Ultrasound Journal 25 - Hepatocellular Carcinoma (HCC) in Non-Cirrhotic Liver Undergoing Right Hepatectomy Guided with Intraoperative Ultrasound
2024-05-22
Special thanks to Ismael Dominguez-Rosado MD,MSc for contributing the case.
Hepatic Pancreatic Biliary Surgeon/Researcher in medical sciences, Instituto Nacional de Nutrición Salvador Zubirán, México
Introduction
Hepatocellular Carcinoma (HCC) is a primary liver neoplasm, prevalent in patients with a history of liver cirrhosis. Although the treatment that confers the greatest chance of long-term survival is liver transplantation, surgical resection is an option in early stages and in patients with non-cirrhotic livers that may progress while waiting for a donor or who fail to meet transplant criteria despite strategies to achieve understaging. In situations where surgery is not initially possible, the use of systemic therapy to convert an unresectable disease into a resectable one is currently being explored. For this to be possible it is necessary to have a sufficient remaining liver that sometimes requires preoperative portal or suprahepatic venous deprivation procedures.
Medical History
This is a 67-year-old woman diagnosed with unresectable HCC in the non-cirrhotic liver. At the time of diagnosis, Barcelona A stage, with an 6 cm lesion confined to segments V, VI, VII and VIII, LIRADS 5, definitive for hepatocellular carcinoma with a liver remnant of less than 30%. Alpha fetus protein of 72.3 ng/ml. Negative viral hepatitis profile.
Systemic chemotherapy was started with the aim of reducing the size of the lesion and facilitating surgery with a greater possibility of negative margins and an adequate liver remnant, receiving 7 cycles of atezolizumab + bevacizumab. (Figure 1)

In preparation for surgery, right portal venous and suprahepatic vein deprivation were performed (Figure 2). After venous deprivation, there is an increase in liver remnant from 30% to 42%.

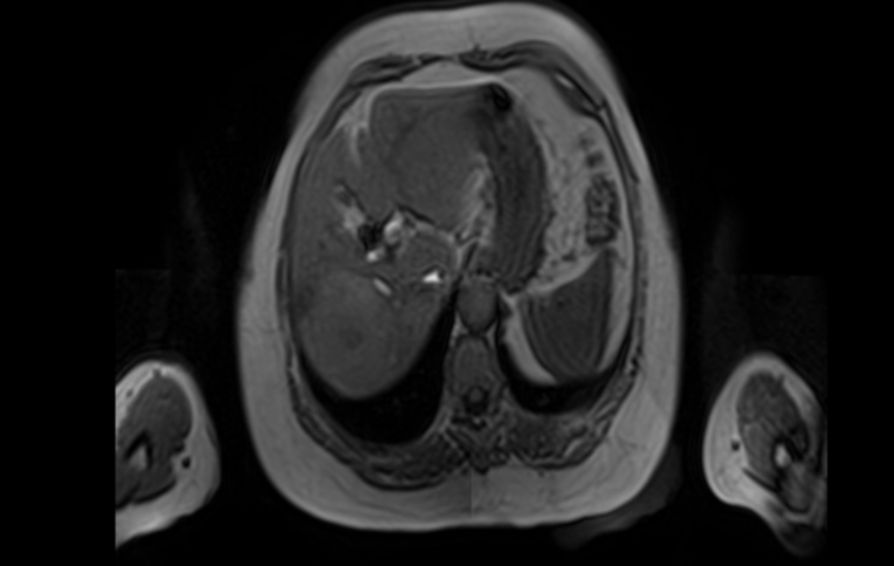
The patient underwent a right hepatectomy. In the transoperative period, we used intraoperative ultrasound with Mindray´s linear T-Shape probe 7LT4s ( Figure 3) and TE7 portable ultrasound system to mark the transection line just at the level of the middle suprahepatic vein, taking care to preserve the material used for suprahepatic venous deprivation (Figure 4 and 5).



We also use transoperative Doppler to evaluate an adequate Pringle maneuver, which consists of blocking arterial and portal flow transiently to facilitate liver transection and decrease intraoperative bleeding. (Figure 6)

The delimitation of the margin of ultrasound-guided transection allows to plan and visualize in advance the structures that must be preserved or cut, making a safer procedure. (Figure 7)

Disccusion
Currently, the use of atezolizumab and bevacizumab in patients with advanced HCC has shown a significant impact on overall survival as demonstrated by the phase 3 IMbrave 150 clinical trial. [1] Its use in unresectable advanced HCC is standard of care, but there is still no strong evidence on its benefit as a preoperative treatment. [2.3]
Surgical resection, particularly when venous deprivation material is present, is facilitated by the use of intraoperative ultrasound. Ultrasound allows you to locate key anatomical points, such as the middle suprahepatic vein that delimits the transection zone of a right hepatectomy. Although its use is common in certain regions of the world such as Japan and Italy since the late twentieth century, its application has not been widespread elsewhere where liver surgery is still in its infancy. [4]
Dr. Torzilli has developed multiple liver resection techniques, where the use of intraoperative ultrasound plays a fundamental role in intraoperative planning and decision making. [5] As in this case, where intraoperative ultrasound allows to locate the amplatzer and plan a liver transection where this venous deprivation material is preserved.
Conclusion
Intraoperative ultrasound is a fundamental tool for the liver surgeon that allows both diagnosing unknown lesions during the procedure, as well as planning liver transection, defining peritumoral surgical margins and performing anatomical resections of one or more liver segments. Likewise, it allows to evaluate the suitability of a Pringle maneuver and the permeability of the portal, arterial and suprahepatic vasculature in situations where they are reconstructed. It is an indispensable tool whose use should be widely disseminated.
References
[1]. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, Li D, Verret W, Xu DZ, Hernandez S, Liu J, Huang C, Mulla S, Wang Y, Lim HY, Zhu AX, Cheng AL; IMbrave150 Investigators. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020 May 14;382(20):1894-1905. doi: 10.1056/NEJMoa1915745. PMID: 32402160.
[2]. Chamseddine S, LaPelusa M, Kaseb AO. Systemic Neoadjuvant and Adjuvant Therapies in the Management of Hepatocellular Carcinoma-A Narrative Review. Cancers (Basel). 2023 Jul 5;15(13):3508. doi: 10.3390/cancers15133508. PMID: 37444618; PMCID: PMC10340217.
[3]. Hagiwara S, Nishida N, Kudo M. Advances in Immunotherapy for Hepatocellular Carcinoma. Cancers (Basel). 2023 Mar 30;15(7):2070. doi: 10.3390/cancers15072070. PMID: 37046727; PMCID: PMC10093619.
[4]. Joo I. The role of intraoperative ultrasonography in the diagnosis and management of focal hepatic lesions. Ultrasonography. 2015 Oct;34(4):246-57. doi: 10.14366/usg.15014. Epub 2015 Apr 6. PMID: 25971896; PMCID: PMC4603208.
[5]. Donadon M, Torzilli G. Intraoperative ultrasound in patients with hepatocellular carcinoma: from daily practice to future trends. Liver Cancer. 2013 Jan;2(1):16-24. doi: 10.1159/000346421. PMID: 24159592; PMCID: PMC3747551.
