In Mindray’s Case Observation section, you will find “comrades in arms” who encounter similar problems with you; hear different fresh diagnosis and treatment ideas and solutions; learn more comprehensive and intelligent monitoring methods and analysis methods; find more efficient and applicable clinical decision-making experience.
Assisting the Oxygenation Management of Critically Ill Neonates with Blood Oxygen Level Chart
Case Introduction
The premature was given birth by a woman with gravida 9 para 3 by vaginal delivery at a gestational age of 33 weeks after 6.4 hours of premature rupture of membranes. The premature’s birth weight was 2.2 kg, and his/her Apgar score was 9 points at 1 min and 10 points at 5 min and 10 min, respectively.
Physical examination after admission for NICU
Low-flow oxygen therapy was given in the incubator, SPO fluctuated between 90-94% and occasionally decreased to 86%. No shortness of breath, cyanosis, and apnea were observed. Moderate yellowing of the skin was observed. The bregma was flat and soft, and smooth breathing was observed. The three retraction signs were negative. Coarse breath sounds were heard in both lungs, and no dry or moist rales were heard. Normal heart rhythm and strong heart sounds were detected, and no pathological murmurs were heard. The liver was 2.5 cm below the costal margin, and its texture was soft. The spleen was palpable at the umbilicus level. The bowel sounds were normal, and the muscle strength and tone of the four limbs were satisfactory.
Results of the first auxiliary examination after admission for the premature
Hematology test:
WBC 70.13 *109/L↑, HGB 163g/L, HCT 47.6%, PLT 249*109/L, CRP 2.22mg/dL↑.
Doppler ultrasound of the heart showed:
left-to-right shunt at the atrial septum level, and no significantly abnormal echogenicity was observed in the transcranial Doppler ultrasound A chest radiography showed patchy shadows in the right lung field, and the shadows were increased as compared to before.
Diagnosis
Preliminary Diagnosis:
1. Premature infant, low birth weight infant;
2. Neonatal pneumonia (intrauterine infection).
Supplementary Diagnosis:
1. Neonatal sepsis (long duration of premature rupture of membranes, significantly increased neutrophil percentage and CRP, positive for UU and vaginal GBS);
2. Neonatal premature-related jaundice;
3. Cytomegalovirus infection;
4. Cephalohematoma (a palpable mass in the parietal region);
5. Cytomegalovirus infection.
Summary of Early Treatment
For anti-infective therapy, the patient was switched from ceftazidime to azithromycin + piperacillin/tazobactam for combination anti-infective therapy. Due to the occasional decrease in oxygen saturation, the premature was switched from low-flow oxygen therapy to high-flow oxygen therapy via the nasal cannula, and the premature’s condition improved thereafter. Subsequently, the premature was switched to spontaneous breathing, and was moved from the incubator to the rescue table.
Disease Progression
From Day 17 of hospitalization, the premature experienced frequent decline in blood oxygen level. A physical examination revealed hepatosplenomegaly, and a hematology test suggested thrombocytopenia and a slight decrease in hemoglobin level. A serum specific antibody testing showed: CMV-IgG antibody was 34.1 U/ml, and CMV-IgM antibody was 40.3 U/ml. The diagnosis of cytomegalovirus infection was confirmed.
The mortality rate of cytomegalovirus infection in premature infants is high (the case fatality rate can reach 30%), and pneumonia accompanied by respiratory failure is the main cause of death. Therefore, in addition to antiviral and symptomatic treatment, it is necessary to pay close attention to blood oxygen and respiratory status.
Brief description of oxygen therapy process
During the antiviral and anti-infective treatment (i.e., Days 17-29 of hospitalization), different methods of oxygen therapy were used according to the premature’s blood oxygen status (with the help of the SPO function of Mindray monitor) (Figure 1).
