Falls are the second leading cause of accidental injuries and deaths worldwide. An estimated 684,000 individuals around the world die from falls each year, and as many as 37.3 million falls per year are severe enough to require medical care. And individuals over 60 years old experience the highest number of falls [1].
Advancing age is a major risk factor for falls. Some clinical reports indicated that, as the vulnerability increases with age, the risk to health also increases when a marked event occurs in the most vulnerable population [2].
It is important to identify falls in a faster and more accurate way, followed by immediate treatment for the improvement of the clinical adverse outcomes in older patients, in case of limited care from caregivers and patient's family, against the unpredictability of falls.

Case 1
Patient's profile
Male, 84-year-old, admitted due to "acute appendicitis with peritoneal abscess and abdominal infection".
Medical history
Parkinson's disease (over 15 years), postural hypotension (over 5 years), hypoadrenocorticism (over 3 years), mixed dementia (over 2 years), and lacunar infarction (3 months).
Post-hospitalization
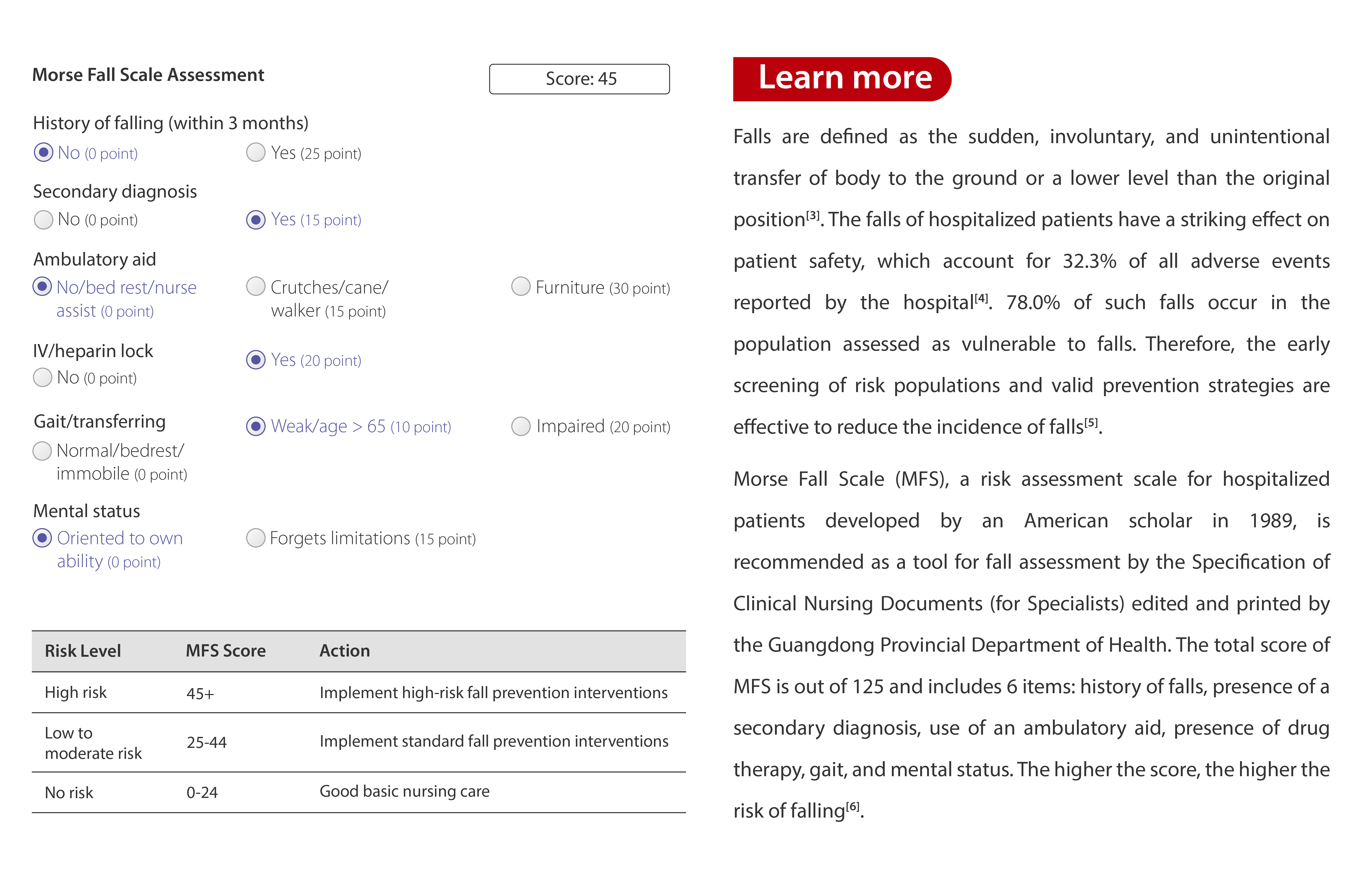
The patient was admitted to a general surgical ward and underwent conservative therapy, which was agreed upon by his family, given his advanced age and poor underlying condition. He was then treated with imipenem (intravenous drip) for anti-infection based on the bacterial culture results. Meanwhile, he was monitored by the mWear Wearable Patient Monitor as his Morse Fall Scale score was 45.
