinese Society of Ultrasound in Medicine (CSUM) and Shanghai Society of Ultrasound in Medicine. As a member of the Expert Group of Guidelines and Good Clinical Practice she co-authored recommendations for contrast-enhanced ultrasound (CEUS) in the liver (updated 2020) for WFUMB in cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Dong Yi was a postdoctoral research fellow at the Massachusetts General Hospital, Harvard Medical School, USA, and a research fellow at Pavia University, Italy, and at Caritas Hospital, Bad Mergentheim, Germany.
Professor Dr. med. Christoph Frank Dietrich, MBA, is chief of the Medical Department at Hirslanden Kliniken Beau Site, Salem and Permanence, Switzerland. He is Professor honoris causa at Zhengzhou University, China. He specialized in internal medicine (1997), gastroenterology & hepatology (2000) including the Fellowship in Gastroenterology (EBG), pneumology (2002), hematology and oncology (2008), proctology (2009), palliative care medicine (2009), and geriatric medicine (2009). He served as Honorary Secretary of EFSUMB from 2007 to 2011. He was President of the European Federation of Societies in Ultrasound Medicine and Biology (EFSUMB, 2013-2015) and he was Vice President of the World Federation of Ultrasound in Medicine and Biology (WFUMB) from 2017 to 2019. His academic career is focused on endoscopy and ultrasound. He published more than 1100 scientific papers and book chapters.