People generally think of surgery as a swift and, hopefully, seamless endeavor. However, to ensure the safety of the patient and effectiveness of the procedure, the tasks performed in the operating room (OR) require collaboration pre-, intra- and post-operatively across multiple teams.
How can we enhance patient safety through anesthesia in the operating room?
The risk of perioperative severe complications is easy to overlook when balancing surgical pathways, resulting in increased morbidity and mortality. This is an opportunity for anesthesiologists to play an integral part in the maintenance of patient safety.
Induction
Pre-oxygenation using a high fraction of inspired oxygen (FIO2) is a critical step before induction of anesthesia and tracheal intubation, as it creates an oxygen reservoir in the lungs. This delays the onset of arterial hemoglobin desaturation during apnea. Despite the fact that pre-oxygenation is advised for intubation, inadequate pre-oxygenation was observed in approximately 56% of patients[1].
The oxygen reserve diminishes particularly in high-risk patients, so various strategies such as continuous positive airway pressure (CPAP) and high flow nasal cannula (HFNC) may be used to increase its effectiveness[1,2]. In addition to integrated monitoring of SpO2, new clinical applications like CPAP and HFNC can be very helpful to achieve maximum pre-oxygenation for obese patients, critically ill patients, or patients with a difficult airway.
Maintenance
During general anesthesia inhalation, real-time guidance on fresh gas flow is offered by a fresh gas flow visualization tool – the Optimizer – on Mindray’s anesthesia machines, resulting in reduced anesthetic consumption and a safe low fresh gas flow. Another visualization feature, AA Prediction, allows anesthesiologists to predict anesthetic status (including FiAA and EtAA) and oxygen concentration (including FiO2 and EtO2) for the next 20 minutes.
As medical technologies advance, an automatic controlled anesthesia tool that can automatically adjust the fresh gas and vaporizer output is strongly recommended to enhance the stability and safety of anesthesia while relieving the work of anesthesiologists.
It is also necessary to check on the balance of anesthesia in real time. A graphic ‘anesthesia triangle’ that indicates patient’s status of sedation, paralysis, and analgesia is enabled on the BoA Dashboard in Mindray’s advanced BeneVision N Series patient monitors. There are many more features that can be used to ensure patient safety during the entire peri-operation.
Recovery
After surgery, patients are at risk of developing postoperative pulmonary complications (PPCs) that are strongly related to surgery and anesthesia. This can lead to serious side effects and longer hospital stays[3]. Approximately 5% of patients who undergo general surgery develop PPCs. This figure increases to almost 30% among obese patients or patients who undergo cardiac or thoracic surgeries[4]. Luckily, in recent studies, research has shown that the following criteria help to reduce the rate of PPCs[5,6,7]:
- Ventilation with lower tidal volume or lower driving pressure
- Appropriate levels of positive end-expiratory pressure (PEEP) that prevent alveolar collapse at end-expiration
- Lung recruitment maneuvers that re-expand the collapsed lung alveoli
With Mindray’s perioperative lung-protective ventilation solution, a suitable PEEP level along with secure consistent tidal volume work to meet individual patient’s needs and minimize the incidence of PPCs. Lung recruitment outcomes can be evaluated through respiratory mechanics using anesthesia machines and tracking oxygenation (SpO2 or PaCO2) via patient monitors.
Are anesthesiologists at risk too?
While patient safety is of utmost importance, the safety of medical staff may be at risk too. With ever-growing workloads, health care professionals are particularly at risk of burnout. In a recent systematic review, 67% of physicians reported burnout[8]. Another systematic review showed the highest percentage of burnouts occurred in critical care and emergency medicine physicians (55%), closely followed by anesthesiologists (50%)[9]. Although burnout is multifactorial, it develops in response to long working hours in high-risk and complex work settings involving multidisciplinary teams.
Better patient outcomes with less physician time and effort may be achieved with an informed and streamlined workflow utilized in intraoperative care. User-friendly interfaces, easy-to-read screens and a set of visualization tools can be helpful. Mindray anesthesia machines, especially the A7, have constantly been recognized for providing a good user experience. The A7 received a ‘Good’ rating in workflow, interoperability, and user experience by the ECRI evaluation[10].
In addition to these, Mindray offers a comprehensive data integration system that standardizes patient data monitoring for effective decision-making. Seamless data transfer from patient admission to discharge is now possible to automatically upload data to the central monitoring system and the hospital’s multiple IT systems to simplify time-consuming activities.
Anesthesia machines can be interfaced with patient monitors. A series of clinical assistive applications are integrated into Mindray’s patient monitoring system to visualize multiple clinical parameters, allowing clinicians to read, diagnose, and intervene easily, enabling a less stressful work environment.
What is a “green” operating room?
Healthcare practitioners can be exposed to anesthetic gases released during medical procedures. These gases are known as waste anesthetic gases (WAGs). Not only do WAGs risk surgical staff and patient safety, they also contribute to anthropogenic climate changes. As only 5% of anesthetics are metabolized by patients, the rest is routinely vented to the atmosphere through the OR scavenging system. It has been shown that the global warming potential of a halogenated anesthetic is up to 2,000 times greater than CO2[11,12].