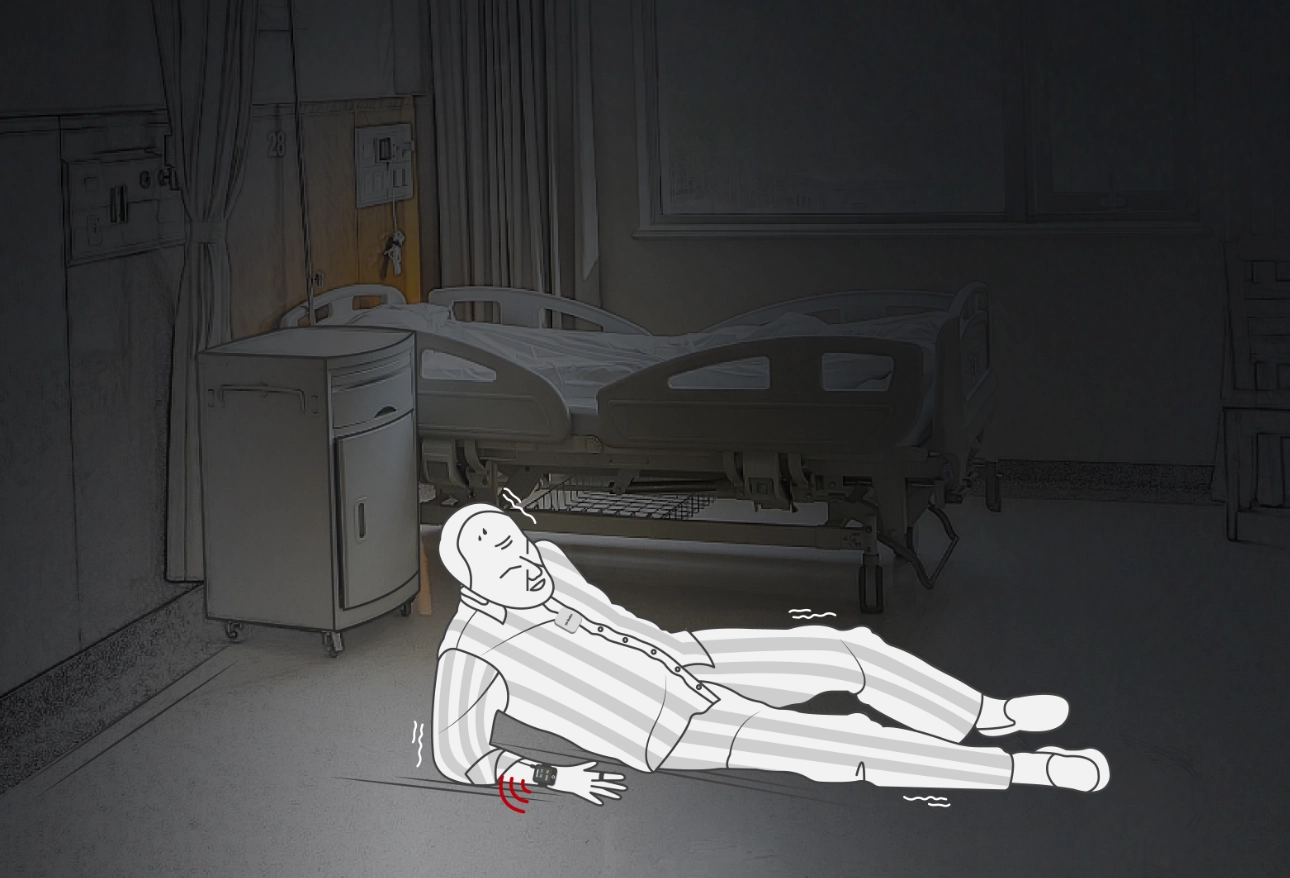
At 03:10 on Day 7 post-admission, the central monitoring system sounded an urgent alarm of falling down. A nurse went to the patient's bed immediately according to the displayed warning, and found the patient fell at the bedside. The patient did not call, the caregiver was asleep, and other patients and their families in the same ward did not hear any sound at all.