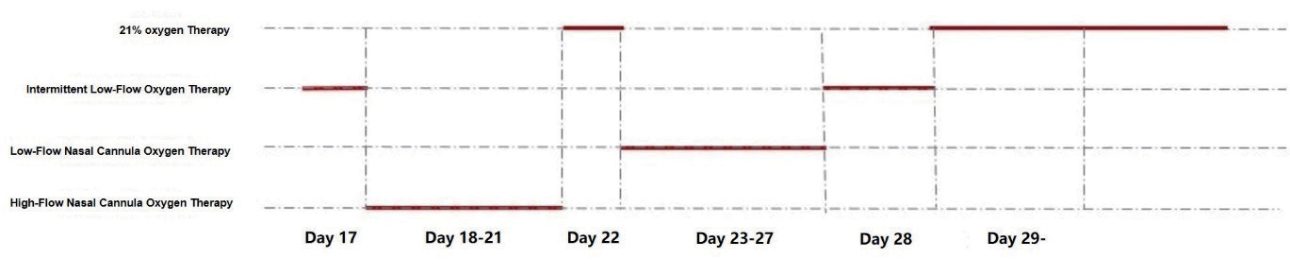
Selection of method of oxygen therapy with assistance of blood oxygen statistics monitoring function
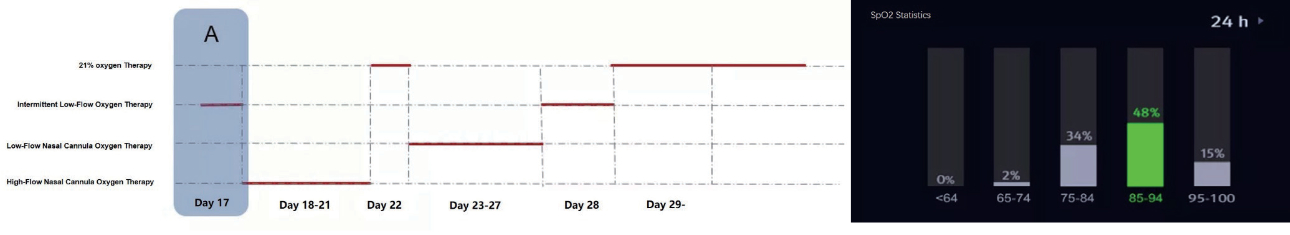
(As shown in Figure 2-A above) Due to the sudden and frequent decrease in oxygen saturation when the premature was in the spontaneous breathing state, the premature was switched to intermittent low-flow oxygen therapy directly. It can be seen from the blood oxygen statistics function: In the past 24 h, 34% of the SPO was within the range of 75%-84%, and 2% of the SPO was within the range of 65-74%. Even if oxygen therapy was provided, it was still insufficient to support the normal oxygen demand of the premature.
(As shown in Figure 2-B above) As intermit- tent low-flow oxygen therapy still could not meet the oxygen demand of the premature on Day 18 of hospitalization, so the prema- ture was switched to high-flow nasal cannula oxygen therapy (the maximum inhaled oxygen concentration was 30%), and other supportive treatments such as drugs were also given. Until Day 21 of hospitalization, his/her blood oxygen level could be maintained between 91-95%, and his/her oxygenation status improved significantly, indicating the treatment is effective.
On Day 21, another analysis was performed using the blood oxygen statistics function: In the past 24 hours, 48% of the blood oxygen levels exceeded the control target, which was within the range of 96%-100%. In order to prevent the secondary risks of BPD and ROP when the premature is exposed to high-concentration oxygen therapy for a long time, the method of oxygen therapy must be adjusted again.
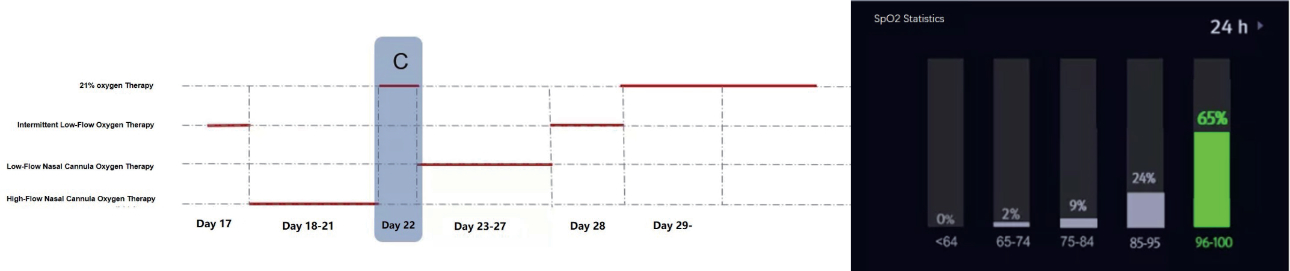
(As shown in Figure 2-C above) As the premature’s condition improved, so the first attempt to remove the cannula was made on Day 22, and the premature was allowed to breath spontaneously, and the oxygenation target was changed to 96%-100%. An analysis was performed by using the blood oxygen statistics function: After changing the high-flow nasal cannula oxygen therapy to spontaneous breathing for 24 hours, there is an unstable decrease in blood oxygen level. In 35% of the time, the blood oxygen level was less than 96% (2% was within the SPO2 range of 65%-74%, 9% was within the SPO2 range of 75%-84%, 24% was within the SPO2 range of 85%-95%), indicating that it was insufficient to support the normal physiologi- cal needs of the premature. Hence, the attempt to remove the cannula failed.