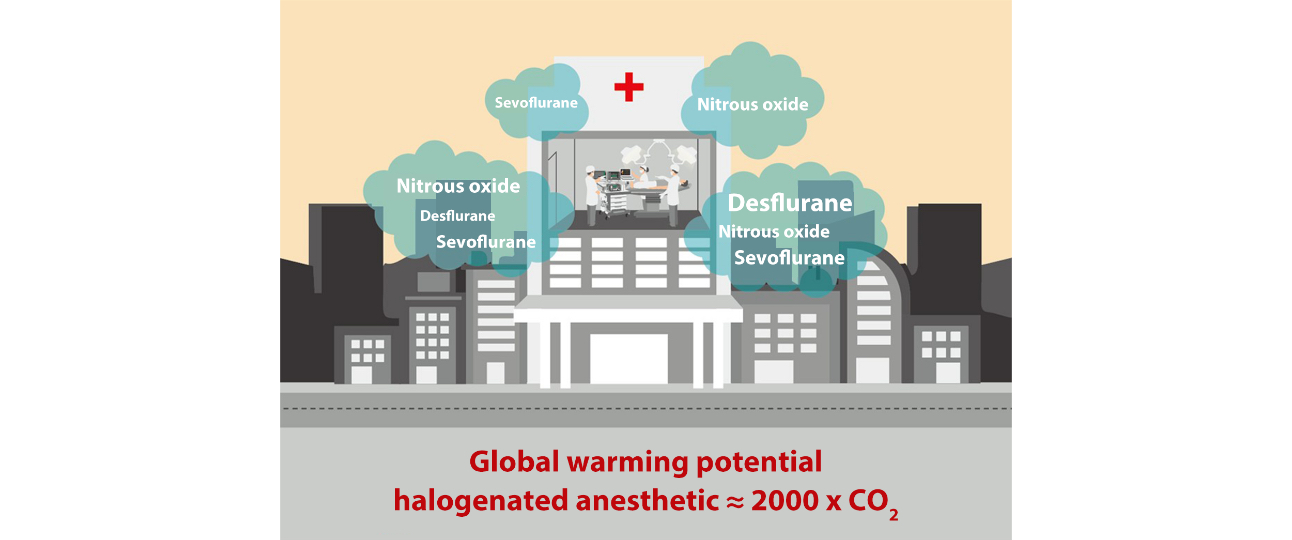
Exposure to chronic halogenated anesthetics is linked with adverse reproductive effects and cancer. Exposure to nitrous oxide can cause light-headedness, shortness of breath, reduced fertility, and spontaneous abortion, as well as renal, liver, and neurogenic diseases[13].
Mindray attempts to prevent OR staff from being exposed to unnecessary anesthesia leaks through the flow pause function in anesthesia machines, designed to temporarily discontinue the fresh gas flow. In a safety advancement, Mindray’s anesthesia machines offer the option to reuse sample gases taken from the anesthetic gas monitoring module by making them return to the circuit. Exposure is further reduced by optimizing an efficient anesthetic gas scavenging system (AGSS) designed to vent WAGs out of the surgical environment.
Read more on: What’s an anesthesia machine got to do with… glacier melting?
Keeping safety as the primary goal, Mindray adopts a path of technological advancement with a multifaceted approach towards achieving all-round safety. We seek to fulfill safe breakthroughs in a cost-effective manner for hospitals to achieve a healthier perioperative environment for patients, medical staff, and the environment.
In the upcoming new generation of Mindray A Series anesthesia machine, many new features and upgrades will be unveiled.
Reference:
[1] C. Baillard, F. Depret, V. Levy et al. Incidence and prediction of inadequate preoxygenation before induction of anaesthesia. Annales Françaises d'Anesthésie et de Réanimation Volume 33, Issue 4, April 2014, Pages 55-58.
[2] Nimmagadda U, Salem M. R, Crystal G J. Preoxygenation: Physiologic Basis, Benefits, and Potential Risks. Anesthesia & Analgesia: February 2017 - Volume 124 - Issue 2 - p 507-517.
[3] Miskovic, A. B. Lumb. Postoperative pulmonary complications. British Journal of Anaesthesia, Volume 118, Issue 3, March 2017, Pages 317–334.
[4] Canet J, Gallart L, Gomar C et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010 Dec;113(6):1338-50.
[5] Marret E, Cinotti R, Berard L et al. Protective ventilation during anaesthesia reduces major postoperative complications after lung cancer surgery. European Journal of Anaesthesiology. October 2018 - Volume 35 - Issue 10 - p 727–735.
[6] Futier E, Protective lung ventilation in operating room: A systematic review. Minerva Anestesiol 2014; 80:726–35.
[7] Alcino C L, Ludhmila A H, Marcia S. V et al. Effect of Intensive vs Moderate Alveolar Recruitment Strategies Added to Lung-Protective Ventilation on Postoperative Pulmonary Complications A Randomized Clinical Trial. JAMA. doi:10.1001/jama.2017.2297 Published online March 21, 2017.
[8] Rotenstein LS, Torre M, Ramos MA. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA. 2018 Sep 18;320(11):1131-1150.
[9] Sanfilippo F, Noto A, Foresta G. Incidence and Factors Associated with Burnout in Anesthesiology: A Systematic Review. Biesia unit. Health Devices. 2017 Feb 22.
[11] Ryan, S. M., & Nielsen, C. J. (2010). Global warming potential of inhaled anesthoMed Research International. Volume 2017. Article ID 8648925.
[10] ECRI Institute. Evaluation: Mindray Medical International A7 general-purpose anesthetics: application to clinical use. Anesthesia & Analgesia, 111(1), 92-98.
[12] Gadani H, Vyas A. Anesthetic gases and global warming: Potentials, prevention and future of anesthesia. Anesth Essays Res. 2011 Jan-Jun; 5(1): 5–10.
[13] NIOSH: Chemical Hazards: Health and Safety Practices Survey of Healthcare Workers.