The nurse notified the on-call physician of the patient's fall, who performed examinations on the patient, including a lumbar spine AP and a left ankle AP & LAT X-rays. The physician provided first response to the minor fracture caused by the fall based on the exam results, preventing a potentially more serious outcome from occurring in time.
Note
The elderly patient himself was unable to explain exactly what happened before and after he fell out of bed that night when the clinician and the caregiver asked him afterwards. If the fall was not identified in time followed by instant treatments, it would be highly likely to have irreversible adverse consequences.
Case 2
Patient's profile
Female, 78-year-old, admitted due to the "numbness of lower extremities that persisted for over 6 years with aggravation for 3 months".
Medical history
Hypertension (over 30 years), diabetes (over 30 years), and balloon angioplasty in the left popliteal artery using a DSA + femoral artery stenting.
Post-hospitalization
The patient was monitored, after admission, by the mWear Wearable Patient Monitor for vital signs and health parameters, as his Morse Fall Scale score was 45.
At 17:30 on the day of admission, the central monitoring system displayed a warning of "Fall down". Then a nurse went to the ward and found the patient had fallen in the bathroom.
The patient recalled that she got out of bed to use the toilet on her own, without her family accompanying her. Not seeing clearly the position of the toilet, she fell into the gap between the toilet and the bathroom door, with buttocks on the ground and back leaned against the bathroom door.

Then, the nurse helped the patient up and informed the on-call physician, who performed the imaging and other related examinations on the patient. Fortunately, no positive results were caused because of falling down.
Summary
In addition to alarm warnings, it is more important to prevent patients from falling in clinical nursing, via the environment, education, and other means, including handrails and alarm buttons available everywhere in the ward. But many patients, as well as their families who accompany them, do not believe that they or the patients they are caring for will fall, until the first fall occurs.
Nevertheless, as illustrated in the two cases above, it is impossible to "predict" where a fall will occur, and elderly patients may not be able to call the health care providers or families for help on their own after a fall. Therefore, for the patients with a risk of falls after admission, mWear serves as another pair of eyes and another "body" of health care providers and patient's family members. It identifies patient status (fall down, exercise, rest, and sleep) by continuously monitoring, and notifies the health care providers via an alarm instantly after the fall occurs, in order to take corresponding measures as soon as possible to avoid adverse consequences to the greatest extent and safeguard patient's safety from all dimensions.

More Info

The mWear Wearable Patient Monitor's algorithm for fall detection is based on 2 modules. One is the ES30 module clipped to the patient's neckline, and the other is the EP30 module worn on the wrist.
For the former, the fall sign results from voting among three features, current posture, velocity, and acceleration, detected from the motion waveforms generated by the three-axis accelerometer. For the latter, the final fall status sign results from the intermediate fall result of the device combined with the marker of the physiological signal in place.
References
[1] World Health Organization (2012) Fact sheet 344: Falls. http://www.who.int/mediacentre/factsheets/fs344/en/. Accessed 6 June 2015.
[2] Clegg A. The frailty syndrome. Clin Med. 2011;11(1):72-5.
[3] Song Yalan, Zhang Lingling, Li Yuanfang, et al. Fall prevention bundle management strategy based on data analysis and its clinical practice among tumour inpatients. [J] Chinese Journal of Modern Nursing, 2018, 24(23): 2767-2772. doi: 10.3760/cma.j.issn.1674-2907.2018.23.009.
[4] Healey F , Scobie S , Oliver D ,et al. Falls in English and Welsh hospitals:a national observational study based on retrospective analysis of 12 months of patient safety incident reports[J]. Qual Saf Health Care, 2008,17(6):424-430. doi: 10.1136/qshc.2007.024695.
[5] Baek S , Piao JS , Jin YJ ,et al. Validity of the Morse Fall Scale implemented in an electronic medical record system[J]. J Clin Nurs, 2014,23(17-18):2434-2440. doi: 10.1111/jocn.12359.
[6] Pan Yue, Pang Lijia, Yao Yunshuang, et al. Occurrence of fall and its influencing factors in elderly patients with knee osteoarthritis. [J]. Chinese Journal of Modern Nursing, 2019, 25(26): 3417-3423. doi: 10.3760/cma.j.issn.1674-2907.2019.26.026.