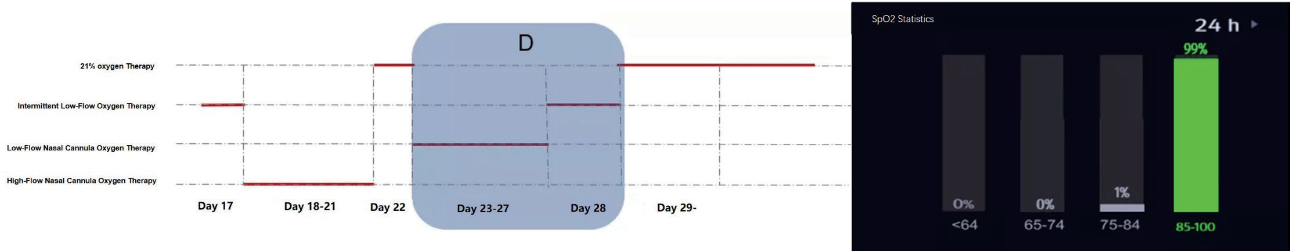
(As shown in Figure 2-D above) Therefore, the oxygen withdrawal training regimen was re-customized for the premature, and intermittent oxygen therapy was used (gradually switched from low-flow oxygen therapy to intermittent low-flow oxygen therapy until the premature was able to breath spontaneously). During the 6 days of training, the blood oxygen statistics function can be combined with intermittent oxygen withdrawal training to present the daily training results. As shown in the figure above, after stepping down to intermittent low-flow oxygen therapy on Day 28, it can be clearly seen that the premature’s blood oxygen level was within 88-100% for 99% of the time within 24 hours, indicating that the oxygen withdrawal training is effective.
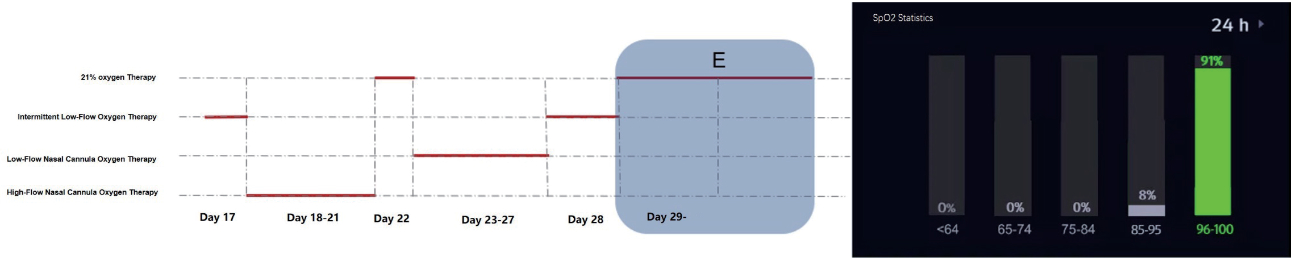
(As shown in Figure 2-E above) On Day 29 of hospitalization, the premature continued the stepped-down to spontaneous breathing. Through the blood oxygen level chart, it was found that the premature could maintain normal oxygenation in the spontaneous breathing state (24h statistics, 91% of the blood oxygen levels was maintained between 96-100%), which proves that the current can- nula removal is successful.
Summary
There is a relatively large proportion of premature infants in the NICU. Due to incomplete development of the prematures’ lungs, central sleep apnea and other reasons, inadequate oxygenation in premature infants is common in clinical practice. For example, the status of cytomegalovirus infection in this case, oxygenation support and other methods need to be used to avoid long-term hypoxia in the premature, but it is also necessary to avoid complications such as BPD and ROP induced by excessive use of oxygen.
Neonatologists need to use the blood oxygen results as feedback to perform the precise assessment and management of oxygenation in order to avoid the above problems.
However, most of the assessment of the overall status of prematures’ blood oxygen can only rely on the nurse’s daily regular and timely recording, oral communication, and review of the blood oxygen trend recorded in the monitoring device, which bring about problems such as incomplete data, subjective bias, difficulty in obtaining accurate statistics, etc. Therefore, how to obtain the overall status of blood oxygen monitoring efficiently and easily is currently a challenge in clinical practice.
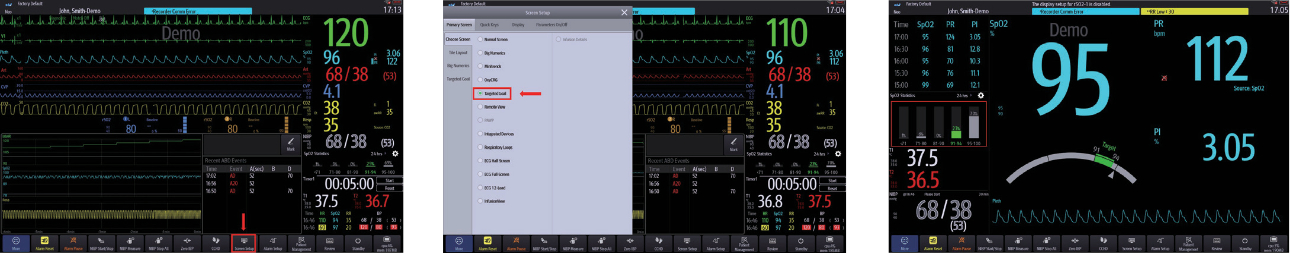
The blood oxygen target chart on Mindray monitor can customize the blood oxygen interval (customized blood oxygen target and segment) and time period (30 min-24 h), which can intuitively and quantitatively display the blood oxygen distribution and the proportion of blood oxygen levels achieving the target. Apart from solving the above clinical problems, it enables the oxygenation management of critically ill neonates in NICU to be “performed more effortlessly”. (The steps are as follows: Main Menu Bar Interface Settings-Target Monitoring-SPO2 tatistics)